Since the first successful full thickness corneal transplantation was performed by Eduard Zirm in 1905,1 the procedure has grown to become the most commonly performed transplantation globally. In the last 20 years, the field of corneal transplantation has been revolutionized by the development of partial-thickness transplantation techniques allowing less invasive approaches to treating corneal disease.2,3 However, despite the significant technological and surgical advancements that have dramatically improved the clinical outcomes of corneal transplantation, there continues to be a significant shortage of available corneal tissue. Currently, only 1 in 70 patients who may benefit from the procedure eventually receive it.4
 |
|
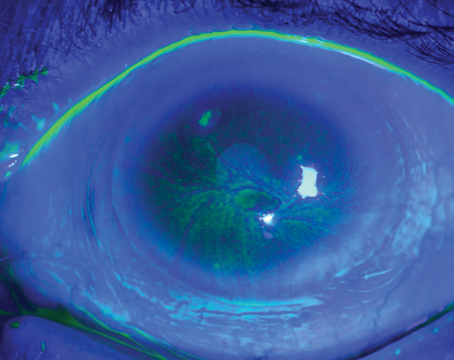
Figure 1. A) Rabbit model of acid burn injury. B) One-month postop following mi-KPro implantation. C) One-year postop following mi-KPro implantation. Intraocular pressure, retina and optic nerve were normal at one year. Irido-corneal angle was open with no retroprosthetic membrane and clear optic. Photo credit: Eleftherios Paschalis, MD. |
Artificial corneas, or keratoprostheses, have been proposed as a potential answer to the limitations of traditional donor keratoplasty. Fully synthetic corneas can be made readily available and be used to augment the supply of transplantable tissue by circumventing the need for costly eye banking infrastructure. However, artificial corneas have historically been used primarily as a last-resort option for patients who’ve experienced multiple graft failures or aren’t suitable candidates for traditional donor keratoplasty, likely due to the frequent postoperative complications that may lead to loss of vision or loss of the eye.
Keratoprostheses that have been cleared by the United States Food and Drug Administration include the Boston type-1 keratoprosthesis (1992) (Massachusetts Eye and Ear Infirmary, Boston), the most widely implanted device globally with subsequent modifications including the click-on and Lucia models also gaining approval; the Boston type-2 keratoprosthesis (1992), and the AlphaCor (2003) (formerly Coopervision Surgical, Lake Forest, California) which was the first approved fully synthetic keratoprostheses. Recently, reinvigorated efforts in developing fully synthetic flexible devices have resulted in several prototypes now undergoing clinical trials. Here, we’ll summarize these new developments.
Boston mi-KPro
The Boston type-1 keratoprosthesis is the most extensively studied device; frequently referenced as the standard of care for artificial corneal transplantation. Newer models of the device including the click-on and Lucia models that consist of a two-piece design have likewise gained FDA approval and improved the accessibility issues outside of United States. However, long-term studies reporting increasing rates of complications including retroprosthetic membrane formation, sterile keratolysis and, most significantly, glaucoma, have limited the application of these devices.5,6
The minimally invasive keratoprosthesis (Boston mi-KPro) was developed in an attempt to overcome these postoperative complications by decreasing the inflammation, post-implantation.7 The device uses a new ultra-thin, flexible titanium backplate that’s implanted anterior to Descemet’s membrane similar to deep anterior lamellar keratoplasty.7 There remains limited biointegration with the host cornea due to the titanium material. Only the optic penetrates the anterior chamber, resulting in less trauma compared to the Boston type-1 keratoprosthesis. The flexibility of the new backplate addresses the rigidity issue of the Boston type-1 keratoprosthesis, which caused a significant inflammatory response due to micro-trauma from blinking.
A poster presentation detailing an animal study compared the mi-KPro to traditional penetrating keratoplasty in alkali and acid burn models, reporting minimal complications in the mi-KPro eyes after 12 months. No mi-KPro eyes developed ocular hypertension or had significant optic nerve axonal loss, while half of the eyes receiving traditional keratoplasty showed significant optic nerve axonal loss.
CorNeat
 |
|
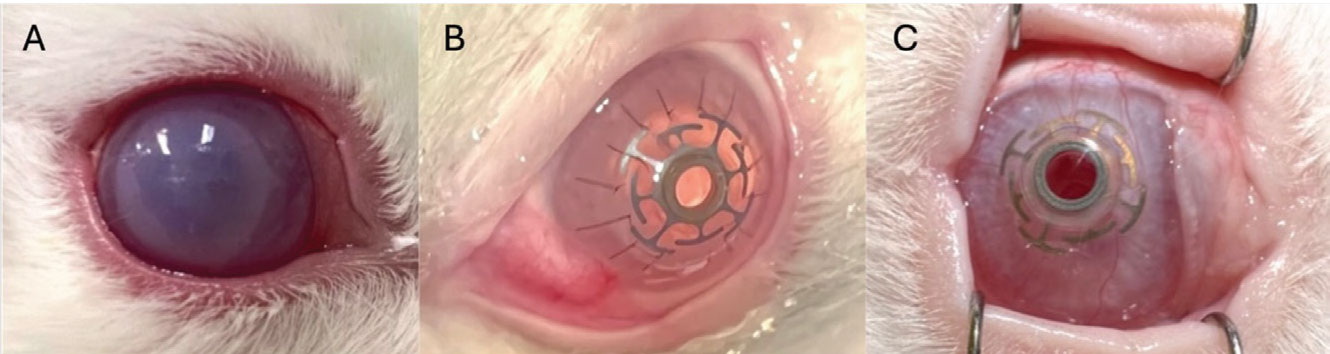
Figure 2. Slit-lamp picture showing postoperative month 12 following CorNeat implantation. Photo credit: Allan Slomovic, MD. |
CorNeat keratoprosthesis (CorNeat Vision, Israel) features a unique design that consists of a central full-thickness optic made out of polymethylmethacrylate integrated with a polyurethane fiber skirt, representing a combination of traditional rigid keratoprostheses and novel flexible devices. The skirt is designed to integrate directly with the host conjunctiva rather than the optic with the host cornea, a novel approach that aims to enhance the bio-integration by taking advantage of the highly vascular conjunctival bed to ideally minimize the risk of device extrusion. The polymethylmethacrylate is a proven material with excellent optics.
The surgical technique involves placement of the device skirt under the host conjunctiva with insertion of the optic into a central corneal trephination site. Although the biointegrating skirt is a novel way to improve the device retention, rigidity and lack of bioadhesion around the optic may pose known challenges that traditional keratoprosthesis devices have been associated with. This device is indicated for patients with a history of previous graft failure.
The first published in-human implantation in 2023 marked a milestone for the company.8 One-year outcomes of the device in the first human implantation showed visual acuity improvement. The device remained in position with some regional conjunctival retraction over the skirt, and no anterior chamber inflammation was observed. Short-term rabbit studies reported a retention rate of over 80 at six months, with minimal anterior chamber inflammation. However, cataract developed in five of the eight eyes, as expected with any full-thickness device.9 The ongoing multicenter clinical trial in Canada, France, Israel and the Netherlands will provide critical data on the device’s longer-term performance in diverse populations and clinical settings.
 |
|
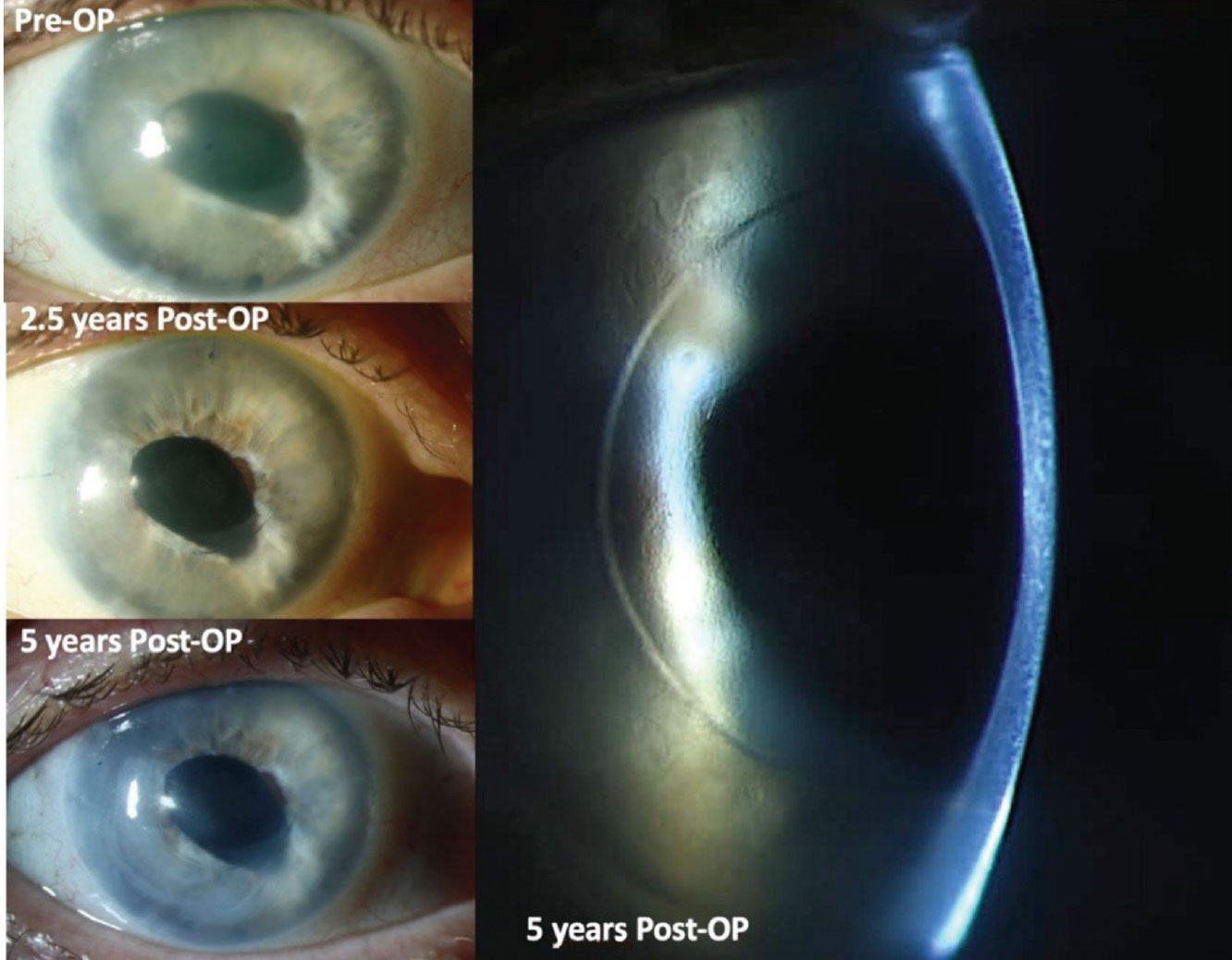
Figure 3. A 58-year-old female status post cataract surgery complicated by endophthalmitis sustained corneal endothelial decompensation, despite aggressive management. She underwent a conventional DMEK which failed and led to end-stage bullous keratopathy. EndoArt device was implanted in 2019 which kept the cornea clear over the five years of follow-up. Photo credit: Gerd U. Auffarth, MD. |
EndoArt
The EndoArt (EyeYon Medical, Israel) introduces a 50-µm thick, flexible, synthetic partial-thickness disc with a diameter of 6 to 8 mm designed to function as an artificial corneal endothelium.10 The device is made from a hydrophilic acrylic material and serves as a barrier preventing excessive hydration of the posterior stroma in cases of endothelial failure. The implantation technique is similar to that of donor corneal endothelial keratoplasty. After the Descemet’s membrane and endothelium are removed from the host cornea, the EndoArt is injected, and an air bubble is used to facilitate adherence to the posterior stroma. The device is currently indicated for patients with multiple endothelial graft failures or as a bridge therapy until donor endothelial keratoplasty is available.
The first human implantations, with a follow-up up to 17 months, have shown promising results, with sustained reductions in corneal thickness and improved visual acuity.10–12 The common complication of device dehiscence requiring re-bubbling may be a concern, but the lack of sterile keratolysis or encapsulation reported thus far is encouraging. A clinical trial is currently being planned in the United States.
GORE Synthetic Cornea Device
 |
|
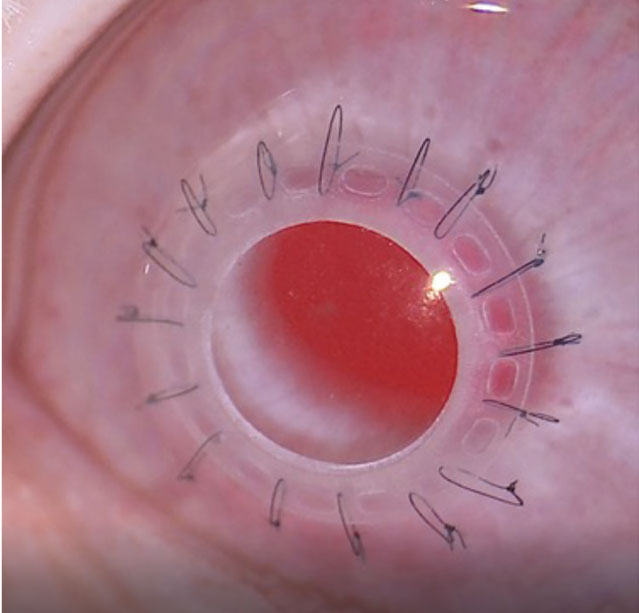
Figure 4. Gore synthetic cornea device implanted in a healthy rabbit eye. Photograph was taken 12 months following the surgery. Photo credit: Esen Karamursel Akpek, MD. |
Developed jointly by W. L. Gore & Associates and Johns Hopkins University, the GORE synthetic cornea is a flexible, full-thickness, single-piece keratoprosthesis device that aims to mimic the biomechanics of the human cornea closely.13 The device consists of a central optic and a peripheral skirt made from perfluoroalkoxy alkane (PFA), with expanded polytetrafluoroethylene (ePTFE) lining the skirt and optic wall to enhance bio-integration into the recipient corneal stroma.
The implantation process involves placing the device’s optic into a central corneal trephination and inserting the skirt into a circumferential stromal pocket.14 The surgical technique along with the biomechanical design considerations aim to minimize the effect of shear forces at the optic-device junction, reducing inflammation and enhancing the stability of the device. Spoilation studies have shown that the GORE device doesn’t experience the same issues with spoilation and debris deposition on the optic that may compromise visual acuity as previous flexible keratoprostheses.13 These results highlight the device’s potential for long-term compatibility with commonly used topical eye medications.
Medium-term rabbit studies have shown no signs of intraocular inflammation, periprosthetic membrane formation, cataracts or glaucoma.14,15 The evidence of bio-integration, including collagen deposition and fibroblast ingrowth into the skirt and optic wall, as early as six weeks post-implantation, is particularly promising. Currently, an early feasibility human study assessing the safety and efficacy of the device is being initiated in Mexico.
In conclusion, recent advances in the field of artificial corneal transplantation hold significant promise for patients who are poor candidates for traditional donor keratoplasty or reside in areas of the world with a scarcity of donor corneal tissue or eye banking. Newer devices seem less-invasive surgically and are showing fewer complications and better outcomes compared to earlier models. Notably, studies on newer flexible devices report significantly lower rates of glaucoma than the rigid Boston keratoprosthesis, although these findings are based on significantly shorter-term follow-ups.
Minimally invasive and/or partial-thickness devices such as the EndoArt and Gore synthetic cornea device offer an option for patients with repeated endothelial graft failure or an alternative for treating endothelial disease in areas where the donor supply isn’t adequate to address patient needs. These innovations signify a shift towards more tailored approaches in corneal prosthetics. However, the challenge remains to develop a cost-effective device that can be widely adopted, particularly in resource-limited settings devoid of eye banking, where artificial corneas could provide substantial benefits.
Further research and extensive clinical studies are essential to optimize these devices, improve their outcomes and broaden their applicability. The ultimate goal is to enhance access to sight-saving treatments for patients with corneal blindness around the world, ensuring that advancements in biotechnology translate into real-world benefits for those in need.
Mr. Li is a medical student at the Icahn School of Medicine at Mount Sinai in New York City, and a research assistant with the Ocular Surface Disease and Dry Eye Clinic at the Wilmer Eye Institute at Johns Hopkins University.
Dr. Akpek is the Bendann Family Professor of Ophthalmology and director of the Ocular Surface Disease and Dry Eye Clinic at the Wilmer Eye Institute.
Address correspondence to:
Esen Karamursel Akpek, MD, The Bendann Family Professor, The Ocular Surface Disease Clinic, The Wilmer Eye Institute, Johns Hopkins University School of Medicine, 1800 Orleans Street, Woods 372, Baltimore, MD 21287-9238.
Phone: (410) 955 5214
Fax: (410) 614 9172
esakpek@jhmi.edu
Financial disclosures: Dr. Akpek serves as a consultant to W.L. Gore & Associates, maker of the Gore synthetic cornea device. Mr. Li doesn’t have a financial interest in any products mentioned.
1. Zirm E. Eine erfolgreiche totale Keratoplastik. Graefes Arhiv für Ophthalmologie 1906;64:3:580-593.
2. Ghosheh FR, Cremona F, Ayres BD, et al. Indications for penetrating keratoplasty and associated procedures, 2001-2005. Eye Contact Lens 2008;34:4:211-214.
3. Lois N, Kowal VO, Cohen EJ, et al. Indications for penetrating keratoplasty and associated procedures, 1989-1995. Cornea 1997;16:6:623-629.
4. Gain P, Jullienne R, He Z, et al. Global survey of corneal transplantation and eye banking. JAMA Ophthalmol 2016;134:2:167-173.
5. Dohlman C. The Boston keratoprosthesis-The first 50 years: Some reminiscences. Annu Rev Vis Sci 2022;8:1-32.
6. Greiner MA, Li JY, Mannis MJ. Longer-term vision outcomes and complications with the Boston type 1 keratoprosthesis at the University of California, Davis. Ophthalmology 2011;118:8:1543-1550.
7. Sharma J, Dohlman TH, Zhou C, et al. Minimally invasive keratoprosthesis (mi-KPro) for vision restoration after severe chemical injury. Investigative Ophthalmology & Visual Science 2023;64:8:5136.
8. Bahar I, Reitblat O, Livny E, Litvin G. The first-in-human implantation of the CorNeat keratoprosthesis. Eye (Lond) 2023;37:7:1331-1335.
9. Litvin G, Klein I, Litvin Y, Klaiman G, Nyska A. CorNeat KPro: Ocular implantation study in rabbits. Cornea 2021;40:9:1165-1174.
10. Auffarth GU, Son HS, Koch M, et al. Implantation of an artificial endothelial layer for treatment of chronic corneal edema. Cornea 2021;40:12:1633-1638.
11. Fontana L, di Geronimo N, Cennamo M, Mencucci R, Versura P, Moramarco A. Early outcomes of an artificial endothelial replacement membrane implantation after failed repeat endothelial keratoplasty. Cornea. November 22, 2023. Online ahead of print. doi:10.1097/ICO.0000000000003433
12. Abusayf MM, Tan GS, Mehta JS. Pull-through insertion of EndoArt for complex eyes. Am J Ophthalmol Case Rep 2023;32:101878.
13. Li G, Aldave AJ, Amescua G, et al. Design and biocompatibility of a novel, flexible artificial cornea. Transl Vis Sci Technol 2024;13:5:19.
14. Akpek EK, Aldave AJ, Amescua G, et al. Twelve-month clinical and histopathological performance of a novel synthetic cornea device in rabbit Model. Transl Vis Sci Technol 2023;12:8:9.
15. Akpek EK, Van Court S, Glass S, Schmiedel T, Troutman M. Short-term clinical outcomes of a novel corneal prosthetic device in a rabbit model. Cornea 2020;39:6:706-712.