If a surgeon could remove an appendix or unclog a coronary artery without breaking the skin, it would pay a lot of dividends: anesthesia risks would decrease; iatrogenic infection rates would drop to zero and the recovery period would be a lot easier, just to name a few. Though such surgery may sound like the stuff of science fiction, one femtosecond laser, the Femtec (20/10 Perfect Vision, Heidelberg, Germany), has been able to perform intrastromal treatments for refractive errors that leave the outside of the eye intact. Here's a look at preliminary results with this cutting-edge procedure.
Surgery Without a Trace
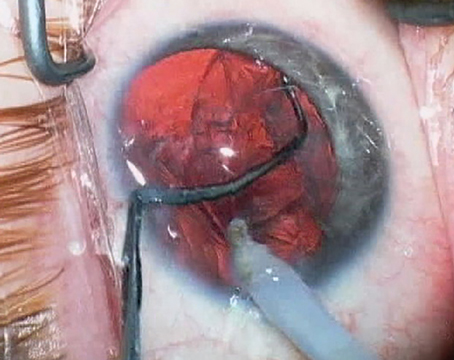
The Femtec treatment, performed primarily for presbyopia at this point, focuses the laser inside the stroma and makes a refractive change. No flap, epithelial debridement or side cut to remove a tissue lenticule is needed.
"It avoids the problems with a flap, and avoids the problems with surface ablation because we don't disturb the epithelium or Bowman's," says Luis Ruiz, MD, of
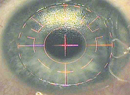
To perform the procedure, Dr. Ruiz enters patient data into the laser, including keratometry, hysteresis values, refraction and corneal thickness, "especially corneal thickness in the plane where we want to work," he says. The system then develops a photodisruption pattern for that patient. "The pattern is customized," says Dr. Ruiz. "It could change if the cornea is flatter, steeper, thinner, thicker, et cetera. It could also change depending on the preop refraction. If the patient is +1, it's different than if the patient is emmetropic or -1."
The thing all the presbyopic patterns have in common is multifocality, with the center treated for near and the periphery for distance. However, the size of the zones, the depth of photodisruption and the energy levels are currently proprietary, Dr. Ruiz says.
Femtec's maker says the laser's approach to fixation, which maintains almost all the cornea's natural curvature as opposed to applanating it flat, plays a role in the apparent efficacy of the procedure. "Both we and Dr. Ruiz think that a key aspect, from the perspective of predictability, is to treat the eye in its near-natural curvature," says Frieder Loesel, PhD, co-founder and chief technical officer of 20/10 Perfect Vision. "The Femtec uses a proprietary fixation approach with a curved patient interface. This interface is basically a sterile, disposable, curved contact lens that sits on the application end of the laser and is brought into contact with the eye and fixated with a suction ring. Instead of flattening it, the cornea's only mildly adapted to the curvature of the interface, so the ablations can be placed precisely in the three-dimensional volume of the stroma."
Preliminary Results
Dr. Ruiz has performed a study of 59 mostly emmetropic and hyperopic patients who have undergone the intrastromal procedure. In terms of uncorrected near vision, at one month postop, patients went from 0.28 ±0.17 (around 20/63 or J8) to 0.72 ±0.26 (around 20/25, or a little better than J3). The procedure was able to preserve uncorrected distance vision at one month, with not much of a change from a preop average of 0.77 (just under 20/25) to a one-month average of 0.88 (a little better than 20/25). Dr. Ruiz also measured patients' intermediate vision at a distance of 60 cm. "In decimal notation, it's usually between 0.8 and 1 [20/25 and 20/20]," he says. "We'll probably have to fine-tune it a little more as we see how patients change, but right now we're happy with it."
Five percent of the patients lost two lines of uncorrected distance vision, and another 5 percent lost three lines. Dr. Ruiz ascribes this to the learning curve of the procedure, and the initial need to fine-tune the photodisruption profile. "When we didn't know everything about the profile, we could get some patients who were corrected a little bit more than we wanted, maybe by 0.5 D or 0.75 D," he says. "And that's enough to lose lines of uncorrected distance vision. We've since made some modifications to the profile." No patients lost any lines of best-corrected vision at one month.
Dr. Ruiz says the patients' quality of vision has been good. "A number will have halos for one to one and a half months postop, but they don't complain about them," he says. "They will acknowledge them if you ask about it."
"My main question is about the stability," says Dr. Ruiz. "When I saw the first group of patients on the first day, they did very well, and I thought, 'Maybe they'll lose something by one week.' But when we saw them at a week, one month, two months and three months, they're the same as the first day postop. Obviously we need a longer follow-up, though."
The newest ablation profile Dr. Ruiz is working on is for myopic presbyopia, which is always a challenge since the patients already see acceptably at near and don't want to lose that, but want to improve their distance vision. "We're trying to modify the pattern a little," he says. "What we've been doing is selecting some patients with myopia and doing the presbyopic procedure on them after they have myopic LASIK. The ideal, though, would be to do it in just one step and correct both at one time."
Dr. Ruiz has also used the procedure on primary myopic and hyperopic and astigmatism cases, as well as post-LASIK eyes, post-RK eyes and pseudophakes.
"We've operated on a pseudophake with monocular IOLs and, after the 20-second intrastromal procedure, he saw 20/20 at distance and no worse than J2 at near," says Dr. Ruiz, who adds that the procedure is so innocuous some patients actually wonder if anything has been done. "It came to the point where we'd sometimes wonder what medication we could give to the patients for use postop so they'd feel as if they'd had something done, so we prescribe some very mild fluorometholone for use b.i.d. or t.i.d. for a week. Because we don't have a wound, there's no chance of infection, thin corneas aren't a contraindication unless it's actually keratoconus and we don't have to worry about dry eye postop. It's a very simple procedure."
For the myopes and hyperopes, Dr. Ruiz says they're taking small steps with the procedure. "At this moment, we're going little by little," he says. "We're working with myopia of 2.5 D or less and hyperopia up to 2.5 to 3 D. We'll have to study the procedure for two to three years, I'd say, to know its real limits."