This year’s cornea section shows a robust level of activity by scientists and clinicians, with more than 1,600 abstracts being presented at ARVO. Collagen crosslinking and improved techniques in keratoplasty continue to produce the lion’s share of work that will interest the practicing ophthalmologist, though there is much of note in other areas. Here is but a sampling of the work. (Disclosed commercial relationships and support are indicated where applicable.)
Crosslinking
Epithelium-on corneal collagen crosslinking appears to be a safe and effective treatment for patients with corneal ectatic disease, say researchers at various U.S. sites, some of whom are members of the CXL USA Study Group. There were 181 (127 male, 49 female) eyes enrolled in the study that underwent epithelium-on crosslinking, with preservative-free 0.1% isotonic riboflavin for 30 to 90 minutes. Riboflavin loading was stopped once the cornea was determined by slit-lamp examination to be saturated. UV light was initiated for 30 minutes after ensuring that the minimum corneal thickness was at least 400 µm. Follow-up ranged from three months minimum to 18.7 months maximum with a mean of 10.85 months; 81 percent had keratoconus, 15 percent had post-LASIK ectasia, and 2 percent had pellucid marginal degeneration.
Postop, average corneal hysteresis values increased from 7.3 to 7.8, and average corneal resistance factor values increased from 5.9 to 7.8. Average refractive cylinder decreased from 4.52 D to 3.96 D. Average 2-mm K astigmatism (Pentacam) decreased from 5.47 to 4.66, and average Holladay astigmatism decreased from 3.18 to 2.19. In 35.8 percent of eyes there was no change in the number BSCVA lines, and 46.4 percent of eyes gained one or more lines; 30.2 percent of eyes experienced a loss in one or more lines of BSCVA. Average BSCVA preop was 20/145 and postop was 20/114.6786
Researchers in Milan, Italy and Dresden, Germany, compared changes in biomechanical properties of human cadaver corneas after standard transepithelial crosslinking (CXL-TE), CXL-TE using iontophoresis, different solutions and irradiance power. The four treatment groups are shown in Table 1.
|
Brazilian researchers found a significant increase in intraocular pressure after crosslinking treatment in keratoconic patients, though the mechanism remains uncertain. In a prospective interventional study, they measured IOP (Goldmann and Pascal tonometers) and central corneal pachymetry before and one month after the corneal crosslinking with riboflavin 0.1% and ultraviolet A for 30 minutes in 12 patients (17 eyes, mean age, 24.4 ±9.1 year, eight females).
Both tonometers revealed a statistically significant increase in the mean IOP one month after crosslinking. The increase in the means were 2.4 ±0.4 mmHg for Goldmann (p=0.0053) and 2.9 ±0.7 mmHg for Pascal (p=0.0001). Pachymetry showed no statistically significant difference, with means of 481.1 ±42.8 µm preop, and 481.6 ±37.4 µm one month postop (p=0.8852). The authors speculate that the increased IOP could be caused by an increase in corneal rigidity but caution that the possibility of a “true” IOP increase cannot be excluded, possibly due to an effect from the crosslinking on the trabecular meshwork.1520
Researchers at the University of California, San Francisco, have developed an approach to crosslinking that may offer a means of achieving clinically useful concentrations of riboflavin in the cornea without removing the corneal epithelium, thereby improving the risk profile of corneal crosslinking procedures. The key: ultrasound.
They placed fresh cadaveric rabbit eyes with intact corneal epithelium in a solution of 0.1% riboflavin at 37C. Continuous wave ultrasound at 1 W/cm2 was applied to the central cornea for five minutes, and the eyes were then left in riboflavin solution for an additional 40 minutes. Control eyes received the same exposure to riboflavin solution without ultrasound treatment.
They found that at a depth of 200 µm, average fluorescence intensity of riboflavin was 162 in the 12 treated eyes and 69 in five control eyes. The confocal images suggested the existence of some areas of epithelial cell damage on the anterior surface of ultrasound-treated eyes. Ultrasound treatment facilitated the entry of topical riboflavin into the corneal stroma despite the presence of a previously intact epithelial barrier.6806
Photo-crosslinking stromal collagen to stiffen the cornea may be an alternative to the more common riboflavin/UVA treatment, say researchers in Boston. Their work suggests that it’s faster and non-toxic to stromal keratocytes. (Some of the researchers report a commercial relationship to the technology’s developer.)
After applying Rose Bengal dye for two minutes, de-epithelialized rabbit corneas were exposed to green (532 nm) light from a KTP laser for one to five minutes. For comparison, additional corneas were treated with 0.1% riboflavin for 30 minutes, then exposed to UVA while applying drops of riboflavin, similar to the clinical treatment. Mechanical testing was used to calculate Young’s modulus, a measure of stromal stiffness. The depth of stromal penetration of the solutions was determined by the dye fluorescence intensity on confocal microscopy, every 10 µm from the anterior surface. Cell viability was determined by H&E staining at 24 hours.
The same increase in stromal stiffness was produced by both methods, when dye-treated corneas were treated with only five minutes of green light. Values of Young’s modulus for dye-treated (34.0 ±7.4 MPa) and riboflavin-treated (31.8 ± 11.2 MPa) corneas were greater than that for untreated corneas (15.4 ±5.1 MPa, p<0.05). Rose Bengal penetrated less deeply than riboflavin into the stroma, as indicated by the decrease in dye fluorescence with distance from the anterior surface, which reached 10 percent of the initial intensity by 93 ±6 µm. Thus the dye/green light-initiated crosslinks are produced closer to the anterior surface than with riboflavin/UVA, since riboflavin penetrated throughout the cornea. RB/green light did not affect keratocyte viability, whereas riboflavin/UVA decreased cell viability to less than 5 percent.
The group reports that the new method effectively crosslinked stromal collagen in less than seven minutes total treatment time and was not toxic to keratocytes, suggesting that this procedure has potential as a second generation photo-crosslinking treatment for keratoconus.6813
Long-term follow-up confirms that crosslinking is effective in arresting progressive keratoconus, say surgeons in Switzerland and Milan. They report three-year results on 97 eyes of adults with progressive keratoconus that underwent standard crosslinking treatment. BSCVA, refraction, topography, tomography and aberrations were documented at regular intervals, and BSCVA results for different age groups were compared with a cohort of crosslinking-treated pediatric eyes.
At 36 months, mean BSCVA had significantly (p<0.05) improved from 0.47 ±0.29 to 0.73 ±0.24 (decimal scale). Sixty-one percent of the eyes had gained two or more lines of BSCVA by the three-year follow-up. Mean spherical equivalent refraction had improved from -3.74 D to -2.76 D. Mean cylinder was lowered from -2.69 D to -2.13 D. Topography maps exhibited a statistically significant improvement from 0.57 to 0.73. The authors suggest that improved BSCVA is likely due to the significant reduction of corneal asymmetry and wavefront aberrations. BSCVA improved in all age groups studied.6820
Keratoplasty
An experienced corneal surgeon’s learning curve when transitioning from penetrating keratoplasty to deep anterior lamellar keratoplasty will average about eight cases, say researchers at the New York Eye and Ear Infirmary. Their retrospective chart review of 18 eyes undergoing DALK by one surgeon documented clinical and anatomic success compared to the literature with more experienced surgeons in the DALK technique. The indication for surgery in 16/18 eyes was keratoconus (12 men, six women, average age: 35). One patient had lattice dystrophy and one patient had an HSV scar.
The overall conversion rate to PK at the time of surgery was 50 percent (9/18), in comparison to a conversion rate of approximately 15 percent in the literature. After the first six cases were completed, the conversion rate decreased to 25 percent, and after eight cases, the rate dropped to 20 percent. Average best-corrected visual acuity at the end of follow up was about 20/45 as compared to about 20/40 or better reported in the literature.16
A group at the Devers Eye Institute, Portland, Ore., also assessed an economic issue: the possibility that pre-cut tissue is unnecessarily deemed unsuitable for transplant by slit lamp and specular microscopy, traditional eye-bank exam techniques. Over a one-year period, two corneas were deemed not suitable for transplantation due to difficulty visualizing cells and atypical appearance of cell morphology upon specular and slit-lamp exam. The two and a sampling of six suitable corneas were trephinated, stained and imaged with fluorescent microscope; endothelial cell loss was calculated using Adobe Photoshop. Cell viability staining demonstrated a 10 percent cell loss at an average of five days post-processing for tissues deemed unsuitable, compared to 13 percent cell loss in the control group sample, a difference deemed not statistically significant (p=0.505). The group concludes that viability staining of the entire graft after processing could be helpful in determining suitability for transplantation and avoiding unnecessary tissue wastage.26
Two researchers at the University of California, San Francisco developed a cost analysis model comparing surgeon-cut and eye bank-cut donor corneal tissue for endothelial keratoplasty. Their findings suggest that at a volume of about 15 cases per year, surgeons may start to reduce costs by cutting their own tissue.
The model considered costs of equipment, consumable supplies, labor, building space and risk of unsuccessful attempts resulting in damaged tissue. Assuming a five-year lifespan of a microkeratome; a team consisting of a surgeon, a registered nurse, a certified scrub technician and a sterilization technician; a time of 30 minutes to cut the cornea before the patient is brought into the operating room; a 1 percent rate of returned corneal tissue secondary to surgeon-induced damage; and a 500 square-foot operating room, the cost per surgeon-cut donor cornea is: $301.90 based on 104 cases performed per year; $376.90 based on 52 cases; $526.90 based on 26 cases; and $826.90 based on 13 cases. The processing fee of a local eye bank to cut the donor corneal tissue is approximately $750. The investigators hope that the data may influence the practice patterns of providers and have implications for determining how third-party payer reimbursements are made.25
Direct needle insertion of the donor lenticule in Descemet’s stripping automated endothelial keratoplasty was found to be comparable to the Busin glide insertion technique with regard to the one-year endothelial cell loss, according to investigators in Irvine, Calif., and Denver, Colo. The retrospective study compared 15 cases of the direct needle insertion technique vs. 40 cases of the Busin glide insertion technique in DSAEK surgery over 18 months based on pre/postop VA, endothelial cell density, refractive error and complications.
Preliminary mean ECD loss was 18 percent at one year following the needle insertion technique and 22 percent for the Busin glide. Mean preop BCVA in both groups improved from 2.0 ±1.0 logMAR to postop mean BCVA 0.30 ±0.10 logMAR. The results are similar to previously reported studies of insertion techniques, and the group concludes that direct needle insertion is simple, cost-effective and fast.38
Surgeons at the University of Pittsburgh Eye and Ear Institute compared three lenticule insertion techniques: forceps, Busin and the Neusidl corneal inserter. The study included 40 eyes of 38 patients (average age: 73.45 years; average preop BCVA: 20/100) undergoing DSAEK surgery for Fuchs endothelial dystrophy, pseudophakic bullous keratopathy (PBK), and previous graft failure. They measured BCVA, and intra- and postop complications at 12 months, following 11 cases in which donor discs were inserted with forceps using the “taco” fold method, 18 with discs inserted with the Busin glide, and 10 with discs inserted using the NCI device.
At 12 months, no statistically significant differences were found among the three techniques in BCVA (p=0.152) or in postop complications (p=0.508) using ANOVA. Postop complications included graft dislocation; pupillary block glaucoma; high postop astigmatism; inflammation; and steroid-response glaucoma. All three groups had a Snellen equivalent close to 20/63, with a range of 20/20 to 20/80 at 12 months.39
Long-term graft survival rates after DSAEK was the focus of a 2.5-year retrospective chart review at New York Eye and Ear Infirmary. Only patients with a minimum of 36 months of follow-up were included, and those who developed primary graft failure (failure of the graft to clear at any point postop) were excluded. Included were 67 eyes of 65 patients; 56.9 percent were female and mean age at time of procedure was 69.4 years (range 33 to 89). Indications, by percentage, included: Fuchs dystrophy (40.3 percent); PBK (26.9); previously failed DSAEK (14.9); corneal endothelial failure from other causes (11.9); previous failed PK (3.0); aphakic bullous keratopathy (1.5); and trauma (1.5).
The overall three-year graft survival rate was 80.6 percent (n=54). The survival rate was highest in Fuchs dystrophy (96.3), decreasing to 77.8 in PBK, and lowest (37.5) in those with endothelial failure from anterior chamber hardware (e.g., glaucoma drainage devices) or disorganized anterior segments. Eyes with pre-existing glaucoma had a significantly higher risk of failure with a survival rate of 61.9 percent compared to 91.1 percent in eyes without glaucoma (p< 0.05).48
|
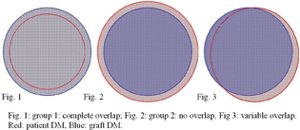
Based on the size of descemetorhexis three groups were found: 15 patients in which the graft and the patients’ DM overlapped completely (group 1); 21 patients in which no overlap was seen and in which the graft was separated from DM by a small gap (group 2); and 69 patients with variable overlap (group 3). Significant graft detachment appeared in 10 eyes of group 1 and three eyes of group 2. The area of peripheral detachment was significantly greater in group 1 than in group 2 (group 1, 3.5 ±1.0 hours, group 2, 0.9 ±0.3 clock hours, p=.002). Re-bubbling was performed in three eyes of group 1 due to persistent major detachment (9.2 ±1.3 clock hours), but was not necessary in group 2. They conclude that complete removal of DM in the area of the graft allows better adhesion of the graft. As greater overlap is a risk factor leading to graft detachment, patients with greater overlap must be followed more carefully.61
Researchers from Devers Eye Institute and the University of Michigan took on the graft thickness issue in a retrospective analysis of eyes that underwent DSAEK and had anterior segment OCT. They compared postop logMAR BCVA and manifest refraction to AS-OCT graft thickness at one, three, six, 12 and 24 months. Included were 43 eyes (average patient age: 66 ±12 years; r: 40 to 86). Mean logMAR BCVAs were: at 0.58 at one month; 0.39 at three months; 0.24 at six months; 0.22 at 12 months; and 0.33 at 24 months.
Further analysis was performed in patients who had both VA and AS-OCT measured at the same visit. There were no significant correlations of logMAR BCVA, spherical equivalent or amount of cylinder with graft thickness by AS-OCT at any time point. There was a trend of patient age correlating with logMAR BCVA at one month (r=0.78, p=0.07), three months (r=0.78, p=0.07) and one year (0.40, p=0.01). There was no correlation of eye bank post-cut graft thickness or transplant size to logMAR BCVA at any postop time points. The group concludes that while there was a trend of younger patient age correlating with better logMAR BCVA, preop (post-cut) and postop graft thickness were not correlated to logMAR BCVA or refractive outcomes at any time point.50
Surgeons at Doheny Eye Institute, Los Angeles, report a small case series of combined Descemet’s membrane endothelial keratoplasty and cataract surgery. They compared preop target refraction to postop refraction at least six weeks after the procedure in three patients who underwent combined surgery by the same surgeon using a temporal scleral tunnel approach. All three patients had Fuchs endothelial dystrophy.
Preop BCVA ranged from 20/30 to 20/150; postop was 20/25 to 20/30. All patients received a one-piece IOL targeting a spherical equivalent of -1 D. The average postop refraction was +0.125 D (SD=0.98), which demonstrated a hyperopic shift of 1.125 D. They conclude that refractive change may vary based on the individual patient but a -1 D target for implanted IOLs may be most appropriate, and they call for additional studies to develop accurate IOL power nomograms for patients undergoing this combined DMEK/cataract procedure.59
Other surgeons at multiple sites in Germany compared DMEK results with PKP. They reviewed the charts of all patients undergoing DMEK surgery in 2011 for VA and complications and compared these to a historical control group of PKP. Their findings:
|
Research in Indianapolis compared the rate of immunologic graft rejection in four types of corneal transplants: PK, Descemet stripping endothelial keratoplasty (DSEK), DMEK and Descemet’s membrane automated endothelial keratoplasty (DMAEK). (All four methods include corneal endothelium; PK has full-thickness donor stroma; whereas DSEK only has posterior stroma; DMAEK only has a 1-mm rim of posterior stroma; and DMEK has no donor stroma at all.) Data was collected prospectively on 200 consecutive DMEK and 100 consecutive DMAEK cases; rate and timing of rejection episodes was compared retrospectively with previously reported results in series of 598 DSEK cases and 30 PK cases performed at the same center, using the same postop corticosteroid regimen and the same evaluation criteria for rejection episodes. Overall, 89 percent of the grafts were done to treat Fuchs endothelial dystrophy; 62 percent of the recipients were female; 96 percent were Caucasian; and the relative proportions were comparable in all four transplant groups.
At two years, the Kaplan-Meier cumulative rejection-free survival rate was 99.4 percent for DMEK, 95 percent for DMAEK, 88 percent for DSEK and 82 percent for PK (p=0.0007). The relative risk of a rejection episode was substantially higher with PK than with any of the endothelial keratoplasty techniques. The relative risk of experiencing a rejection episode was six times lower with DMEK than DMAEK and 2.8 times lower with DMAEK than with DSEK. The relative risk of immunologic rejection decreased as the amount of donor stromal tissue in the graft decreased, and the risk of rejection was lowest when donor stromal tissue was eliminated. This finding is consistent with studies showing that the corneal endothelium may be relatively immune-privileged. As a result of these findings, a multicenter prospective randomized study has been initiated to determine if corticosteroid strength can be reduced after DMEK to avoid steroid-associated side effects without unduly increasing the risk of graft rejection.3138
Dry Eye, MGD
Oral azithromycin may be a useful therapy for treating meibomitis, particularly in patients who have failed traditional therapies, say researchers in San Francisco and Phoenix. They retrospectively reviewed the charts of 32 patients with meibomitis refractory to standard treatment who were given oral azithromycin (1 g orally once per week for three weeks) as part of their treatment regimen. Seventy-five percent of patients reported improvement in their symptoms at follow-up (average time, 5.6 weeks). Though all patients received concurrent steroid therapy, when controlling for those who had previously failed steroids, 64 percent still reported improvement. No significant adverse effects attributable to azithromycin were reported. The group proposes that, given oral azithromycin’s well-documented anti-inflammatory and antimicrobial properties and because its ocular pharmacokinetics allow for a much simpler and shorter dosing regimen than other frequently used medications, further investigation is warranted.606
Is there a relationship between signs and symptoms of dry-eye disease in a general patient population? Probably not, according to studies by a combined German/U.S. team, most of whom report commercial relationships to TearLab Corp. They retrospectively analyzed data from two cross-sectional observational studies, with seven tests for clinical signs and symptoms evaluated for 598 eyes in the general patient population (n=164 normal, n=434 dry eye) at 11 sites. Included were tear osmolarity; tear-film breakup time; Schirmer’s; corneal and conjunctival staining; meibomian gland dysfunction grading; and the Ocular Surface Disease Index questionnaire. From the data, they derived a full matrix of squared Pearson correlation coefficients of determination (r2) and an independent components analysis (ICA) mixing matrix.
No correlations above r2=0.20 were found between any of the signs or symptoms, except for corneal and conjunctival staining, which was r2=0.34. The average r2 for osmolarity (0.04), TBUT (0.12), Schirmer test (0.08), corneal (0.15) and conjunctival staining (0.16), meibomian grading (0.10) and OSDI (0.11) were consistently low. Similarly, each component of the ICA mixing matrix exhibited minimal residual information. Given that independent measurements are uncorrelated, the group concluded that each type of measurement reveals unique information about the status of the ocular surface. Overall, the clinical presentation of dry-eye disease is multifactorial, with each test contributing different information and no correlation between them.550
Dry-eye symptoms that persist despite improvement in objective signs that suggest successful treatment for meibomian gland dysfunction may be due to subclinical inflammation, according to researchers from several sites in Boston. Using in vivo confocal microscopy (IVCM), they imaged the cornea, palpebral conjunctiva and meibomian glands on five patients (mean age: 41.6 ±14.5) after treatment by LipiFlow (TearScience) for chronic MGD and related dry-eye symptoms. Images were analyzed for signs of inflammation undetected by slit-lamp exam. Two questionnaires were used to evaluate symptoms; the objective signs that improved post-LipiFlow were meibomian gland function and tear breakup time.
By IVCM, all patients had subclinical inflammation of the palpebral conjunctival epithelium, substantia propria, periglandular and intraglandular areas, as well as subepithelial conjunctival fibrosis. High inflammatory cell (IC) density in the conjunctival epithelium was associated with increased stromal IC density and periglandular inflammation. Three patients also had increased corneal density. The superficial corneal epithelia had heterogeneous epithelial cell size, increased hyperreflectivity and decreased cell density. Further, increased symptom severity was associated with decreased subbasal corneal nerve density, increased beading, hyperreflectivity and dendritic cell density. This ability to verify inflammation undetectable by slit lamp gives IVCM the potential to explain the presence of symptoms in the absence of obvious signs and, conversely, the presence of signs in the absence of symptoms, the group concludes. (Some of the researchers reported either employment by or commercial relationships to TearScience, the maker of the Lipiflow device.)594
A retrospective study of patients diagnosed with MGD and dry-eye symptoms who were treated with the LipiFlow Thermal Pulsation System shows evidence of restoration of MG function in previously non-functioning glands. (The authors report either employment by or commercial relationships to TearScience, the maker of the LipiFlow device.)
|
The increase in MGYLS from baseline to one month was significant, as was the increase in the volume index from baseline to one month (p<0.0001 in both cases). The changes from one month to 12 months were not statistically significant in either category.601
Rho kinase (ROCK) inhibitors have been shown to promote healing of endothelial cells in rabbit models. Scientists at various sites in Japan attempted to demonstrate the effects of a ROCK inhibitor eye drop, Y-27632, in a primate model. The endothelium of six cynomolgus monkeys (3 to 5 years-of-age; estimated equivalent human age: 15 to 20 years) was damaged by transcorneal freezing. Ten mM of Y-27632 was then applied topically in one eye of each animal six times daily, while buffered saline was applied in the fellow eye as a control.
By slit lamp, both Y-27632-treated and non-treated corneas became hazy after transcorneal freezing, and then recovered their transparency within four weeks. By specular microscopy, endothelial cell density was significantly higher in the Y-27632 group (3,123.7 ±82.4 cells/mm2) compared to the controls (1,833. ±90.8 cells/mm2) at four weeks (p<0.01). Although fairly normal-appearing, same-size hexagonal cells were observed in the Y-27632 eyes, a big variation in cell size and poorly formed cell junctions were observed in the controls by electron microscopy. The percentage of ZO-1 and Na+/K+-ATPase positive cells among the regenerated area in the Y-27632 group was significantly higher than in the controls (98.7 ±1.3 vs. 48.7 ±7.6 percent; p<0.05, and 100.0 ±0.0 vs. 76.6 ±2.0 percent, respectively; p<0.01). The group concludes that ROCK inhibitor Y-27632 promotes recovery of corneal endothelial cell density and wound healing in both morphology and function, and the eye drop might hold the promise of becoming a new pharmaceutical agent for treating corneal endothelial dysfunction.5999
Miscellaneous
After femtosecond laser-enabled keratoplasty, early suture removal within a year does not appear to affect visual acuity compared to sutures removed at later time points, say surgeons in Irvine, Calif. They analyzed 42 eyes of 42 patients who had had complete suture removal after FLEK. At surgery, seven eyes received eight combined interrupted sutures with a 16-bite running suture and the remaining 39 received a single 24-bite running suture with 10-0 nylon. All eyes had zig-zag pattern FLEK incisions. The early suture removal group comprised 18 patients whose sutures were removed between three and nine months postop; the late removal group, 24 patients whose sutures were removed from one to two years postop. Uncorrected and corrected VA and topographic delta simKs were measured six months after suture removal.
There was no significant difference in both uncorrected and BCVA between the early and the late suture removal groups (BCVA: 0.501 ±0.369 early vs. 0.544 ±0.424 late). Nor was there a significant difference in astigmatism between the groups (5.1 ±4.3 early vs. 3.9 ±2.5 late). However, a possible trend towards less astigmatism and less variability in the late suture removal group was observed. The group expects that larger numbers of eyes in the database with further enrollment will benefit astigmatism analysis.6055
A study at the University of Tsukuba, Tsukuba, Japan, suggests that polarization-sensitive OCT may noninvasively measure birefringence and detect the disruption of the lamellar arrangement in the keratoconic cornea, which is a prodrome to the development of morphological changes, offering the potential to evaluate keratoconus even before its development.
In 19 eyes of 19 normals, eight eyes of eight keratoconus suspects and 28 eyes of 19 patients with keratoconus, corneal thickness and regular and irregular astigmatism were obtained. Phase retardation tomography, which reflects birefringence of the cornea, was obtained by high-speed swept-source PS-OCT.
Phase retardations of the corneas were 0.64 ±0.53 radians in subjects with keratoconus; 0.32 ±0.15 radians in keratoconus suspects, and 0.24 ±0.17 radians in normal subjects. Corneal thicknesses were thinner in the patients with keratoconus. In the normal cornea, neither hyper-scattering nor strong birefringence was observed. Strong birefringence was found in keratoconus corneas.4123
Corneal surgeons at various sites in Cleveland and Atlanta used 3D anterior segment, spectral-domain OCT to create epithelial thickness profiles that they say can aid interpretation of corneal curvature changes after collagen crosslinking. They analyzed the corneal morphology of 17 eyes with keratoconus preop, and one and three months after crosslinking. A custom-written automated algorithm automatically segmented images based on intensity and gradient cues to produce 3D thickness profiles of the epithelial and stromal layers. Averaged epithelial thickness measurements were made at the corneal apex and 1.5 mm and 2 mm offset from the corneal apex.
Epithelial thickness in the keratoconus patients showed a standard deviation in the vertical axis ranging from 3.25 to 22.55 µm and from 2.72 to 15.98 µm in the horizontal axis. Epithelium was significantly thickened 1.5 to 2.5 mm below the corneal apex (p<0.001); thickness at the corneal apex was a mean ±STD of 49 ±13 µm preop, 51 ±5.0 µm one month postop, and 50 ±7.7 µm at three months. Preop averaged epithelial thickness measurements were statistically thinner at the corneal apex (p=0.017) and in the 1.5-mm (p=0.001)and 2-mm (p=0.007) offset locations compared to one month after crosslinking.95 REVIEW
Dr. Afshari is a professor of ophthalmology, director of Centers of Excellence, and director of Cornea and Refractive Fellowship at the Duke University Eye Center. She receives funding from Research to Prevent Blindness as well as the National Eye Institute.