Photorefractive keratectomy received approval by the U.S. Food and Drug Administration in 1996, and quickly rose in popularity over incisional radial keratotomy. However, compared to LASIK, PRK remains a less popular procedure choice for primary refraction correction and represents about 10 to 15 percent of all laser refractive procedures performed in the United States.1 That said, due to its unique advantages, PRK may be preferable in certain situations, and the procedure will continue to play an important role in refractive surgery. Here, we discuss the PRK procedure in further detail, including its indications as well as how to avoid and manage complications.
Indications and Preoperative Considerations
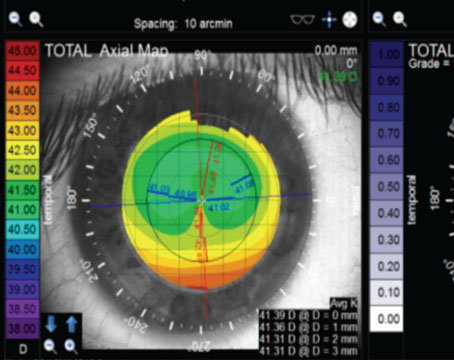
Despite an association with more postoperative discomfort and a slower healing time than LASIK,2 PRK can be the preferred refractive surgery in several instances. For patients who are considered suboptimal candidates for LASIK, PRK may be an option. This includes patients with thinner corneas, especially since a residual stromal bed of at least 250 µm is generally recommended with LASIK.3-5 Certain eyes are deemed to be at higher risk for post-LASIK ectasia, based on tomographical findings and its derived indices.6,7
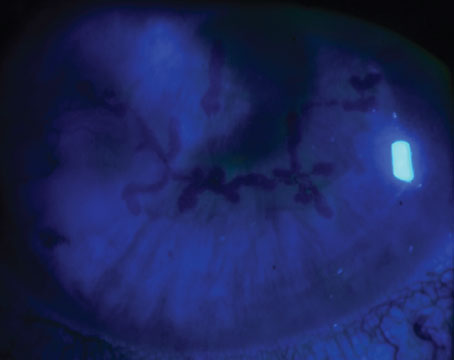
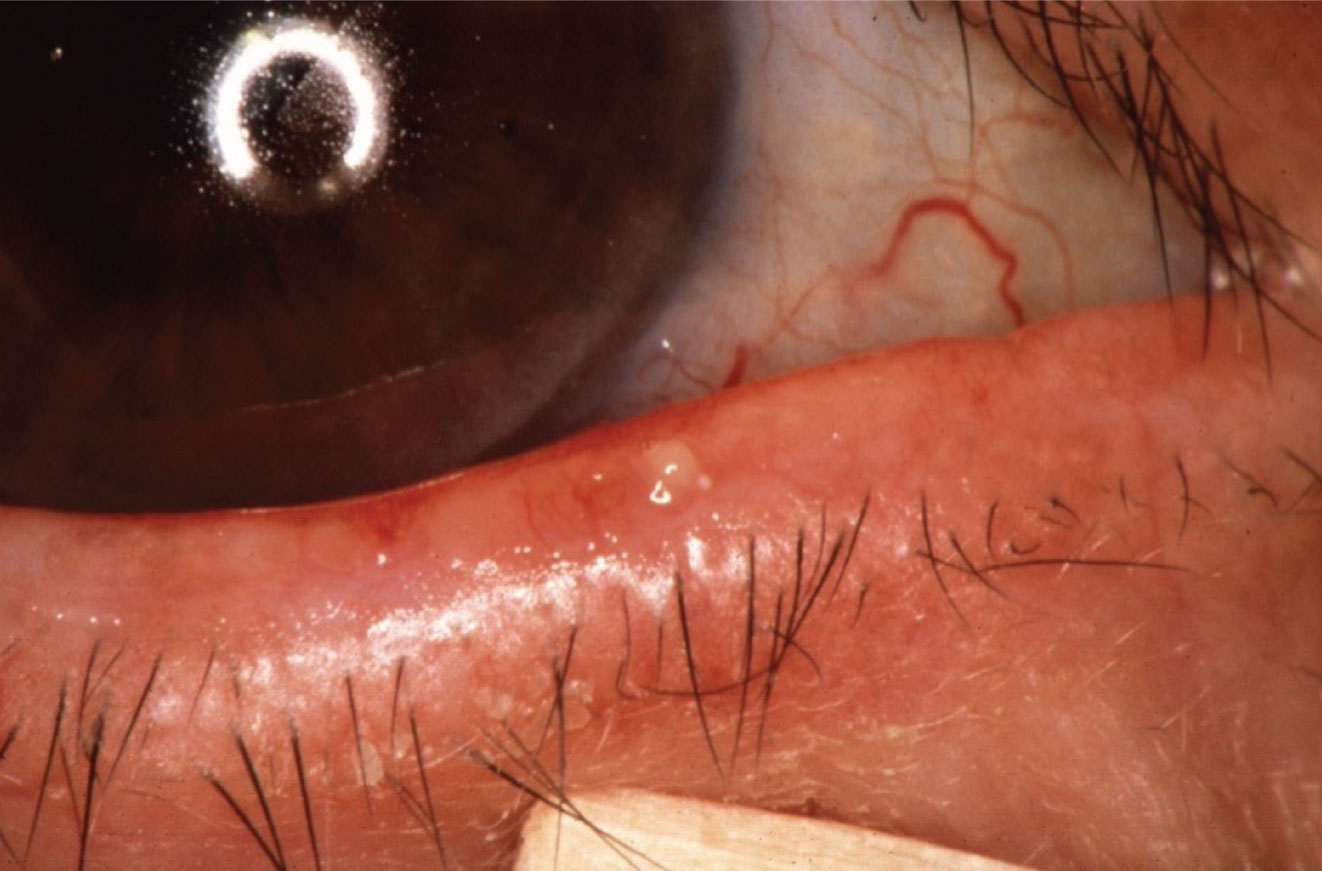 |
|
In a PRK candidate with meibomian gland dysfunction gentle expression of a blocked meibomian gland can help both diagnose the extent of the MGD as well as treat it. |
In addition, variations in anatomy may render the patient to be at higher risk for LASIK flap-related complications.8 These include history of epithelial basement membrane dystrophy, history of recurrent erosions, very flat or very steep corneas, or anteriorly placed scleral buckles.3,8 PRK would be preferable over LASIK in these situations.
For patients with occupations that place them at higher risk for flap dislocation, such as athletes or military personnel, they may elect PRK over LASIK, as traumatic LASIK flap dislocation is a known complication that can occur several years after the procedure.9 Finally, PRK is often used as a reliable means for refractive enhancement following prior cataract surgery or LASIK.10,11
Similar to other refractive surgeries, contraindications to PRK include uncontrolled or significant eye diseases, including severe ocular surface diseases and atopy.3 Systemic connective tissue diseases and uncontrolled diabetes mellitus may be considered relative contraindications as these patients are at risk for delayed epithelial healing.3 Furthermore, PRK should be postponed in patients who are currently pregnant, breastfeeding or who are taking medications that can affect their ocular health.12 Patients with a history of herpes simplex keratitis should be treated with prophylactic antiviral medication for several months before the PRK procedure to reduce the risk of perioperative viral reactivation.3 Meibomian gland disease and blepharitis must be treated and controlled prior to the procedure; measures include lid hygiene, surface lubrications and oral tetracyclines.
Prior to the procedure, patients are instructed to discontinue soft contact lenses for three days and hard contact lenses for two weeks in order to avoid corneal warpage, which can impact preoperative corneal measurements.3
PRK Technique: A Review
The procedure begins with epithelial debridement, which removes the epithelium without disrupting Bowman’s layer. The debridement can be achieved by several methods, including mechanical removal via spatula, mechanical removal using a rotary brush, chemical removal using an alcohol solution, and removal using a femtosecond laser.13-15 Among these various methods, removal of the epithelium using a diluted alcohol solution of 20% ethanol within a 6- or 7-mm corneal marker has been associated with the best long-term visual outcomes and a faster mean epithelial healing time.13-18 Once the epithelium is debrided, a 193-nm argon fluoride excimer laser is used for the surface ablation of the stroma itself.3 Additional pulses to the central 2.5-mm area may help to prevent central corneal islands. Patient fixation and cooperation throughout the procedure are important, in order to avoid decentered ablations, which can lead to poor visual outcomes.
Postoperative Pain and Considerations
Acute postoperative pain typically begins soon after surgery, peaking at about 24 hours, and continues over the first three to five postoperative days until re-epithelialization is complete.19-21 Most patients do report some level of acute pain after PRK, and self-reported pain severity can vary widely.19 Several pain management strategies are available. Topical non-steroidal anti-inflammatory drugs such as ketorolac tromethamine 0.5% or diclofenac 0.1% may be used postoperatively, but these are associated with delayed epithelial regeneration; thus, patients are typically instructed to use these sparingly, i.e., for breakthrough pain.17 Oral codeine/acetaminophen 30/500 mg administered four times per day for four days after PRK has been shown to be a safe and effective way to control post-PRK pain.22
Other pain management modalities for post-PRK pain include short-term oral gabapentin, ketorolac-soaked bandage contact lenses and chilled bandage contact lenses.23-25 A bandage contact lens remains in place post-procedure, and is removed several days after the procedure. Topical fourth-generation fluoroquinolone drops such as moxifloxacin 0.5% and gatifloxacin 0.3% are prescribed to prevent infection during this period. While the epithelium is usually healed by day three, waiting to remove the bandage lens until day five may reduce the frequency of postoperative pain and discomfort, as well as epithelium-related complications (filamentary keratitis and recurrent corneal erosion).26
Postoperatively, patients may experience four to six weeks of halos or blurring while the epithelium regenerates and should be counseled on this to establish expectations.3
Corneal Haze
Corneal haze is more likely to occur in PRK than in LASIK and occurs more frequently in hyperopic and large myopic or astigmatic corrections.3,27,28 Mild early haze incidence peaks around two months, while severe late haze peaks at around four months.27
In regard to prevention of haze formation, the application of topical mitomycin-C has been shown to play an important role in preventing haze.29,30 In a meta-analysis, the usage of MMC during PRK reduced both early- and late-onset haze, and improved the predictability of refraction and subjective postoperative visual acuity.30
While corticosteroids are commonly administered routinely after PRK, studies have demonstrated conflicting and controversial results, especially when it comes to its role in haze prevention.31,32 A more recent systemic review and meta-analysis suggests that steroids can reduce postoperative corneal haze and myopic regression during the first six months after refractive surgery.33 In addition, long duration of steroid administration (more than three months) post PRK appeared to be unnecessary in low and moderate myopia compared with high myopia.33
Ultraviolet-B (UV-B) has been associated with corneal subepithelial haze and abnormal stromal repair following PRK.17,34 Patients should also be advised to wear UV-blocking sunglasses when appropriate for at least six months postoperatively.17 Oral ascorbate has been shown to have a protective effect against haze formation following PRK.35 A survey study showed that the most common regimen used postoperatively to prevent post-PRK haze were sunglasses, mitomycin-C, topical corticosteroids and oral ascorbate.36
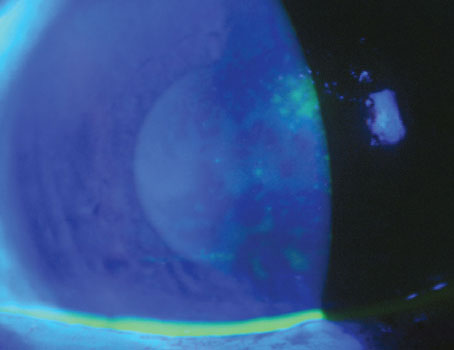
 |
|
More common with PRK than LASIK, corneal haze occurs more frequently in hyperopic and large myopic or astigmatic corrections. |
Management of Post-PRK Haze
Clinically significant corneal haze post-PRK can be separated into the categories of early-onset haze (less than three months following PRK), versus late-onset haze (greater than three months following PRK). Early-onset haze typically responds well to topical steroids, whereas late-onset haze tends to be more resistant to them.37-39
For early-onset haze, topical prednisolone acetate 1% may be used five to six times daily and tapered over the course of three months. Adjunct serial imaging (such as slit lamp photography, anterior segment OCTs, epithelial maps, and Scheimpflug densitometry) along with slit lamp examinations performed over the subsequent weeks may be helpful in monitoring the response.37 If haze persists beyond three months, it’s considered to have progressed to late-onset haze, and further intervention is warranted.37
For late-onset haze, topical prednisolone acetate 1% may be initiated, similar to early-onset haze. However, unlike early-onset haze, if improvements aren’t seen by four weeks, surgical intervention can be discussed with the patient.37
Surgical interventions for superficial corneal haze refractive to medical therapy comprise mechanical debridement or superficial PTK for less than 15 μm.38 If haze involvement is more than one-fifth of the corneal thickness or deeper than 15 μm, deep PTK or therapeutic myopic PRK ablation can be performed.38 The laser ablation depth is set to the haze depth, after accounting for the thickness of the epithelial hyperplasia.37
Alternatively, based on surgeon preference, instead of deep PTK or therapeutic PRK, a beaver or crescent blade or a diamond burr can be used to remove the underlying stromal haze after epithelial debridement.37 In either approach, 0.02% MMC (usually via a soaked sponge) is applied to the surface for two minutes,37,39 followed by copious irrigation of the cornea with balanced salt solution.
Regression
Regression is a risk of any refractive surgery. Refractive regression is defined as the gradual, partial or complete loss of the attempted correction, and affects the predictability of refractive surgery procedures; regression is deemed to be mainly due to epithelial hyperplasia and stromal remodeling.41,42 Most cases of myopic regression develop over the first three months after surgery, with only a slight change after the first three months and up to 10 years.41,42
Higher refractive correction (>-5 D), small optical zone (<6 mm) and unstable fixation during laser ablation of PRK for myopia and myopic astigmatism were found to be associated with higher risk for regression.43 Additionally, corneal haze post-PRK can also contribute to refractive regression.28
The main indication for retreatment is patient dissatisfaction with visual acuity due to the residual refractive error.28 Compared to older studies, one study by Utah’s Majid Moshirfar, MD, and his co-authors demonstrated that modern PRK enhancement after PRK has improved visual acuity and refractive outcomes.44 While PRK enhancement isn’t an FDA-approved procedure, the authors demonstrated that PRK enhancement meets or exceeds the FDA criteria for the correction of refractive error.44
When considering PRK enhancement, the surgeon should determine that there is stability of the refraction for at least six months.
Additional Complications
Mildly decentered ablation is quite common and is of little clinical significance. Decentration, however, becomes clinically significant when the decentration is greater than 0.5 mm from the visual axis.42 Decentered treatments may be associated with poor postoperative visual acuity and decreased quality of vision.45 Topography-guided customized ablation can be an effective option for patients who underwent prior eye surgery that resulted in decentered ablation.46,47
The incidence of central corneal islands is higher in PRK compared to LASIK. Following PRK, most cases of central islands resolve by one month, and nearly all resolve by one year.48,49
Therefore, conservative management is generally recommended, especially in the early postoperative period, with regular monitoring using topography. Asymptomatic central corneal islands don’t warrant treatment. Persistent, symptomatic central islands may need surgical intervention, but stability of the island (for at least six months) should be established prior to treatment. PTK is used to treat symptomatic and persistent central islands; at this time, there’s no consensus regarding the best ablation algorithm to treat central corneal islands.50,51
Corneal ectasia may occur after refractive surgery, although the incidence is lower in eyes undergoing PRK than LASIK.52
In conclusion, given PRK’s unique advantages, the procedure will continue to play an important role in refractive surgery, as it can serve as the preferred modality of vision correction in certain patients. By becoming familiar with the pearls and pitfalls surrounding the procedure, the surgeon can ensure that PRK is a safe and effective procedure that affords excellent visual outcomes and patient satisfaction.
Ms. Pajek is an MD & MPH Candidate and Cornea Research Fellow at the Bascom Palmer Eye Institute at the University of Miami.
Dr. Koo is an associate professor of clinical ophthalmology at the University of Miami Miller School of Medicine, and practices at the Bascom Palmer Eye Institute. Neither author has a financial interest in any product mentioned.
Corresponding Author:
Ellen Koo, MD
Bascom Palmer Eye Institute
900 NW 17th St
Miami, FL 33136
email: exk126@med.miami.edu
phone: 561-355-8974