It should come as no surprise that medical technology has found a platform on our mobile devices. Smartphone use in clinical practice is growing,1 and applications that can save surgeons time and money are also helping improve patient outcomes. Here, we’ll take a look at some of the recent advances.
Panacea IOL Calculator
The Panacea IOL and Toric Calculator is a multi-program ophthalmic application created by David Flikier, MD, medical director of the Instituto de Cirugía Ocular in San José, Costa Rica. Panacea considers two new corneal variables, the Gullstrand ratio (posterior-to-anterior corneal ratio) and corneal Q asphericity, which Dr. Flikier says increase predictability in normal cases and also allow for the calculation of abnormal corneas with objective data.
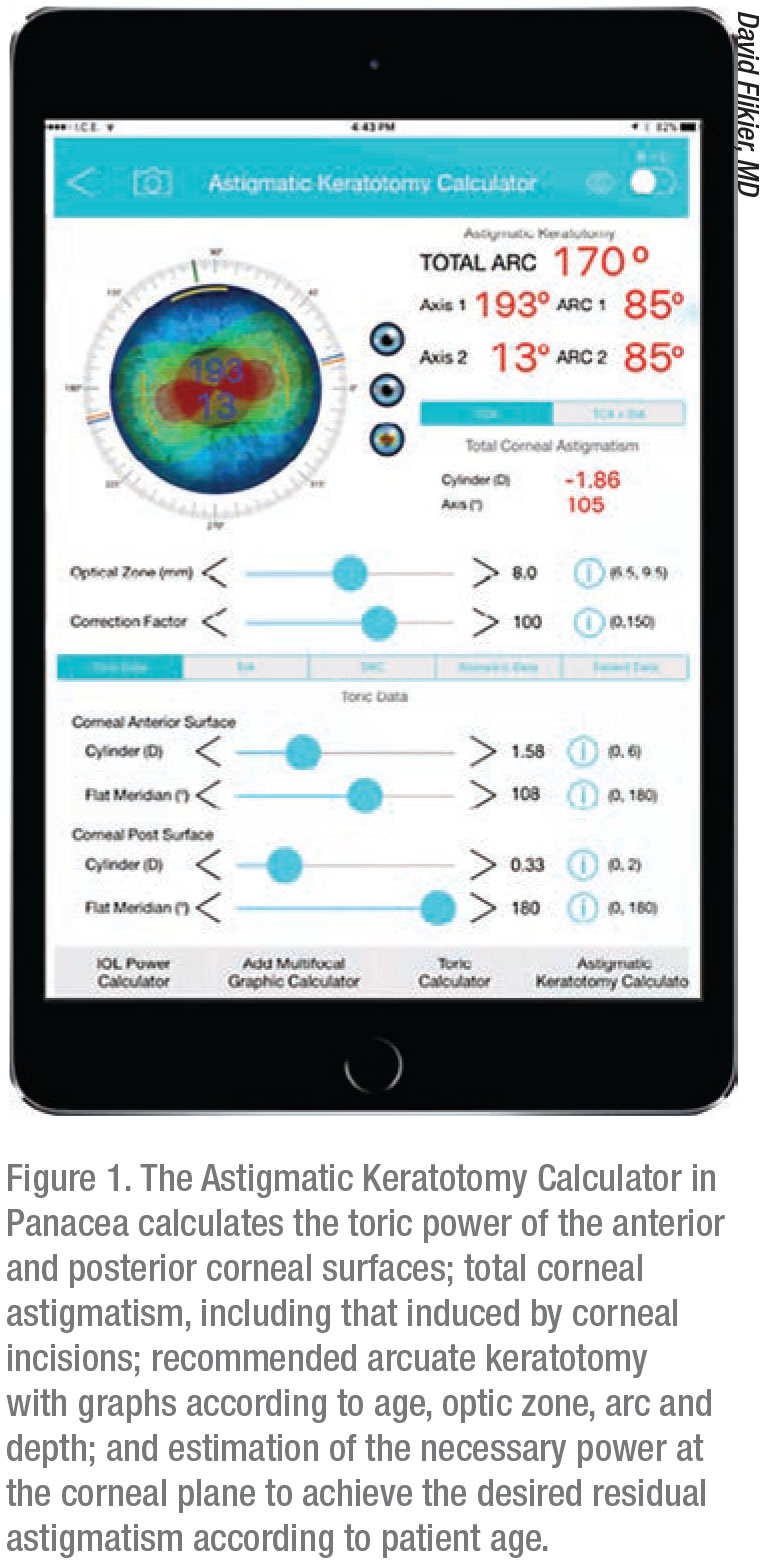 |
Dr. Flikier says he designed Panacea to be intuitive and easy to use. The app features 19 programs, including:
• “IOL Power and Toric Calculator.” This includes calculators for surgically induced astigmatism, postop toric calculation, Holladay and SRK/T anterior chamber depth calculation and astigmatic keratotomy calculation;
• “Aphakic/Phakic Calculator.” This allows both aphakic and phakic IOL calculation, posterior chamber intraocular phakic lens diameter and LASIK and PRK ablation thickness calculators; and
• “Optometric Formulas Calculator.” This includes calculators for toric contact lenses, prism, vertex distance and abbe value.
“I’m very impressed with the Panacea software for IOL calculations,” says Arturo Chayet, MD, of the Codet Vision Institute in La Jolla, California. “In my opinion it’s the most complete, effective but underrated IOL calculator. I’m using it with great success.”
Luis Lu, MD, senior member of Eye Consultants of Arizona and preceptor at Arizona State University and Hyatt Medical Education, International University, agrees. “I use the program to compare the calculations done with the other fourth-generation formulas that are available,” he says. “In normal corneas, in a few cases the calculation can change a little, but my main use is on those with previous corneal surgeries. I believe this ‘fifth’-generation program should be used in conjunction with the other formulas to improve the outcome of the target refraction. Panacea can calculate the toricity well, perhaps because it includes factors or vectors not included in other programs.”
Dr. Lu says the Panacea formula works well in all kinds of eyes, so long as the individual’s posterior corneal power can be measured. This is where the advantage of Panacea lies, says Dr. Flikier. “To really get the advantage of Panacea, you need to introduce the posterior surface data through the Gullstrand ratio or posterior surface curvature,” he explains.
While the app features several calculators and variables, “it does require the surgeon to be able to calculate the power, radius and axis of the anterior and posterior cornea,” Dr. Lu says. One improvement he suggests is that “the data from the Pentacam, Galilei G4 or G5, IOLMaster 700 or any device capable of measuring the total corneal power be directly integrated into the program.” He hopes that in the future more variables will be taken into account, such as aqueous index of refraction, vitreous index of refraction, lens tilt and retinal tilt.
A 2017 study comparing methodologies using estimated versus measured values of total corneal astigmatism for toric IOL power calculations found that the centroid prediction error, the error in the predicted mean of residual astigmatism for a series of patients, was 0.25 ±0.43 D at 173° for the Panacea calculator.2
The latest results of a 2019 study headed by Filomena Ribeiro, MD, PhD, FEBO, director of the Ophthalmology Service of the Hospital da Luz Lisboa and professor of ophthalmology and biomedical engineering at the University of Lisbon, found Panacea calculated a mean absolute error of intended versus achieved refraction of 0.291 D for the Alcon SN60WF and 0.305 D for the Johnson & Johnson PCB00.3
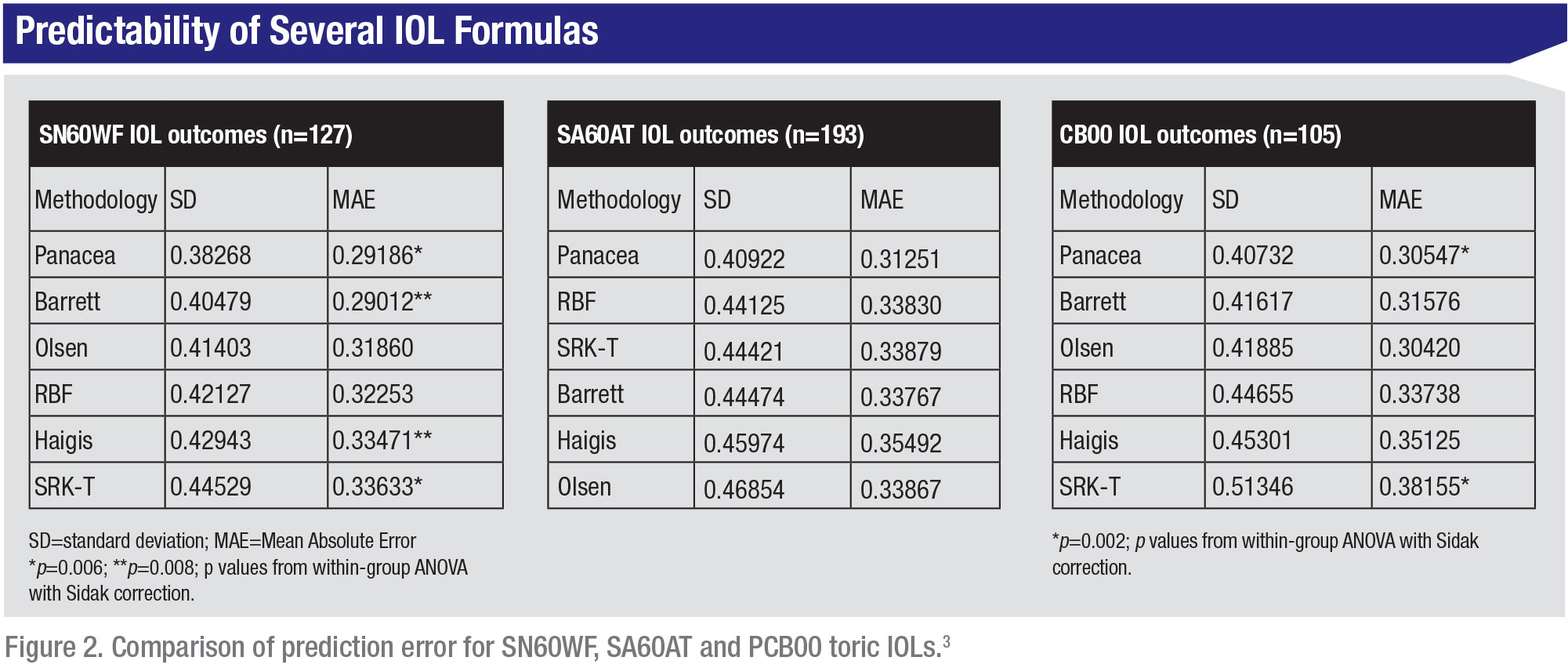 |
| Image courtesy of Filomena Ribeiro, MD |
Dr. Lu finds that his refractive outcomes have improved with Panacea. “Prior to this program, about 70 to 75 percent of my patients were within 0.5 D of the target refraction and 85 to 90 percent within 1 D. With the use of Panacea as a comparative formula, my results are 85 percent within 0.5 D.”
The Panacea app is currently available for iPad, as well as for desktop Macs and PCs. Android and iPhone versions are in the works. For more information, visit panaceaiolandtoriccalculator.com.
iToric Patwardhan
The iToric Patwardhan is an axial marking tool that checks the accuracy of toric marking and suggests a new placement axis to reduce error in IOL placement. There’s no need for a slit lamp or bubble marker. All the app requires is an Android smartphone with a good camera.
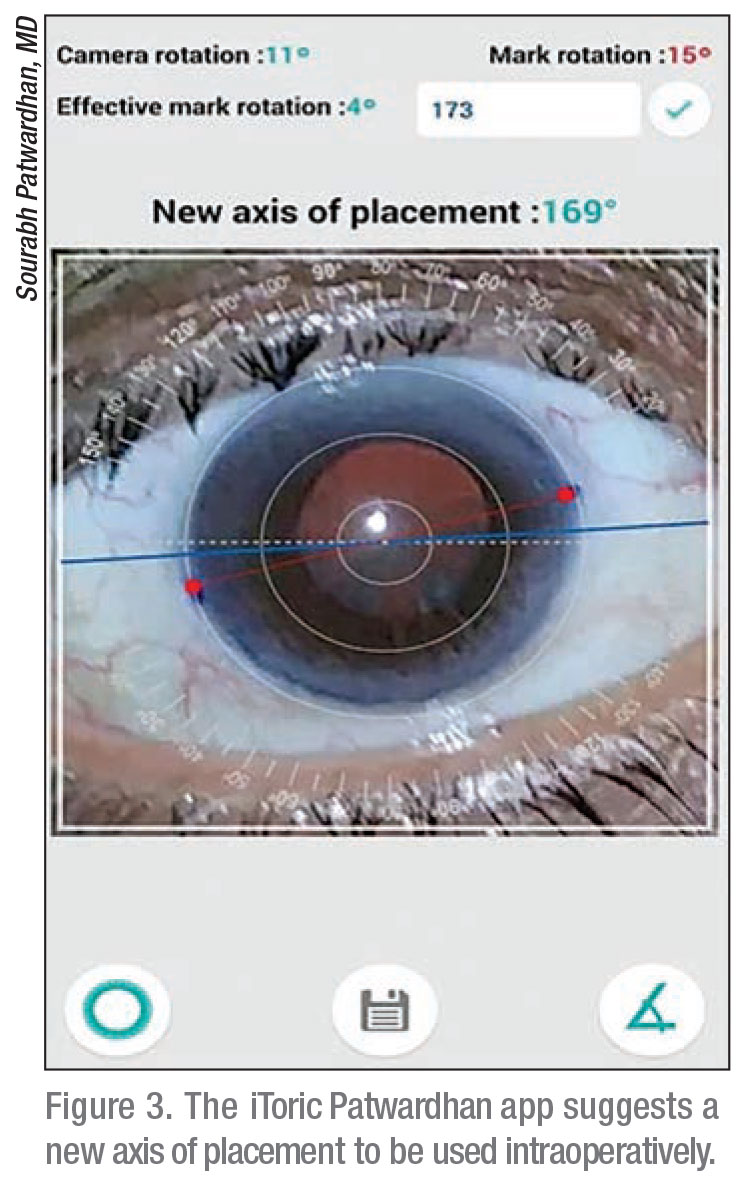 |
iToric Patwardhan was developed by Sourabh Patwardhan, FRCS, MD, medical director at India’s Nandadeep Eye Hospital and Institute. Using the smartphone’s built-in gyroscope, which can measure angular acceleration, iToric can pinpoint the exact orientation of a mark in space within 1 degree of precision.
After taking a photo of the eye, the surgeon can zoom in and align the cornea within the outer calibration circle in the app. Once the eye is centered, the user places the marks on the cornea and enters the placement axis. The app will then suggest a new placement axis to correct any error in marking.
In Dr. Patwardhan’s experience, the iToric resulted in a decrease of average residual cylinder from 32 to 22 percent and, in 87 toric IOL cases, none of them was more than 5 degrees away from its intended axis.
The quick workflow, high accuracy and opportunity to avoid additional calculations are the main advantages of the app, says Dr. Patwardhan. “Patients are much more comfortable with freehand pen marking,” he notes. “Children are also more cooperative with this than with metal toric marking instruments.”
Vinit Shah, MD, who practices at the Vinit Eye Clinic Retina and Laser Centre in Mumbai, India, agrees, saying, “iToric is very good in a busy operation theater where it might be difficult for surgeons to come out of the OT after every case to perform corneal marking at the slit lamp with bubble markers. This even helps the patient, as the process is fast and less cumbersome.”
Zain Khatib, MD, in practice at the Khatib Eye Clinic, Mumbai, has been using iToric for more than two years. “You can capture a photograph and then align the marks with the calibration circles later,” he says. “This is much more stable and easier to perform than working with real-time apps.”
“Accuracy-wise, it’s excellent,” Dr. Khatib says. “iToric almost matches the accuracy of a digital marking system.”
A 2018 study supports this conclusion. Compared to manual marking methods, preoperative marking with smartphone gyroscope-assisted marking significantly improved accuracy.4
For a tutorial, watch this video: youtu.be/vHKrFGimkHw. Visit play.google.com/store/apps/details?id=com.itoric.app1 to download the app.
Eye Pro
Eye Pro is a suite of programs for iOS that performs calculations such as post-LASIK biometry, vector astigmatism analysis and outcome analysis. Edmondo Borasio, MD, FEBO, Head of the Ophthalmology Department at Burjeel Day Surgery Center in Abu Dhabi and creator of the Borasio Edmondo Smith and Stevens (BESSt) formula,5 developed Eye Pro in 2009, and he says it was the first ophthalmological app released for iOS. The current version includes standard biometry formulas like SRK/T and Hoffer Q, the BESSt formulas for post-refractive surgery patients,5 and toric IOL and SIA calculators. It also includes an aggregate astigmatism plotter, optical formulas and converter programs for visual acuity notation, corneal to spectacle plane and Cartesian (x,y) to polar (r,θ) notation, which describes a point in terms of distance from and angle of rotation around a point.
 |
“You can bring it with you to the operating theater to recheck biometries on the spot,” says Dr. Borasio. “I also often use it in the clinic to perform post-laser refractive surgery biometries using BESSt 2 and Borasio Myopic/Hypermetropic Regressions (BMR/BHR),6 or for toric IOL calculations and for converting visual acuity notations.”
Surgeons say that Eye Pro’s ability to analyze multiple patient data sets at once has helped them see important trends in their work. “Being able to see aggregate plots of pre-, post- and induced astigmatism and the centroid calculation was an eye-opener that helped me to modify my surgical technique based on my results,” says Eduardo Viteri, MD, of Centro Oftalmológico Humana Vision, Ecuador. “I changed from a steeper axis to temporal incisions and was able to take into consideration the vector effect of my 2.2-mm incisions to decide on the IOL axis alignment.”
For a series of cases, Dr. Viteri explains, “you can easily obtain the mean astigmatism and standard deviation, after conversion to Cartesian notation; plot two series simultaneously on the same plot—for example, pre- and postop; and plot the astigmatism centroid.” The SIA plotter produces high-resolution, publication-level, double-angle polar plots, says Dr. Borasio.
Charles Diaper, MD, an oculoplastic surgeon with a general cataract practice in the National Health System in Scotland, says Eye Pro’s astigmatism plotting and group outcome analysis came in handy when he needed to generate audit output data for his department to show they were matching national audit benchmarks for surgically induced astigmatism. Dr. Diaper says his plots showed a change in incision width from 4.2-mm incisions to 2.2 mm, a decrease linked to a reduction in SIA,7 which helped maintain his department “when management wished to constrain resources.”
Both Dr. Viteri and Dr. Diaper find the app easy to use, but point out the ever-present possibility of data input error. “For individual cases, the data input is intuitive,” Dr. Viteri says. “You just have to be careful. I suggest using a positive cylinder notation to avoid confusion.”
Though the app’s portability on iPads and iPhones is convenient, especially when the surgeon, as Dr. Diaper puts it, “is away from biometry machinery,” Dr. Viteri says he’d like to be able to use Eye Pro on his computer to make data transfer easier. “It can be a little cumbersome to export and import the .cvs files to obtain the centroid and polar plots, but it’s worth the effort,” he says. “Having it on my computer would just make data transfer easier for aggregate vector analysis in astigmatic correction.
“It would be great to have Eye Pro integrated with Pentacam AXL to take the back of the cornea into consideration, avoid data input error and improve efficiency,” continues Dr. Viteri. “I’d also like to be able to take or import anterior segment photographs for axial marking.”
While Dr. Viteri doesn’t use Eye Pro routinely, instead sticking with Goniotrans, a virtual angle conveyor for axial marking, and a Pentacam AXL for biometry and IOL calculation, he still considers Eye Pro a “must have” for cataract surgeons looking to improve their refractive results.
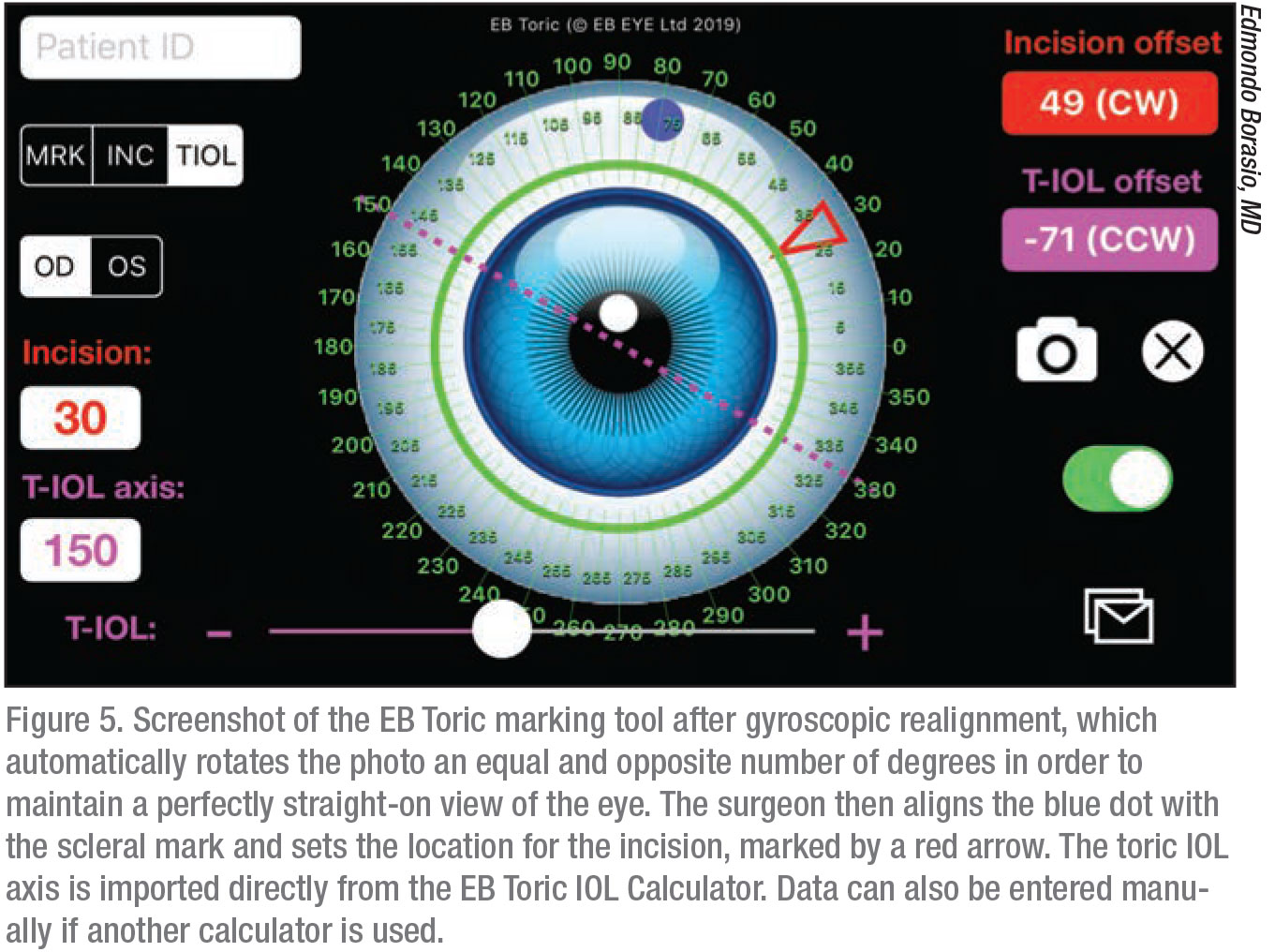 |
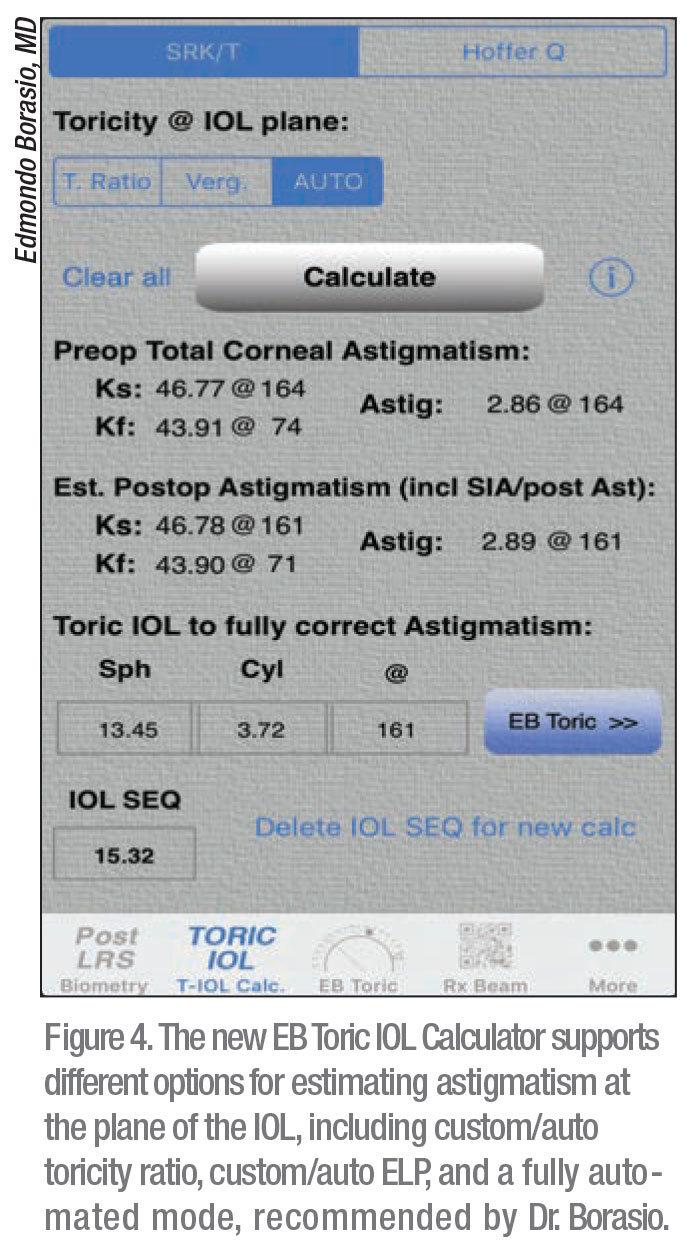
The latest release of the app contains three new features: a streamlined prescription app; a toric IOL calculator that supports posterior corneal astigmatism as well as Naeser/Savini Optimized Keratometry regressions and different options for estimating the astigmatism component at the IOL plane, including toricity ratio and effective lens position; and a new method of toric marking. The EB Toric marking tool employs a speculum and an ink mark applied anywhere on the sclera to orient the iPhone. A photo is taken, realigned by gyroscope, and digital marks can be added.
Comparing digital toric marking to direct marking, Dr. Borasio says it’s fast, inexpensive, convenient and safe, since there’s no need to unpack sterile instruments and there’s no risk of corneal abrasions.
For more information or to download a free trial of the new release, visit eb-eye.com. REVIEW
1. Karthikeyan SK, Thangarajan R, Theruvedhi N, Srinvasan K. Android mobile applications in eye care. Oman J Ophthalmol 2019;12:2:73-77.
2. Ferreira TB, Ribeiro P, Ribeiro F, O’Neill JG. Comparison of methodologies using estimated or measured values of total corneal astigmatism for toric intraocular lens power calculation. J Refract Surg 2017;33:12:794-800.
3. Ribeiro F, et al. Hospital da Luz Lisboa. 2019. [Submitted]
4. Khatib Z, Haldipurkar S, Shetty V, Setia M. Verion vs manual marking and smartphone-assisted manual marking in toric IOL implantation. September 23, 2018. Vienna 2018 36th Congress of ESCRS. Laxmi Eye Institute, Navi Mumbai. [pending publication]
5. Borasio E, Stevens J, Smith GT. Estimation of true corneal power after keratorefractive surgery in eyes requiring cataract surgery: BESSt formula. J Cataract Refract Surg 2006;32:2004-2014.
6. Borasio E. IOL power calculation accuracy in post-myopic and hyperopic ablations using the Borasio Regression formula. March 2011. ASCRS Annual Meeting. San Diego.
7. Masket S, Wang L, Belani S. Induced astigmatism with 2.2- and 3.0-mm coaxial phacoemulsification incisions. J Refract Surg 2009;25:1:21-24