 |
|
Allergy season is projected to begin sooner and last longer due to a warming climate, a study in Nature finds. (All Images: Getty) |
Allergy season is still upon us. It seems to grow longer and longer every year—and in fact, spring pollen emissions are projected to begin 10 to 40 days earlier and last five to 15 days longer in the summer and fall, according to a study published in Nature.1 That’s bad news for most allergy-sufferers, but it also means it’s never too late for a review of seasonal ocular allergy management. In this article, experts share their approaches to and tips for this irritating condition.
Artificial Tears
For mild ocular allergies, physicians usually begin with conservative treatments such as cold compresses or artificial tears. “Artificial tears can soothe mildly itchy eyes, and they also help flush off any allergens from the eye,” says Vatinee Bunya, MD, MSCE, co-director of the Penn Dry Eye and Ocular Surface Center and the William F. Norris and George E. de Schweinitz Associate Professor of Ophthalmology at the Scheie Eye Institute of Penn Medicine in Philadelphia. “I recommend that patients use artificial tears when they come inside to rinse their eyes. Chilling the artificial tears in the refrigerator is also soothing and can help with allergy symptoms. Preservative-free, non-viscous drops seem to work most effectively.”
One thing to counsel patients about is eye rubbing, says Dr. Bunya. “Eye rubbing worsens allergy symptoms because it triggers the eye to release histamines,” she says. “Eye rubbing starts a cycle of rubbing, itching and rubbing again. It’s key to not rub or touch the eyes at all. This is really difficult for patients, especially now with pollen counts rising every year.”
Topical Medications
 |
|
Timothy grass (Phleum pratense) pollen photographed by Bob Sacha. Timothy grass pollen is a common cause of hay fever, or allergic rhinitis. Experts say it’s important to avoid eye rubbing, which exacerbates itchiness and histamine release. |
If artificial tears aren’t sufficient to alleviate a patient’s ocular allergy symptoms, many clinicians turn to antihistamines or mast cell stabilizers, which work by antagonizing histamine receptors or preventing the release of histamines, respectively.
Prescription histamine-1 receptor antagonists include bepotastine besilate 1.5% (Bepreve, Bausch + Lomb) and emedastine difumarate 0.05% (Emadine, Alcon). Zerviate (cetirizine 0.24%, Eyevance) is the most recent addition to the prescription-only antihistamine offerings. It’s an H-1 receptor antagonist approved for b.i.d. dosing. In two Phase III studies, topical cetirizine administered 15 minutes or eight hours prior to a conjunctival allergen challenge model resulted in significantly lower ocular itching scores at all time points (p<0.0001) compared with vehicle. The researchers also observed lower amounts of conjunctival redness among cetirizine-treated eyes, and no safety concerns.2
Today there are more over-the-counter options available for ocular allergy than there were just a few years ago. Alcon’s formerly prescription-only trio Pataday, Patanol and Pataday Extra Strength (formerly Pazeo) are now available OTC. “These contain varying concentrations of olopatadine, a mast cell stabilizer,” says Soroosh Behshad, MD, MPH, an assistant professor of ophthalmology and chief of the Emory Eye Center at Emory St. Joseph’s Hospital in Atlanta. “The extra-strength formula contains 0.7% olopatadine hydrocholoride and is indicated for once-daily dosing. Pataday 0.2% is dosed once daily and Patanol 0.1% twice daily. Other OTC options include Zaditor (ketotifen fumarate 0.035%, Alcon) and Lastacaft (alcaftadine 0.25%, Allergan).”
“Cromolyn sodium 4% (Crolom, Bausch + Lomb) is an older mast cell stabilizer, but we sometimes use it if patients fail one of the other drops,” Dr. Bunya notes. Allergan’s Alocril (nedocromil 2%) is another option.
Steroids
In more severe cases with significant inflammation or for patients who don’t respond well to antihistamines or mast cell stabilizers, topical steroids such as difluprednate 0.05% (Durezol, Alcon) or loteprednol etabonate (0.2% Alrex, Bausch + Lomb) may be added to the management regimen.
“Steroids are always a short-term option [because of their possible side effects],” Dr. Behshad points out.
“I usually use a two-week steroid course, often paired with allergy drops,” says Dr. Bunya. “Steroids are useful for calming things down very quickly, which offers relief for the patient until the allergy drop’s full effect kicks in.”
Dr. Behshad says a pulse approach for one week can be helpful, depending on the severity of the allergy. “I may do a pulse approach with a mild steroid twice daily for a few days and then once a day for a few days and then stop,” he says.
Another steroid option for ocular itch comes from a familiar drug: Dextenza (0.4 mg, Ocular Therapeutix). Its labeling was recently expanded to treating patients with ocular itching associated with allergic conjunctivitis. The FDA update for the dexamethasone punctal insert was based on the results of three randomized clinical trials that found the implant lowered mean ocular itching scores compared with vehicle at all time points during a 30-day period with a favorable safety profile.
Systemic Allergy Medications
Systemic allergy medications such as Zyrtec, Claritin or Allegra may also provide patients with some relief, Drs. Bunya and Behshad say. “The only thing I usually warn patients about is that these medications tend to be drying,” Dr. Bunya notes. “For patients with dry eye, these medications may make dryness worse.”
Allergy Testing
 |
|
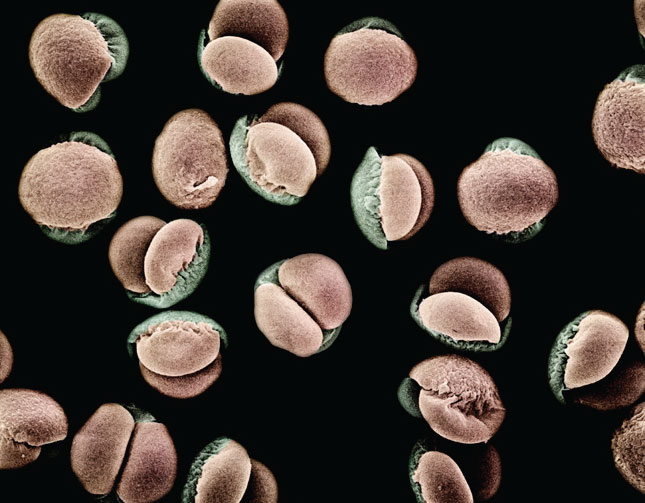
Mugo pine (Pinus mugo sp. uncinata) pollen grains under a scanning electron microscope at 280x magnification. (Photographed by Albert Lleal Moya.) |
If a patient’s allergies are very severe and aren’t responding well to topical medications, experts say the next step is to involve an allergist. “If the allergies are severe and recurrent, we try a team approach with an allergy specialist or maybe a dermatologist, depending on the patient’s condition,” Dr. Behshad says. “Number one is allergy testing to determine what exactly the inciting factor is and to see if it’s something that can be avoided. Allergy shots are also an option. These help to desensitize patients to prevent the symptoms from being a recurring issue.
“In the case of seasonal allergies, we can’t really avoid pollen altogether, so much of management involves being proactive and using some of the newer treatments available such as H-2 antagonists or combination mast cell stabilizers,” he continues. “These help not only with immediate relief but in preventing the allergic reaction.”
“Sometimes patients come in thinking they have seasonal allergies when it turns out they’re allergic to their dog or cat,” Dr. Bunya says. “I had one patient whose symptoms improved once she decided not to have her dog in her bedroom anymore. That alone helped her so much because she didn’t realize she was allergic to her dog. Allergy testing confirmed a dog allergy.”
An allergist should also be involved for treating cases of vernal keratoconjunctivitis, a rare and recurrent condition common among children, says Dr. Behshad. “Symptoms include itchy and painful eyes and light sensitivity,” he says. Treatment has traditionally involved topical medications, allergy drops and steroids, but there’s now an FDA-approved treatment specifically for VKC in children and adults: Verkazia (cyclosporine ophthalmic emulsion 0.1%, Santen). Verkazia is a prescription-only emulsion that inhibits T-cell activation and reduces the level of immune cells and mediators that cause allergic inflammation. “Having treatment options that don’t have [steroid] side effects for this population will be great,” Dr. Behshad says.
Contact Lenses for Allergies
Johnson & Johnson Vision recently launched Acuvue Theravision, the first FDA-approved drug-eluting contact lens for ocular allergy. Acuvue Theravision corrects vision and offers symptom relief with 19 mg of ketotifen in each daily disposable lens. The lenses are suitable for patients with 1 D or less of astigmatism. In the company’s Phase III clinical studies, the lenses demonstrated a statistically significant reduction in ocular itch at three minutes, with efficacy out to 12 hours. Importantly, the company notes that these lenses aren’t suitable for patients with red or irritated eyes.
In the Pipeline
Aldeyra’s novel small-molecule drug candidate for allergic conjunctivitis, Reproxalap 0.25% produced a decrease in ocular itching symptoms in clinical trials.
In the Phase III ALLEVIATE clinical trial (n=318), the two Reproxalap-treated groups’ (0.25% and 0.5% concentrations) ocular itch scores were significantly lower compared with vehicle after allergen exposure (p<0.0001). The drug also demonstrated a clinically significant response rate in ocular itch score that was statistically higher than vehicle at 20, 30 and 40 minutes (p<0.01) and at 50 and 60 minutes (p<0.05).3
Reproxalap is a reactive aldehyde species (RASP) inhibitor that’s intended to alleviate the symptoms of both dry eye and allergic conjunctivitis. The company says Reproxalap’s novel mechanism of action will fill a gap left by current therapies by having a longer duration of effect and no risk of steroid-induced side effects or increased dryness.
Dr. Bunya and Dr. Behshad have no relevant financial disclosures.
1. Zhang Y and Steiner AL. Projected climate-driven changes in pollen emission season length and magnitude over the continental United States. Nature Communications 2022;13:1234. [Epub March 15, 2022].
2. Meier EJ, Torkildsen GL, Bomes PJ, Jasek MC. Phase III trials examining the efficacy of cetirizine ophthalmic solution 0.24% compared to vehicle for the treatment of allergic conjunctivitis in the conjunctival allergen challenge model. Clin Ophthalmol 2018:12:2617-2628.
3. Clark D, Cavanagh B, Shields AL, et al. Clinically relevant activity of the novel RASP inhibitor Reproxalap in allergic conjunctivitis: The phase 3 ALLEVIATE trial. Am J Ophthalmol 2021;230:60-67.




