Alcon Infiniti
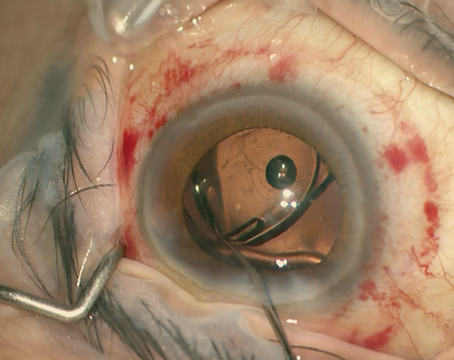
Alcon Infiniti The most recent addition to Alcon’s Infiniti system is OZil Intelligent Phaco, or IP. The original OZil consisted of an oscillating side-to-side motion by the phaco tip. The idea behind this movement was to cut lens material, avoid repelling lens fragments and to emulsify lens material on both ends of the motion. However, surgeons found that sometimes it’s actually a good idea to push material away a little bit in order to avoid clogging the phaco needle. “If you’re using pure torsional, it’s easy to clog the needle,” says Tucson, Ariz., surgeon William Fishkind. “This is because there isn’t much cavitation at points where the needle narrows, such as the hub.”
With OZil IP, the surgeon sets a certain vacuum threshold that will signal to the machine there’s the risk of a clog. Then, when that vacuum threshold is reached during surgery, the OZil IP system sounds a tone and adds a measure of back-and-forth longitudinal phacoemulsification energy to the OZil’s normal torsional movement, clearing the potential clog with cavitational energy. “OZil torsional phaco was a great boon to us,” says Southlake, Texas, surgeon Robert Lehmann. “It rises to only a third of the temperature of traditional ultrasound and is more efficient at cutting nuclear material. Now with IP, you never come to a complete occlusion, because the IP system will kick in just enough longitudinal movement to break any occlusion or pre-occlusion state. As a result, you get a much more stable anterior chamber. The old trampolining that you used to see with peristaltic pumps just doesn’t occur. With average cases, I’ve found the OZil IP’s ease of cutting makes things go smoother. And on the harder cataracts—where we had to be concerned with clogging and thermal issues—such concerns are greatly lessened.”
Jason Jones, MD, of Sheldon, Iowa, says using OZil IP can help make surgery more efficient. “If you do chopping, you may want to hear the IP activation signal as you place your tip in the nucleus for the first chop,” he says. “That means you’re achieving a fairly high vacuum level, which is what you want to hold the piece. If you do a grooving technique and you get IP activation, that avoids getting an occlusion and causing problems, and you may realize you need more phaco energy to avoid reaching that higher vacuum level again, and so you can keep your tip clear.
 “The same issues apply if you’re taking out a piece,” Dr. Jones continues. “If you’re hearing the IP activation, then you can train yourself to respond to it; you can put your foot down farther in foot-position three to use more energy to keep the tip clear. The extra energy will help keep your tip clear and avoid getting an occlusion. At the beginning of the surgery, we all have a sense, based on our grading of a cataract, whether it will be dense or mild. But, sometimes, there will be a cataract that surprises us by how dense it is. You can get a sense of this density by the IP activation. If you have a lot of IP activation, it prevents you from getting an occlusion because it will push the piece away and let you reacquire it at a different tissue interaction face.”
“The same issues apply if you’re taking out a piece,” Dr. Jones continues. “If you’re hearing the IP activation, then you can train yourself to respond to it; you can put your foot down farther in foot-position three to use more energy to keep the tip clear. The extra energy will help keep your tip clear and avoid getting an occlusion. At the beginning of the surgery, we all have a sense, based on our grading of a cataract, whether it will be dense or mild. But, sometimes, there will be a cataract that surprises us by how dense it is. You can get a sense of this density by the IP activation. If you have a lot of IP activation, it prevents you from getting an occlusion because it will push the piece away and let you reacquire it at a different tissue interaction face.”
The Infiniti system also allows the surgeon to program up to four different grades of cataract and different machine parameters for each. When it goes up a grade, for example, the machine can be programmed to increase aspiration flow rate, vacuum and bottle height. It can also modify the power modulations on the OZil handpiece. “You can also change your threshold presets for any parameters that are linear,” explains Dr. Jones. “In other words you can start off at a different threshold, based on what you think the cataract will require. In this way, you waste less flow of fluid through the eye, and waste less time and energy at those lower levels of fluidics and power.”
Alcon has also introduced a disposable polymer I/A tip as an alternative to the reusable silicone tip. Though Dr. Lehmann says he still uses the silicone tip routinely because it’s reusable, the advantage of the polymer tip comes into play when dealing with certain phases of the cataract procedure. “If you have a nuclear remnant or epinucleus that’s fairly moderate or firm, if you were using a silicone I/A tip you might have to use an instrument to crush it into the tip,” he explains. “But with the polymer I/A tip you can go to a higher vacuum level and the tip will draw the nuclear remnant in a little more readily.”
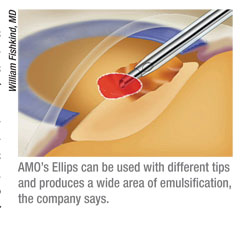 |
AMO initially enhanced the cutting efficiency of its Whitestar Signature system by offering Ellips ultrasound, which blends longitudinal ultrasound with transversal ultrasound in an effort to avoid clogs while still emulsifying lens material. In the past year, however, the company added a wrinkle to its Ellips ultrasound called Ellips FX. “The Ellips used to alternate frequencies as it operated,” says Dr. Fishkind. “Now, it’s been redesigned to work at the same frequency throughout: 38Khz. This makes it more efficient in terms of removing different types of nuclei.” The company says FX also results in a larger area of emulsification.
The second innovation is non-zero start. “When you push down on the foot pedal in foot-position three, the machine can start at whatever power you want,” explains Dr. Fishkind. “You don’t have to go through 10, 15, 20 then 25 percent; if you have a harder cataract you can start at 30 percent and get right to it. So, there’s less time spent getting to the power you want and this makes the system more efficient, since it comes on right where you want it to be. This also seems to improve followability significantly.” Dr. Fishkind says these changes have affected how he approaches cases. “With softer cataracts, you can rely more on aspiration and use phaco power almost as if it were phaco-assisted aspiration,” he says. “With harder cataracts, you can choose the tip that you like because the elliptical movement of the Ellips FX isn’t dependent on the phaco tip. So with non-zero start and highly controllable fluidics, removal of harder nuclei is more efficient since the device can hold the nucleus at the tip without allowing occlusive surge and instead fosters a steady, slow emulsification of the material.
“What I find with the AMO machine,” Dr. Fishkind continues, “is that you can dissect the nucleus surgically. So it makes it easy to remove the endonucleus with chopping procedures because the aspiration is so controlled; it’s easy to chop a nucleus into fragments and then remove a fragment with just slightly higher vacuum and flow levels. It allows precise control over the material you’re emulsifying in the anterior chamber. You can also chop nicely because you can use burst power to get into the nuclear material and hold it to do vertical chop. I do vertical chop currently, which I think is a more gentle, controlled way to remove the nucleus. The Whitestar Signature system facilitates such chopping techniques.”
AOI Vizual
The second innovation is non-zero start. “When you push down on the foot pedal in foot-position three, the machine can start at whatever power you want,” explains Dr. Fishkind. “You don’t have to go through 10, 15, 20 then 25 percent; if you have a harder cataract you can start at 30 percent and get right to it. So, there’s less time spent getting to the power you want and this makes the system more efficient, since it comes on right where you want it to be. This also seems to improve followability significantly.” Dr. Fishkind says these changes have affected how he approaches cases. “With softer cataracts, you can rely more on aspiration and use phaco power almost as if it were phaco-assisted aspiration,” he says. “With harder cataracts, you can choose the tip that you like because the elliptical movement of the Ellips FX isn’t dependent on the phaco tip. So with non-zero start and highly controllable fluidics, removal of harder nuclei is more efficient since the device can hold the nucleus at the tip without allowing occlusive surge and instead fosters a steady, slow emulsification of the material.
“What I find with the AMO machine,” Dr. Fishkind continues, “is that you can dissect the nucleus surgically. So it makes it easy to remove the endonucleus with chopping procedures because the aspiration is so controlled; it’s easy to chop a nucleus into fragments and then remove a fragment with just slightly higher vacuum and flow levels. It allows precise control over the material you’re emulsifying in the anterior chamber. You can also chop nicely because you can use burst power to get into the nuclear material and hold it to do vertical chop. I do vertical chop currently, which I think is a more gentle, controlled way to remove the nucleus. The Whitestar Signature system facilitates such chopping techniques.”
AOI Vizual
American Optisurgical’s Vizual system is a lightweight (22 lbs.), portable unit that the company says is aimed at cataract missions in foreign countries that need a portable machine, as well as surgical centers that are looking to control per-procedure costs; to keep the cost per case down, the system uses reusable tubing and tips, rather than disposable ones.
The Vizual, which has a peristaltic pump, uses a 40-kHz handpiece that has the option of using burst and micropulse phaco. “The micropulse phaco divides the energy pulses into pulses of a set millisecond duration,” explains AOI’s President, Herbert Cameron. “The surgeon can control the on and off time of the pulses. This is engineered toward maintaining a cool incision site.” In burst mode, the surgeon can extend the duration of a pulse, making it wider until eventually it becomes continuous.
To keep the surgeon from having to alter power and fluidics settings throughout the procedure, the Vizual also offers multi-modulation, or the ability to define three phaco modes that each have different phaco settings, such as burst or micropulse. “A surgeon might use phaco 1 for sculpting, phaco 2 for cracking and phaco 3 for quadrant removal,” Mr. Cameron explains. The system also allows 24 different users to save their mode settings.
To help avoid surge, the system uses an anti-surge system built into the software that controls the ramp up and ramp down of the peristaltic pump. The system can be adjusted to provide between 0 and 50 cc/minute of flow, and the surgeon can adjust the vacuum from 0 to 500 mmHg.
Bausch + Lomb Stellaris
Though the Stellaris system has featured various innovations over the past several years, surgeons say it’s real claim to fame is the ability to allow sub-2 mm incision surgery. Specifically, it can be used for 1.8-mm coaxial micro-incision surgery, or 1.8-mm CMICS.
Terence Devine, MD, of Sayre, Penn., helped develop the Stellaris system, although he no longer consults for Bausch + Lomb. He says that, even if he has to enlarge the 1.8-mm cataract incision to implant an intraocular lens, he still appreciates the benefits of sub-2 mm surgery.
“The smaller needle and sleeve really do make a difference in visibility and maneuverability during surgery,” Dr. Devine says. “You can not only better see what you’re doing, but if you’re using a divide-and-conquer technique, for example, it’s much easier to perform it with a smaller needle and a smaller sleeve. You can sculpt a very thin groove and get down to the base of it and that makes the cracking easier.
“We face intraoperative floppy iris cases on a daily basis, and a lot of surgeons will use some sort of iris hooks or retractors on them, but I never use them,” Dr. Devine continues. “I can get through these small pupils with the 1.8-mm CMICS technique. I also see post-RK patients these days. One of the problems with performing a phaco on someone who has had RK is that the incisions never fully heal and regain full strength. So, with phaco, there’s a risk of inadvertently spreading one of the RK incisions, resulting in induced regular or irregular astigmatism after the cataract procedure. But with the CMICS 1.8-mm surgery, I can go between the incisions. The same thing is true with sutures in a patient who has had keratoplasty.”
Dr. Devine thinks the smaller CMICS needle and sleeve allow the system’s fluidics to be more tightly controlled. “By this, I mean the challenge with any machine is to maintain chamber stability,” Dr. Devine avers. “So, whatever in the way of fluid and material is being removed from the eye via aspiration needs to be replaced with the infusion, and I believe that that balance is maintained better with 1.8-mm CMICS. I did a computer search of all my cases from my first CMICS case in October 2006 through May 2010, and found 6,846 cases. And I only had one broken capsule in all that time.” To increase the infusion with such small ports, the Stellaris uses a system called DigiFlow, which pressurizes the infusion bottle with a digitally controlled air pump. The surgeon sets the actual bottle height, but then dials up a certain amount of air pressure that will create pressure as if the bottle were set higher.
To control the ultrasound energy being used in the eye the Stellaris uses the Attune Energy Management system, which cycles the ultrasound energy on and off as quickly as every 2 ms. The power modes include pulse, burst, fixed burst, multiburst and continuous. It can also produce energy that conforms to square wave or waveform pulses. With the former, the energy hits the highest amount instantly and then decreases just as quickly. With the alternative, waveform approach, the power builds gradually during the duty cycle to a pre-set limit, and then drops quickly to baseline.
Staar Surgical Sonic Wave
The Sonic Wave is the only phacoemulsification system that allows users to dip into the sonic frequency range when emulsifying a cataract. By using the device’s foot pedal, the surgeon can use low-frequency energy of between 40 and 400 Hz to help break up the lens more efficiently. When paired with the device’s fluidics system, the company says the Sonic Wave can use much less energy than an instrument that uses all ultrasonic energy. The company also says sonic energy doesn’t risk wound burn, require an irrigation sleeve or churn up turbulence in the anterior chamber.
Staar also uses a special filtering system called Cruise Control to limit post-occlusion surge. Since the filter traps nuclear material and only allows fluid to pass, Staar says flow is kept at an even level and that extremely high flow rates, the kind that can cause anterior chamber collapse, are eliminated.
Ocusystem Advantage
The Ocusystem Advantage features a dual-linear footswitch and a fluid venting system that William Banko, MD, Surgical Design’s president, says makes for excellent surge protection.
The Advantage vents to a second fluid-filled chamber that’s higher than the infusion fluid to help prevent surge. Dr. Banko says this surge- prevention feature is most noticeable during the irrigation/aspiration of cortex, when there’s no epinuclear shell keeping the capsular bag expanded. He says the dual-chamber venting is helpful because, rather than slowing aspiration by ramping down pump speed or avoiding complete occlusion, the Advantage’s venting method doesn’t compromise the system’s effectiveness, or the surgeon’s ability to work safely at high vacuum levels.
The system’s reversible dual linear footswitch has both vertical and linear functions, and can be programmed to map vacuum and flow to the vertical axis and ultrasound to the horizontal, or to map ultrasound and vacuum control on the vertical axis and flow on the horizontal. Dr. Banko says that the former is better for removing lens material and the latter is better for capsule management (combined with the system’s gravity-driven infusion and outflow and its ultrasonic I/A).
The audible feedback tones on the device are very precise, Dr. Banko says, rising smoothly as the vacuum in the aspiration line rises and beeping when it reaches the preset vacuum limit that the surgeon has chosen. “I can hear the difference between aspiration of BSS, viscoelastic and vitreous,” he says.