In the United States, there are approximately 18,000 ophthalmologists, of whom 9,000 perform cataract surgery regularly. Thus, a typical surgeon might anticipate a surgical volume of about 400 eyes per year. National statistics in other specialties, such as cardiovascular surgery and orthopedics, suggest that a surgeon who performs more than 50 procedures per year generates a significantly lower complication rate; for an institution, the threshold number is 200. America’s cataract surgeons and the institutions where they work almost universally reach these numbers, which is encouraging for the potential patient. Still, the cataract operation of today is far from perfect, and because vision is so important to quality of life, everyone engaged in this marvelous sight-restoring procedure is highly motivated to seek continuous improvement in outcomes. Here, I will share some thoughts on what I am doing in 2015 to enhance my patient outcomes.
Preoperative Issues
In the preoperative examination, I do more testing and objective screening, usually at my own expense, since most third-party payers will not pay for these tests. Approximately 25 percent of my patients opt for a so-called premium option, which includes a desired refractive outcome to reduce their dependence on glasses. I call this refractive cataract surgery, and I discuss this option with all patients. In order to properly determine who is a good candidate for refractive cataract surgery, I find screening for hyperosmolarity and dry eye with the TearLab device, irregular astigmatism, astigmatism axis and ectasia with corneal topography, and subtle macular changes with optical coherence tomography all to be indispensable. These tests are therefore a routine part of my current exam.
As a corneal surgeon who also treats a lot of glaucoma, my preop testing may also frequently include pachymetry, goniscopy, specular microscopy, visual fields and OCT of the optic nerve. In summary, I am doing a lot more testing, and in the Accountable Care Act era with the triple aim of excellent outcomes, highly satisfied patients and reduced cost, the extra cost is usually borne by me. The 25 percent of patients who opt for refractive cataract surgery helps cover these costs, as does the fact that my partners at Minnesota Eye Consultants and I perform most of our surgery in an owned ambulatory surgery center. As I have suggested in several editorials in Ocular Surgery News, the triple aims of the accountable care act will in large part be achieved on the backs of the physician provider. Such is the state of modern-day U.S. practice.
In those patients with evidence of significant ocular surface disease, I perform what I call ocular surface preparation. Most patients do not want to wait more than two weeks to schedule their surgery. For me, the most rapidly acting agent for ocular surface preparation is a topical corticosteroid. I usually combine it with an antibiotic using one of the combinations drops such as tobramycin/dexamethasone or tobramycin/loteprednol 4X daily, along with artificial tears (usually Systane Balance or Blink), hot packs (Bruder Compresses are convenient and effective), lid hygiene(I Lid Cleanser from NovaBay and, in recalcitrant cases, Cliradex) and 2 grams a day of a quality omega 3 (PRN or Nordic Natural). I want corneal staining absent before surgery whenever possible. I am increasingly aware of and aggressive in the preoperative management of ocular surface disease. I also pretreat with an NSAID for three to seven days, with duration depending in large part on a given patient’s risk for postoperative inflammation and cystoid macular edema. If I am using a topical corticosteroid, I prescribe it before surgery for use the same number of days. The NSAID and corticosteroid are synergistic, and no additional cost is generated.
Intraoperative
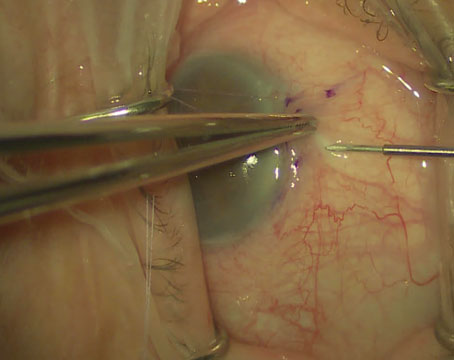
In 2013-2014, I worked to incorporate femtosecond laser-assisted cataract surgery (FLACS) into my practice, but in 2015 it will play a minimal role. I like FLACS and find it fun to do, but simply cannot afford it in my current practice environment. I am passionate about the ocular surface, and also advocate for protecting it during surgery. I therefore treat the corneal epithelium with the same respect most surgeons reserve for the corneal endothelium. I find a dispersive viscoelastic on the ocular surface, especially when warmed in an incubator to 34 to 37 degrees C, to be extremely effective in protecting the ocular surface during surgery. In addition, the surgeon view is enhanced and no irrigating with BSS is required during the procedure, freeing the scrub nurse for other tasks.
 |
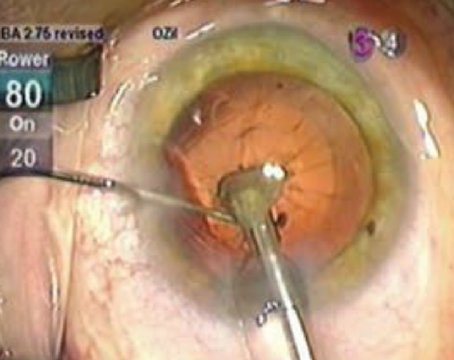
I have found intraoperative aberrometry enhances my refractive outcomes (Verifye, WaveTec). The average patient in America who presents for cataract surgery is 69 years of age with only a mild/moderate density of nucleus. For this reason, I have adopted a supracapsular phacoemulsification approach I call tilt and tumble for most cases. I hydrodissect the nucleus with the Chang cannula until it sits vertical within the capsular bag. In some cases, viscodissection with my dispersive viscoelastic is helpful. This approach also works extremely well in patients with small pupils, intraoperative floppy iris syndrome, or IFIS, and pseudoexfoliation cases, which are very common in my practice. I will also “push” the iris back in IFIS cases with Viscoat. In this approach, the nucleus itself dilates the pupil and irrigation is superior to the iris plane, blowing the floppy iris posterior rather than anterior. The use of the soft-shell approach, as described by Steve Arshinoff, MD, with a dispersive viscoelastic (the same Viscoat I have used to protect the corneal epithelium, viscodissect and position the iris in IFIS) and a bevel-down, 20-ga. phaco needle with a hyper-pulse energy profile generates minimal endothelial cell loss. I have also adopted forced-infusion fluidics with the Stellaris and Centurion, setting the intraocular pressure at 55 to 60 mmHg, generating an extremely stable anterior chamber. When needed, the ocular sealant ReSure has replaced sutures. Perhaps most controversial, after three years of intracameral moxifloxacin, I have adopted the intavitreal transzonular injection of moxifloxacin or moxifloxacin/vancomycin and triamcinolone (TriMoxi, Imprimis) for infection prophylaxis and inflammation management.
Postop
My preferred postoperative regimen requires only a single drop when TriMoxi is injected—ILevro or Prolensa once per day at bedtime. I like my patients to be on an NSAID for four to six weeks in routine cases and eight to 12 weeks in high-risk cases such as those with diabetes mellitus. I also encourage patients to continue with ocular surface treatment as needed. To me, there is an ocular surface rehabilitation required after surgery followed by long-term ocular surface maintenance. At a minimum, I encourage the same artificial tears prescribed preoperatively 4X daily, along with other adjuncts as needed. For many patients, ocular surface disease is first diagnosed in a preoperative examination and lifelong therapy is appropriate and to be encouraged, including adjuncts such as omega 3 nutritional supplements, Restasis, erythromycin ointment or topical azithromycin and low-dose oral doxyclycline (20 to 40 mg a day), when needed.
In refractive surgery patients, I am aggressive with enhancements, which for me are usually LASIK or PRK. I will rotate a toric intraocular lens in select cases, using the astigmatismfix.com guidelines of my partner David Hardten, MD and former fellow John Berdahl, MD, but I find laser corneal refractive surgery to be more accurate for most patients, as I can fine-tune both the sphere and cylinder. I am very reluctant to exchange multifocal or accommodating IOLs, and stall as long as I can and exhaust all other possibilities—especially ocular surface restoration, posterior capsule clarity and residual refractive error management—before performing IOL exchange. Having implanted these lenses for more than 20 years, I find an in-focus, well-centered multifocal or accommodating IOL in a healthy eye is almost always accepted over time by the patient. Exceptions are patients who likely should have never received a presbyopia-correcting IOL, such as those with prior radial keratotomy, significant higher-order aberrations after LASIK or even frank keratoconus, Fuch’s dystrophy, glaucoma with significant damage and macular disease, especially unrecognized epi-retinal membranes and age-related macular degeneration.
Cataract surgery fortunately continues to evolve. This field of surgery is economically viable and critical to the ophthalmic surgeon, patient and society, which supports continuing innovation. Even after 40 years, it is extremely satisfying to restore and, in many cases, enhance the vision of a patient handicapped by cataract. REVIEW
Dr. Lindstrom is the founder and attending surgeon at Minnesota Eye Consultants; he is an Adjunct Professor Emeritus at the University of Minnesota, Department of Ophthalmology and a visiting professor at the University of California, Irvine, Gavin Herbert Eye Institute.