In recent years, endothelial transplant methods have replaced penetrating keratoplasty for the treatment of Fuchs’ endothelial dystrophy, and several new transplant techniques are currently in the pipeline. The hope is that these new techniques will have a global impact. “In the United States, we’re very fortunate. We have an excellent eye banking system; we don’t have tissue shortages. The rest of the world is a different story,” says Kathryn Colby, MD, PhD, the Elisabeth J. Cohen Professor and Chairman of the Department of Ophthalmology at the NYU Grossman School of Medicine.
Sioux Falls, South Dakota’s John Berdahl, MD, agrees, noting that the unmet need for endothelial cell transplants across the globe is enormous. “The United States has a healthy system of eye banks. Our limiting factor is the number of cornea transplant surgeons that we have. The problem abroad is that we don’t have enough tissue to cover all the needs. What’s exciting about these techniques is they don’t have to be one-to-one, meaning one corneal donor to one recipient. They can be manufactured corneas, manufactured drugs, or based on cell therapy cultures where one cornea could turn into hundreds or even thousands of corneal transplants. So, it allows the therapy to be delivered at scale and to provide for the global need for endothelial cell transplantation. Additionally, the surgical technique is not as delicate and specialized, so this should open the pathway for more surgeons to be able to perform these techniques,” says Dr. Berdahl.
Dr. Colby adds that these new techniques would provide more specific treatments. “Now, we do endothelial keratoplasty instead of a full-thickness penetrating keratoplasty, which is what we did for Fuchs’ in the 90s. It’s great if we can do a less invasive, less extensive type of surgery that is less resource intensive. You can imagine that we might be able to develop a medication that prevents the endothelial cells from degenerating and prevents the need for any kind of surgical intervention. The advantage of the cultured cells is that they can potentially be used in the developing world where there are tissue shortages. And if you had a cell suspension, it would probably be easier to transport if you were going internationally,” she adds.
The new techniques fall into three categories. “First, there are cultured endothelial cells. Several companies are working on that. There’s a company looking at basically an artificial endothelial layer that just acts as a barrier, and a number of companies are looking at medications that may enhance the success of Descemet’s stripping only, which is where we just remove the central endothelium and let the peripheral host endothelium repopulate the central cornea. Those are the three major buckets,” Dr. Colby says.
She adds that companies overseas are developing techniques. “There’s a lot of interest in the disease. It’s a very common condition. In fact, up to 4 percent of people in the United States have a mild form of it. Fewer need any intervention, but it tells us a lot about the biology of the cornea, which is also very interesting,” she says.
 |
|
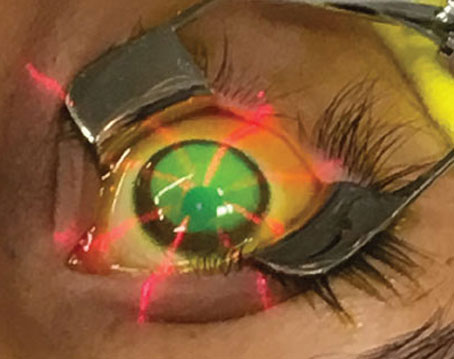
The initial part of the Descemet’s Stripping Only procedure. Also seen is the pre-existing anterior capsulorhexis opening (left). The completed DSO procedure and the surgically detached disc of Descemet’s membrane with compromised endothelial cells (right). The pre-existing capsulorhexis opening is also visible. Photo: Mark A. Terry, MD. |
Cultured Endothelial Cells
Two new techniques being evaluated by Aurion and Emmecell fall into this category. According to Francis Mah, MD, who is in practice in La Jolla, California, Aurion’s technology is ex vivo expansion of endothelial cells. “They take donor cells and expand them in culture. Then, investigators inject the donor cells into Fuchs’ dystrophy patients who need a corneal transplant. Some positioning is needed. The patients need to lie face down so that the endothelial cells can attach to the posterior cornea,” he says.
Dr. Mah explains that this technique started with Shigeru Kinoshita in Japan, who did groundbreaking research developing it. He performed an uncontrolled, single-group study involving 11 patients who were diagnosed with bullous keratopathy and had no detectable corneal endothelial cells.1 Human corneal endothelial cells were cultured from a donor cornea. A total of 1×106 passaged cells (passenging refers to the removal of the medium and transfer of cells from a previous culture into fresh growth medium) were supplemented with a rho kinase (ROCK) inhibitor and were injected into the anterior chamber of the eye that was selected for treatment. After the procedure, patients were placed in a prone position for three hours. At 24 weeks after the cell injection, the researchers recorded a corneal endothelial cell density of more than 500 cells per mm2 in all 11 treated eyes and more than 1,000 cells per mm2 in 10 of the 11 treated eyes.
“This technology was purchased by Aurion in the U.S.,” Dr. Mah explains, “and they’ve done preclinical as well as the Phase II studies outside Japan. Now, they are doing a five-arm FDA trial. There are some specifics regarding why it needs to be a five-arm study. The technique that Kinoshita described used a ROCK inhibitor that is not currently FDA-approved in the United States. So, they’re studying this technique with and without the ROCK inhibitor. It’s pretty landmark stuff.”
The second technique is Emmecell, which is similar. “Emmecell is unique in that, while it is also ex vivo expansion of endothelial cells, it uses nanoparticle magnets that are inserted into the cells in a proprietary fashion,” says Dr. Mah. “They don’t harm the cells at all. This company has also done an FDA clinical trial. As previously mentioned with the Aurion technology, the cells are injected into the anterior chamber. The patient then needs to look down at the floor, and just through gravitation, the cells are going to kind of float down and attach to the stroma. The patient needs at least two hours—maybe longer—in the face-down position. In the beginning, the Aurion technique required days face down. The endothelial cells with nano-magnets in the Emmecell technology tries to improve on the patient post-cell injection positioning. Patients must wear a magnetic facemask, kind of like a sleep mask with magnets. So, the positioning for the patients becomes a much easier proposition. The patients wear goggles with the magnets, and the magnets actually pull the endothelial cells to the posterior stroma to attach. It helps solve one of the potential downsides of the Aurion technology.”
He notes that Emmecell doesn’t use a ROCK inhibitor, which is another potential advantage. “The Emmecell technology with the magnets just helps attach the cells to the posterior stroma. The Kinoshita technology, Aurion’s technology, is FDA-approved in Japan, so they already have a lot of regulatory data and information available for that technology. So, they’re a little further along in terms of the regulatory pathway than Emmecell. But, at least in the United States, both have completed a Phase I clinical trial,” he explains.
According to Dr. Mah, one of the advantages of Aurion and Emmecell is that they’re injectable, so the procedure could potentially be performed in the office. “There is a small incision with DSEK, DMEK and DSO, but this would be even smaller, potentially, so it would be even safer. Additionally, while it may be initially cost-prohibitive, the costs will come down, and the technology will be able to be used by others where eye banking or corneal transplantation isn’t readily available due to lack of tissue or surgeons. This might be a way to treat corneal blindness in areas that need corneal transplantation,” he adds.
Another potential benefit is that the rates of rejection could possibly be minimal to none. “Right now, those two technologies really seem to work best in Fuchs’ patients, but you might imagine where the technology grows as we learn more about those two technologies, such that we can do other patients who need corneal transplantation due to any endothelial decompensation, not just Fuchs’ patients,” Dr. Mah says.
 |
|
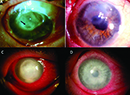
A slit lamp photo (left) and its corresponding endothelial image from a DSO patient. Photo: Kathryn Colby, MD. |
Artificial Endothelial Cell Layer
EndoArt corneal artificial endothelial layer (EyeYon Medical) is the first synthetic implant to treat corneal edema. It attaches to the back of the corneal surface, preventing the transfer of fluids into the cornea and inhibiting the build-up of fluid. The procedure is performed through small incisions.
“EyeYon is an Israeli company, and EndoArt has been used outside of the United States in well over 100 cases,” Dr. Mah explains. “Essentially, it’s like a contact lens. The surgeon makes an incision just like for DSEK or a DMEK and implants EndoArt after removal of the Descemet’s membrane. It has a certain base curve that should shape to the posterior cornea. So, there is a possibility that you could implant it upside down, but they’ve got little markings on it to prevent this complication. You place an air bubble in the eye, and you place a suture through the superior part of the cornea and implant to help with attachment. Basically, the endothelial cells pump fluid out of the stroma and the cornea. This technology prevents fluid from getting into the stroma, so it helps prevent the swelling that lack of endothelial cells produces.”
The company has had to adjust the size of the implant. “They started with a larger size in preclinical and early clinical studies and found that it actually prevented too much fluid from going into the cornea. It also prevented some of the nutrients from the aqueous from entering the cornea. So, they made the implant a little smaller so that nutrients and some amount of fluid can get into the cornea. And now they’re going through the United States’ regulatory process to see if they can get this FDA-approved here,” Dr. Mah adds.
The EyeYon technology wouldn’t require the use of long-term steroids because there’s no chance of rejection. “You would need a short course of steroids in the beginning, probably less than six months,” Dr. Mah adds. “And because there is no corneal tissue, again, this would be very easily used in countries where there’s a lack of eye banking or the infrastructure for corneal tissue is not as robust. This technology may not replace first-line DSEKs and DMEKs, especially, for example, in the United States, but it would give another option for patients who have run out of other options due to their immune system and rejection or other issues with the eye.”
A recent case report found that “this new device could serve as an alternative to lamellar endothelial corneal transplantation in cases where tissue rejection has occurred and is highly likely to recur. The technique is simple, and the deswelling effect on the cornea persisted, although the visual results require further validation in patients with a higher visual potential.”2
The patient in this case study presented with pseudophakic bullous keratoplasty after a history of two rejected PKs and one rejected Descemet’s stripping automated keratoplasty. An artificial endothelial layer was implanted and remained fully attached for a follow-up period of 12 months.
Medications to Enhance DSO
Multiple companies are currently studying medications to facilitate DSO healing. CoA is investigating ripasudil for this purpose, and Dr. Colby is the chair of the study. “We’ve completed the Phase II study, which was positive, and now we are in Phase III trials,” she says. “One of them has virtually completed enrollment; we’re not accepting any more people for screening. And the other one is about three-quarters enrolled. So, we expect to have results within the next year or so. That’s probably the furthest along of the medical treatments. Another company, Trefoil, is looking at a bioengineered fibroblastic growth factor. Additionally, a company called Design Therapeutics is developing a small molecule to inhibit transcription of the repeat expansion that underlies most of Fuchs’ in the United States. Right now, they’re doing a natural history study to try to determine the best biomarker for when they have the product that they can use in patients with Fuchs’ endothelial dystrophy.”
Dr. Berdahl has a financial interest in Aurion, CorneaGen, Dakota Lions Sight & Health. Dr. Colby has no financial interests to disclose. Dr. Mah is a consultant to EyeYon.
1. Kinoshita S, Koizumi N, Ueno M, et al. Injection of cultured cells with a ROCK inhibitor for bullous keratopathy. N Engl J Med 2018;378:995-1003.
2. Rens J, Krolo I, Koppen C, et al. Artificial endothelial layer implantation after multiple failed keratoplasties. Cornea 2024;43:6:790-794.