The Centers for Medicare & Medicaid Services last month granted New Technology Intraocular Lens designation to Bausch & Lomb's SofPort Advanced Optics ("AO") and SofPort Advanced Optics with Violet Shield Technology IOLs for their spherical aberration-reducing design. The NTIOL designation became effective March 6, 2007.
NTIOL designation means the Medicare reimbursement to ambulatory surgery centers for cataract surgery will increase by $50 when surgery is performed with either a SofPort AO or SofPort AO with Violet Shield Technology IOL. This NTIOL subset and adjusted payment for these two IOLs will remain in effect until February 26, 2011. The SofPort AO IOL is designed to be aberration-free and reduce spherical aberration for better vision quality compared to standard spherical IOLs. The SofPort AO with Violet Shield Technology IOL builds upon this design with a filter to block ultraviolet and violet light, which B&L says protects the retina from phototoxicity without compromising night vision or color perception. In order to gain inclusion in the NTIOL category, both lenses demonstrated the same or greater subset-specific clinical benefit as the lens that established the NTIOL subset.
Better Vision May Raise Risk in Elderly
Published studies have shown that cataract and other ocular surgeries reduce falls in elderly patients. A recent randomized, controlled study in
Researchers recruited 616 subjects aged 70 and older (mean age 81) mainly from people attending outpatient aged care services. The intervention group received comprehensive vision and eye examinations conducted by a study optometrist. The optometrist arranged for new eyeglasses for 92 subjects and referred 24 for a home visit with an occupational therapist, 17 for glaucoma management and 15 for cataract surgery. The control group received usual care.
Falls and fractures during 12 months of follow-up were ascertained according to self-report using a monthly postcard system. Fifty-seven percent of subjects fell at least once during follow-up. Falls occurred more frequently in the group randomized to receive the vision intervention (65 percent fell at least once; 758 falls) than in the control group (50 percent fell at least once; 516 falls). The falls rate ratio using the negative binomial model was 1.57 (p= .001). Fractures were also more frequent in the intervention group (31 fractures) than the control group (18 fractures; relative risk from proportional hazards model 1.74, p=.06).
Lead author Robert Cumming, PhD, professor of epidemiology and geriatric medicine at
"New glasses were the most common intervention in the study, and many of the subjects who received new eye glasses had major changes in their prescription," Dr. Cumming said in the study, published in the Journal of the American Geriatrics Society.
"This could explain the findings. Old, frail people may need a considerable period of time to adjust to new eyeglasses and could be at greater risk of falling during this time. Dr. Cumming's advice to those prescribing vision correction for such patients: "They should prescribe conservatively and give appropriate advice about the need for caution during adaptation to new eyeglasses."
Cumming R et al. Improving Vision to Prevent Falls in Frail Older People: A Randomized Trial. J American Ger Soc 2007;55:175–181.
POAG Costs Much Higher than OHT
A study presented at last month's American Glaucoma Society meeting lends economic evidence to the effort to prevent the progression from ocular hypertension to primary open-angle glaucoma. In the study, researchers from Harvard Medical School estimate that health-care charges are considerably higher for POAG than ocular hypertension even when controlling for age, index year, other demographics, treatment with intraocular pressure-lowering pharmacotherapy, co-morbidities and inflation. Opportunities for reducing condition-related charges associated with the transition from ocular hypertension to POAG and cost-effective treatment strategies should be explored.
In the study, the group determined the total and condition-related direct charges of patients with ocular hypertension or POAG and identified factors that affect these charges.
The study identified 36,767 ocular hypertension patients and 72,412 POAG patients with at least one year of continuous enrollment during calendar years 1998 to 2005 in a nationally representative, multi-managed health plan database. First-year total health-care and condition-related charges were calculated, and a multivariate linear regression model determined the impact of condition and treatment on these charges, while controlling for key covariates such as age, index year, other demographics and comorbidities.
Patients with POAG had significantly higher total health-care charges ($2,070 vs. $1,990, p< 0.0001) and condition-related charges ($556 vs. $322, p<0.0001) during the first year of follow-up than patients with ocular hypertension, even when controlling for key covariates. Female and older patients had higher total health-care charges ($586 or 28.3 percent more, p<0.0001) compared to males and younger patients ($27 or 0.8 percent per year more, p<0.0001). Neither gender (p=0.13) nor age (p=0.052), however, was a strong determinant of condition-related charges. Region, payer and product types significantly dictated total and condition-related charges. Patients with ocular co-morbid conditions including cataracts, cataract surgery, diabetic retinopathy and blindness had significantly higher total and condition-related health-care charges than patients without these conditions (p< 0.0001).
Louis R. Pasquale L, et al. Determinants of Healthcare Charges in Patients with Ocular Hypertension or Primary Open-Angle Glaucoma. Presented at the 2007 American Glaucoma Society meeting.
Indiana
Every year for more than a decade, Steve Gerber, MD, has offered a unique opportunity to doctoral residents in
This year's session was held on March 21 at the Bluth, Gerber & Schwartz Eye Care office, where Dr. Gerber is director of ophthalmology education for the family-practice residents. Approximately 50 residents from
The session grew out of Dr. Gerber's love for teaching. He realized that residents don't get to see or learn much in their two-week ophthalmic rotations, often dealing with cases of the same few conditions. Ophthalmology, he says, tends to fall by the wayside during training. Of family practice, Martin Wieschaus, MD, director of the residency program at St. Joseph Regional Medical Center, says, "It's a recognition of normal versus abnormal; defining abnormal, that's where our specialty help comes in." 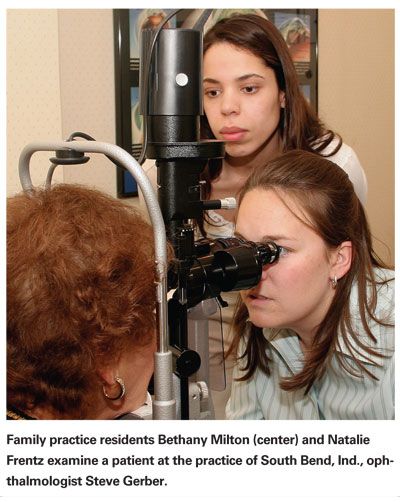
During their ophthalmic rotations residents typically see what Dr. Wieschaus calls "bread-and-butter stuff," cases like cataracts and blurry vision. "As a resident, you just see a lot of stuff that's just mundane. After two days it's old." To enhance and broaden the residents' learning, Dr. Gerber brings in patients with a variety of eye conditions for examination. "We're not seeing the cataracts and the person with astigmatism; we're seeing histoplasmosis in the eye, some herpetic dendrites, somebody with an alkali or acid burn," Dr. Wieschaus says.
"It's enhanced my ophthalmology experience," says Dr. Moeller. Like many involved with the event, she expresses her gratitude toward both the ophthalmologists and the patients for volunteering their time, and for letting the residents learn from them. Says Robert Riley, MD, the family-practice residency director at Memorial Hospital of South Bend, "It really is a great sacrifice these patients make."
ASCRS/ASORN Releases TASS-Prevention Guidelines
The American Society of Cataract and Refractive Surgery and the American Society of Ophthalmic Registered Nurses have released a Special Report, "Recommended Practices for Cleaning and Sterilizing Intraocular Surgical Instruments." The report was prepared by an ad hoc committee following outbreaks of toxic anterior segment syndrome (TASS), an acute inflammation of the anterior segment following cataract surgery.
The report implicates a variety of substances that may cause TASS. These include extraocular substances that inadvertently enter the anterior chamber during or after surgery (topical anti-septic agents, preservatives and others), and irritants on the surfaces of intraocular surgical instruments that accumulate due to inadequate or inappropriate instrument cleaning. The report recommends practices for cleaning and sterilizing intraocular surgical instruments, as well as adminstrative steps that practices may take regarding staff education. Appropriate for all facilities performing cataract surgery, the practices derive largely from existing, evidence-based general recommendations for cleaning and sterilizing surgical instruments and from directions for management of equipment provided by manufacturers. To view the full report, visit ascrs.org.



