Femtosecond Laser Cataract
The precision of femtosecond laser cataract surgery received support from the results of a combined group of surgeons from Bascom Palmer and the Dominican Republic. In a trial, 29 patients had one eye randomly assigned to receive capsulotomy and lens fragmentation with a femtosecond laser (OptiMedica) while the other acted as a control eye with standard manual anterior capsulotomy and lens fragmentation.
The excised capsulotomy disc was removed, followed by phacoemulsification and placement of an intraocular lens. Calibrated high-definition video microscopy was used to measure the excised capsulotomy disc. The shape and diameter of the anterior capsular disc as well as centration of the resulting opening were assessed.
The average deviation of the capsulotomy disk diameter from intended was 29 ±25 µm with laser and 329 ±250 µm with manual capsulorhexis. With 1.0 defining a perfect circle, the average circularity for laser capsulotomies was 0.94 ±0.04, while for manual CCC it was 0.77 ±0.15. Cataracts with LOCs grade 1 to 4 were treated in both groups with 50 percent of cataracts being grade 3. On average, the CDE was reduced by 40 percent from 18.9 (manual) to 11.6 (laser). All results were statistically significant (p<0.05).
Deviation of the diameter of the anterior capsulotomies produced by femtosecond laser from intended was 12 times smaller and deviation from round shape was four times lower than those with manual CCC. Pre-conditioning of the cataract with the femtosecond laser reduced the Cumulative Dispersed Energy by 40 percent, which might lead to reduction of surgical side effects like endothelial cell loss, the group says.5694
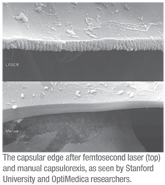 Researchers at OptiMedica and Stanford University evaluated the appearance of the capsular edge and its rupture strength in capsules cut by manual capsulorhexis and femtosecond laser. After the cornea and iris in porcine eyes were surgically removed (n=46, less than 24 hours post enucleation), 13 manual and 33 laser capsulotomies 4.6 mm in diameter were created. Laser pulse energies ranged from 3 to 10 µJ. The lens cortex and the nucleus were then completely removed by standard ultrasonic phacoemulsification. For the capsular stretching experiments the empty capsular bags were refilled using a low-viscosity liquid containing 0.05% gelatin. The eye was mounted on an X/Y/Z translation stage such that two symmetrical half-cylinder stretching pins with 2 mm radius of curvature fit into the capsular opening. The pins were then symmetrically pulled apart and the force on both pins was recorded.
Researchers at OptiMedica and Stanford University evaluated the appearance of the capsular edge and its rupture strength in capsules cut by manual capsulorhexis and femtosecond laser. After the cornea and iris in porcine eyes were surgically removed (n=46, less than 24 hours post enucleation), 13 manual and 33 laser capsulotomies 4.6 mm in diameter were created. Laser pulse energies ranged from 3 to 10 µJ. The lens cortex and the nucleus were then completely removed by standard ultrasonic phacoemulsification. For the capsular stretching experiments the empty capsular bags were refilled using a low-viscosity liquid containing 0.05% gelatin. The eye was mounted on an X/Y/Z translation stage such that two symmetrical half-cylinder stretching pins with 2 mm radius of curvature fit into the capsular opening. The pins were then symmetrically pulled apart and the force on both pins was recorded.
Strength was measured as the maximum force exerted on the capsule until it tore. The rupture strength was determined in each of the manual and lasered eyes. Depending on pulse energy, the laser-created capsulotomies had about two- to threefold higher break force (152 ±21 mN for 3 µJ, 121 ±16 mN for 6 µJ, 113 ±23 mN for 10 µJ) compared to those created by the manual technique (65 ±21 mN). All results were statistically significant (p<0.05). Scanning electron microscopy analysis of the laser capsulotomy edges (See image, right) revealed microgrooves spaced by 5 µm, which corresponds to the laser spot spacing. The group calls the stronger edge provided by the laser capsulotomy an important safety aspect that may reduce the risk of capsular ruptures during cataract surgery.5704
Cataract Surgery Issues
In patients undergoing bilateral sequential cataract surgery, and where the first eye refractive error exceeded 0.5 D, the refractive error of the second eye can be improved by modifying the IOL power to correct 50 percent of the error from the first eye, according to a group at the University of Illinois, Chicago.
The researchers measured both eyes of 250 consecutive patients with the IOLMaster prior to the first eye’s surgery. Second eye surgery was done in one to three months. The first eye refractive error (FERE) was evaluated before the second eye’s surgery. FERE exceeded 0.50 D in 97 patients (38.8 percent). When choosing the IOL power for the second eye in these patients, the calculations were adjusted to correct 50 percent of the error from the first eye. The adjusted second eye refractive error (SERE) was evaluated six to eight weeks after surgery, and compared to the first eye refractive error.
 The median absolute adjusted SERE was significantly lower in the second eye compared to the median absolute FERE in these 97 eyes (0.39 vs. 0.77 D, p=1.85). The statistically significant differences and ranges in these 97 were:
The median absolute adjusted SERE was significantly lower in the second eye compared to the median absolute FERE in these 97 eyes (0.39 vs. 0.77 D, p=1.85). The statistically significant differences and ranges in these 97 were:
- in the 47 patients where FERE was between -0.5 and -1 D: 0.39 vs. 0.66 D, p=0.0004;
- in 15 patients where FERE exceeded -1 D: 0.65 vs. 1.25 D, p=0.0008;
- in the 24 patients where FERE was between +0.5 and +1 D: 0.32 vs. 0.65 D, p=8.0E-06; and
- in the 11 patients where FERE exceeded +1 D: 0.57 vs. 1.19 D, p=0.005.
The median aSERE was also compared to a potential non-adjusted SERE (nSERE) and a potential fully adjusted SERE (fSERE). aSERE were lower than nSERE (0.39 vs. 0.50, p=0.0001) and than fSERE (0.39 vs. 0.44, p=0.06).2790
Since the advent of sutureless, clear corneal incisions in cataract surgery, the risk of surgical wound gaping has become especially relevant. A combined study by surgeons at the University of Toronto and the Wilmer Eye Institute evaluated the early postoperative integrity of the port incisions, the incidence of gaping and the factors that may relate to wound instability.
The study included 40 eyes from 40 patients after uncomplicated cataract surgery. All patients underwent a standard exam on postop day one, including slit-lamp exam, intraocular pressure measurement, and optical coherence tomography to detect and measure the degree of gaping.
Although incision gaping was not visible by slit-lamp, OCT revealed side-port incision gaping in 10 out of 40 (25 percent) patients. The average proportion of gaping, relative to the length of the incision was 21.8 percent (r: 9.1 to 40.1 percent). Neither age nor postop IOP showed any significant effect on gaping. There was a statistically significant relationship between the axial length and side-port incision gaping (p<0.05).
 Linear regression indicated a mild but significant correlation between AL and the degree of port incision gaping (p=0.0153), with longer eyes having higher risk for postoperative gaping. Side-port incisions are susceptible to varying degrees of early postop gaping and may represent an overlooked portal for intraocular contamination. The presence of gaping in the port incision is significantly correlated with AL.6236
Linear regression indicated a mild but significant correlation between AL and the degree of port incision gaping (p=0.0153), with longer eyes having higher risk for postoperative gaping. Side-port incisions are susceptible to varying degrees of early postop gaping and may represent an overlooked portal for intraocular contamination. The presence of gaping in the port incision is significantly correlated with AL.6236
IOL Issues
A small study in Florida evaluated patient outcome following Tecnis multifocal (ZMA00 and ZMB00) and ReSTOR+3 Add lenses (SN60D1) in patients with previous laser vision correction. Eleven eyes of eight patients were evaluated. Mean patient age was 65.5 years, three male, five female. Four eyes of three patients had a Tecnis MF implanted, while seven eyes of five patients received a Restor +3 Add.
No patients had intraoperative limbal relaxing incisions. Postoperatively, three eyes underwent YAG capsulotomy; four eyes had a laser vision correction procedure; and one eye underwent a piggyback IOL to optimize the refractive results. Overall, 75 percent of eyes achieved 20/25 or better UCVA at distance and 60 percent achieved 20/25 or better UCVA at near. Overall, patients with previous laser vision correction were satisfied with their postoperative visual results following multifocal IOL implantation, although 45 percent of eyes required postoperative vision enhancements with either laser vision correction or a piggyback IOL. (Some of the researchers report commercial relationships with Abbott Medical Optics.)5690
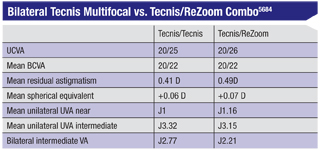
A surgeon in Wilkes-Barre, Pa., retrospectively compared patient satisfaction and spectacle independence in patients (n=60) who had bilateral Tecnis multifocals to those (n=72) who had a combination of the Tecnis multifocal and a ReZoom. (A commercial relationship to AMO was reported.)
Near vision was favored in the Tecnis cohort and intermediate vision was favored in the Tecnis/ReZoom cohort, but the differences were not significant. Clinically, the Tecnis/ReZoom group reported more halos and glare but statistically the differences were not significant. No explantations were performed in either group.5684
Researchers at Abbott Medical Optics in Europe used computer models to simulate how corneal aberrations influence the subjective appearance of halos obtained with multifocal IOLs. Retinal images of extended light sources were simulated in the computer-based eye models. The corneas of the eye models were based on measured data from cataract patients. They included higher-order aberrations, as well as residual lower-order aberrations. These models were then implanted with a bifocal intraocular lens. The point spread function of the eye was convolved with an extended light source, resulting in a retinal light intensity profile. Features of the retinal light intensity profile were correlated with the corneal aberrations.
The retinal light intensity profiles represented a wide variety of halo appearances. The size of the halo (area) varied by a factor of three due to differing cornea aberration profiles. The area of the halo tended to be correlated with the RMS of the higher-order corneal Zernike aberration, although this was not statistically significant (p=0.1). The images revealed very specific features, such as elliptical shapes, and eccentric areas of increased light intensity. Eye length and total optical power of the eye did not correlate with the appearance of these features. The group concludes that the size, shape and intensity of the multifocal halo vary with each eye. Their images suggest that corneal aberrations have a significant effect on the appearance of halos on the retina.6186
Surgeons in Rome, Italy, report that the AcrySof phakic angle-supported Cachet IOL (Alcon) yielded excellent refractive correction and predictability for the correction of moderate and high myopia, with no change in endothelial cell density count during a six-month follow-up. They implanted 19 eyes of 10 patients (mean age 38.26 ±8.98 years) with moderate to high myopia with an AcrySof Cachet.
Manifest refraction SE, UCVA, best spectacle-corrected visual acuity and endothelial cell density were evaluated both preoperatively and six months postop.
The mean preoperative MRSE was -9.49 ±3.08 D (r: -6.00 to -16.75 D). The six-month postoperative mean MRSE was -0.29 D (±0.41; p<0.001). The mean preop endothelial cell density was 2,829 ±301 cell/mm2; the six months postop ECD was 2,902 ±334 cell/mm2 (p=0.67). No iridotomy was performed preoperatively. No pupil ovalization or pupillary block were observed postoperatively.6188
A retrospective chart review at the Rocky Mountain Lions Eye Institute looked at IOL exchanges over a five-year period. Records were reviewed to include three years of follow-up after exchange. The review showed that 35 eyes of 31 patients underwent IOL exchange. The average age was 66.7 years; 54.8 percent were female; and four patients had undergone previous LASIK or RK. At least 45.7 percent of the explanted IOLs were multifocal.
The most common reasons for exchange were IOL dislocation 34.3 percent, dysphotopsia 31.4 percent, and anisometropia 22.9 percent. All cases of exchange for dysphotopsia were for multifocal IOLs. The remaining 11.4 percent of patients underwent exchange for pseudophakic bullous keratopathy, cystoid macular edema, chronic iritis, or lens-induced pigment dispersion with secondary glaucoma. Vitrectomy was performed concurrently in 31.4 percent of exchanges. The most common complications were secondary glaucoma 14.3 percent, residual astigmatism 11.4 percent, and iritis 5.7 percent. Mean BCVA was 20/53 preoperatively and 20/44 three months postop.
Multifocal IOLs cause more dysphotopsia than standard IOLs, the group concludes, and it calls for larger studies to explore the growing subset of multifocal IOL exchanges.6220
Misplacement of IOL haptics and haptic-induced ocular irritation after cataract surgery may remain undiagnosed for several months, mimicking other conditions, according to surgeons at the Cleveland Clinic/Cole Eye Institute. The group performed ultrasound biomicroscopy using a 50-MHz probe in 14 pseudophakic eyes, clinically suspected to have misplaced intraocular lens haptics. Patients were referred due to chronic postoperative inflammation, recurrent hyphema, increased intraocular pressure or recurrent vitreous hemorrhage or a combination of those.
Time from cataract surgery to referral/diagnosis of misplaced haptics by UBM ranged from two to 144 months (mean 57 ±48 months). Seven patients (50 percent) had sulcus-implanted IOL, and seven had an in-the-bag intraocular lens. Six patients (42.8 percent) had a history of chronic postoperative inflammation. Five patients (35.7 percent) had recurrent episodes of hyphema. Elevated IOP was found in nine eyes (64.8 percent). A history of recurrent vitreous hemorrhages was elicited in eight patients (57.1 percent). Intraocular lens haptics misplacement was confirmed by UBM in all suspected cases. In 12 eyes, at least one haptic was embedded in or touching the iris. Haptic extension into the ciliary body process was observed in two patients, and into the pars plana in another. Focal iris thinning/atrophy was detected by UBM in three cases. Focal angle closure associated with haptic misplacement was found in four eyes. IOL exchange was performed in four cases. Out of the nine patients who presented with elevated IOP, seven had it controlled with topical IOP-lowering medications. Two patients were maintained on cycloplegics and topical steroids.
The group calls UBM a valuable tool in confirming the clinical suspicion of misplacement of the lens haptics. Imaging findings, along with the presenting features, are essential in assisting the physician in the decision-making process of management of these patients.6227
Pharmaceuticals
A group in São Paulo, Brazil, cau-tions against sole reliance on the minimum inhibitory concentration as a guide to antibacterial efficacy, saying this may be misleading. Even newer-generation fluoroquinolones failed to demonstrate a significant aqueous bioavailability using a dosing regimen that simulated prophylactic use after cataract surgery in their study.
In the study, 96 rabbit eyes were topically treated with a commercially available formulation of ciprofloxacin 0.3%, levofloxacin 1.5%, gatifloxacin 0.3% and moxifloxacin 0.5% eye drops and intracamerally injected into the anterior chamber with moxifloxacin 0.5% and cefuroxine 1%. Following an initial loading dose of a single antibiotic drop, the aqueous humor was sampled at 30 minutes, one, two and four hours. Biological activity was indirectly determined from the size of the zone of inhibition of filter paper disc soaked in 25 µl of aqueous humor withdrawn from treated eyes and placed on an agar plate surface cultured with Staphylococcus epidermidis.
Although it was not significant, moxifloxacin eye drops showed an initial (30 minutes and one hour post-treatment) trend towards superior aqueous bioactivity compared to all other tested formulations. At and following the second hour, the aqueous humor withdrawn from all treated eyes failed to demonstrate any bacteria inhibitory potential for the four tested formulations, since no zone of inhibition could be observed. For the intracameral groups both moxifloxacin and cefuroxime showed a significant short-term inhibition on the culture plates at 30 minutes, one and two hours. After the second hour no inhibition could be observed.5693
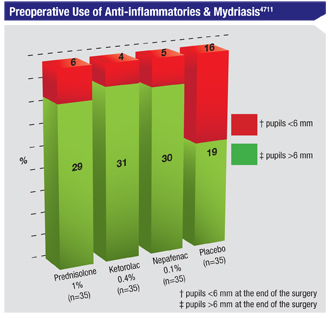
Prophylactic use of ketorolac, prednisolone and nepafenac was effective in maintaining intraoperative mydriasis in a Brazilian study and can be used in surgical practice with similar effectiveness, say the authors.
The masked, single-center, ran-domized clinical study comprised 140 patients undergoing phaco- emulsification cataract surgery. Patients were randomized to receive either placebo carboxymethylcellulose sodium 0.5%, prednisolone acetate 1%, ketorolac thrometamine 0.4% or nepafenac 0.1%. These drops were administered 48 hours before surgery. Digital photos of the pupil were taken preoperatively, at the beginning of the surgery, and postoperatively, immediately at the end of the surgery. The primary endpoint was to measure the efficacy of each medication to inhibit miosis (to achieve pupils >6 mm at the end of the surgery). The secondary outcome was to achieve pupils >6 mm at the beginning of the surgery.
The comparison of the prednisolone, nepafenac and thrometamine groups with the placebo group was statistically significant (p<0.005) in the maintenance of intraoperative mydriasis. All patients achieved preoperative mydriasis >6 mm at the beginning of the surgery.4711
Soaking intraocular lenses in antibiotic solution in their native packaging allows the lenses to act as drug depots with antimicrobial properties in vitro, according to surgeons in New York.
The researchers injected 30 mL of moxifloxacin 0.5% (Vigamox) directly into the plastic case containing one of two types of acrylic IOLs (AcrySof SA60AT and SN60WF) via preexisting ports in the lens packaging. The IOL was allowed to soak in the antibiotic for one minute. The IOL delivery was performed with a cartridge filled with sodium hyaluronate as is done in routine cataract procedures.
Nine IOLs were injected onto an agar plate seeded with Staphylococcus epidermidis without rinsing the sodium hyaluronate and eight lenses were injected onto plates after rinsing with BSS for one minute. This process was then repeated using agar plates seeded with Staphylococcus aureus. A control group consisted of IOLs not soaked in antibiotic which were plated using the above methods.
In the S. epidermidis group, the average inhibitory zone was 22.44 mm with a standard deviation of 8.19 in the BSS rinse group, and 27.75 mm with an SD of 8.71 in the non-rinsed group. In the S. aureus group, the average inhibitory zone was 24.44 mm with a 6.02 SD in the rinsed group, and 22.78 mm with a 1.99 SD in the non-rinsed group.4726
Miscellaneous
A group of researchers at Vanderbilt Eye Institute studied chronic uveitis developing after cataract extraction, and suggests that aggressive measures to prevent inflammation and limit its severity and duration in eyes with intraoperative complications may impact the risk of developing chronic uveitis.
In the eight-year, retrospective chart review, chronic uveitis was defined as persistent intraocular inflammation or continued need for immunosuppressive therapy for a minimum of six months after cataract surgery. Patients were excluded if they had a history of uveitis prior to cataract surgery due to any cause.
In 13,165 cataract surgeries, 26 eyes of 22 patients developed chronic uveitis (0.2 percent). Seven of these eyes (27 percent) experienced intraoperative complications that included any or all of the following: posterior capsular rupture; unplanned vitreous loss with anterior vitrectomy; and unplanned placement of an IOL in the sulcus or anterior chamber. Eight patients underwent consecutive cataract surgery in both eyes (<four weeks apart) and developed unilateral chronic uveitis. Four of these eight eyes with chronic inflammation experienced intraoperative complications compared to none of the eight fellow eyes that did not develop chronic inflammation (p<0.05).4713
Dr. Blecher is in private practice in Philadelphia. He is the co-director of the Cataract Service at Wills Eye Institute and the founding chief med-ical editor of the Review.



