An Elusive, Growing Problem
Skin cancer is the most common form of cancer, with an incidence that is doubling every 15 to 20 years.1 Also, between 5 and 10 percent of all skin tumors occur on the eyelids,2 meaning many of these patients may see their ophthalmologist first when they notice an ocular growth. However, as some epidemiological studies have found, diagnosing carcinoma can be a challenge.
A retrospective study from Philadelphia's Wills Eye Hospital looked at 60 patients with sebaceous carcinoma of the eyelid and adjacent structures. Initial diagnoses elsewhere were sebaceous carcinoma (32 percent), blepharoconjunctivitis (25 percent), chalazion (20 percent), basal cell carcinoma (13 percent) and squamous cell carcinoma (10 percent).3 Even after histology was taken, however, only half were correctly identified as sebaceous carcinoma; 18 percent were diagnosed as squamous cell carcinoma; 8 percent as basal cell carcinoma and 24 percent as another diagnosis or a diagnosis that wasn't available to the researchers.
In a retrospective study from Australia, surgeons studied eight patients with sebaceous gland carcinoma of the lid. Initial clinical diagnoses included blepharitis (three cases), blepharoconjunctivitis (one case), cicatrizing conjunctivitis (one case) and lid lesions (two cases).4 What's more, even after a biopsy was taken, seven of the eight tumors were misdiagnosed as Bowen's disease. Six of these cases showed no invasive disease on the initial biopsy but eventually proved to be invasive sebaceous carcinoma on subsequent excisions. In most of the cases, the upper lid was involved. The delay in diagnosis ranged from zero to 56 months.
Unfortunately, even tumors that respond well to treatment can call for complex reconstruction when they occur in such an intricately formed area as the lid, making prompt diagnosis even more critical. A retrospective study from Spain analyzed 24 cases of basal cell carcinoma located in the nasolabial fold and compared them to patients with basal cell carcinoma that occurred on the cheek or forehead. When compared to similar tumors on the forehead or cheek, the researchers found that basal cell carcinoma on the nasolabial fold presented with shorter evolution times from its first symptom, had a smaller size, had been less aggressively treated before and showed a mostly non-aggressive histological subtype. However, the nasolabial tumors required more stages of surgery and the remaining tissue required more complex reconstruction after the tumors were removed.5
Basal cell carcinoma with destruction of the lid-margin architecture. Basal cell carcinoma represents approximately 90 percent of all periocular tumors.

Ari Nemet, MD
Following is a review of the top three tumors that occur in the periocular region in terms of incidence.
Basal Cell Carcinoma
Basal cell carcinomas represent a little over 90 percent of malignant lid lesions, with around 70 percent of them appearing in the lower lid.6 Risk factors for these particular tumors include fair skin and a greater degree of sun exposure. Outdoor workers and those living in southern latitudes that have higher degrees of ambient UVB radiation are at higher risk, and there's a significantly higher incidence of basal cell in men than women.7
These tumors may also occur in scars caused by X-rays, vaccination or trauma. An elderly patient who has undergone treatment with arsenic in the past is at risk for developing basal cell carcinoma as well, even after a period of many years.8
Basal cell carcinoma will present as one of four types:9
• Nodular. This is the most common, appearing as a translucent, waxy papule with a rolled, pearly border, telangiectasia and often central ulceration.
• Morpheaform/sclerosing. These tumors resemble scar tissue or morphea, occurring as a thick, firm plaque with atrophy, hypopigmentation, erythema and prominent telangiectasia. Morpheaform basal cell carcinomas have an irregular growth pattern, making the tumors' margins difficult to delineate.
• Superficial spreading form. These occur as irregularly shaped erythematous scaling plaques with telangiectasia and a thready, well-defined border. Superficial spreading tumors are more common in the trunk than the ocular area, however.
• Pigmented. Pigmentation can occur in any of the other types.
In the common nodular form, as the margin of the tumor grows, the center's blood supply diminishes, and begins to take on a crusted, umbilicated appearance, which may loosen and bleed.6 Clinicians note that this bleeding is often what brings the patient to the physician.
"The borders of the lesion are usually curly, especially in basal cell carcinoma," says Ari Nemet, MD, oculoplastics specialist and instructor at the Goldschleger Eye Research Institute, Sackler Faculty of Medicine, Tel-Aviv University. "Another important sign is loss of lid margin architecture with the destruction of normal anatomic features."
This patient neglected his basal cell carcinoma and faces complex surgery.

Karen Chapman, MD
Dr. Nemet says that when differentiating basal cell carcinoma from squamous cell carcinoma, an important sign is hyperkeratosis. "This isn't common with basal cell, but instead is more common with squamous cell carcinoma. Also, actinic skin damage is common to both basal cell and squamous cell, but, the lighter a patient's skin is, especially in someone with blue eyes, the more appropriate it is to think about squamous cell."
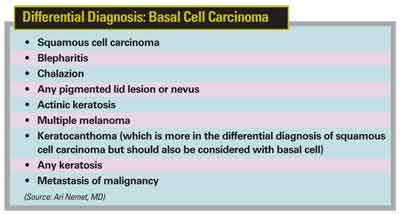
(For the conditions that can resemble basal cell carcinoma, see the boxed text on this page.)
Oculoplastics specialist Karen Chapman, MD, of Sarasota, Fla., says that basal cell carcinoma can also be confused with benign sudoriferous cysts on the lid, but you can differentiate them in the clinic. "Sudoriferous cysts have a thin outer coating, and are very smooth," she says. "They also usually transilluminate."
If you suspect basal cell carcinoma, experts recommend an immediate biopsy for confirmation. Dr. Chapman says you can often do the biopsy yourself. "There's no reason an ophthalmologist can't perform the biopsy to get the ball rolling," she says. "You use an 11 or a 15 blade to do a shave, or use small tenotomy scissors, the instruments you'd usually use for a chalazion." Basal cell carcinoma in the medial canthus poses a high risk of recurrence.

Ari Nemet, MD
Squamous Cell Carcinoma
In terms of frequency, squamous cell carcinoma accounts for roughly 5 to 9 percent of periocular tumors.6
Causal factors and salient points in the patient history include radiation exposure of various kinds: Squamous cell tumors may be linked to skin damage from long-term exposure to UV light, as well as X-ray and infrared exposure.8 They may also arise from pre-existing lesions such as those from Bowen's disease, burns or chronic inflammation.6 Other carcinogens associated with squamous cell carcinoma include pitch, tar, mineral oils and inorganic arsenic.8 DNA alteration may also play a role in the case of certain rare genetic disorders, such as xeroderma pigmentosum, which leads to defective DNA repair; and the DNA of the human papilloma virus, which can be integrated into the DNA of keratinocytes and cause a malignancy to develop.8
Diagnosing squamous cell carcinoma can be a challenge because it varies in presentation, without a constant distinguishing feature.6 Often, however, these tumors will present as painless nodular or plaque-like lesions with irregular, rolled edges, chronic scaling, fissuring of the skin, pearly borders, telangiectasias and early central alteration.6
As with basal cell carcinoma, recurring problems are always a red flag. "One of the things to watch for is an atypical course of a growth that doesn't go away after an intervention," says Dr. Chapman. "Another sign to watch for is madarosis, as long as a mental disorder such as trichotillomania can be ruled out."
Dr. Nemet says if he sees hyperkeratosis, actinic keratosis lesions and scaly skin, he begins to think squamous cell. "Squamous cell carcinoma is much more aggressive than basal cell," he says. "The margin may be much more diffuse with subclinical tumor involvement."
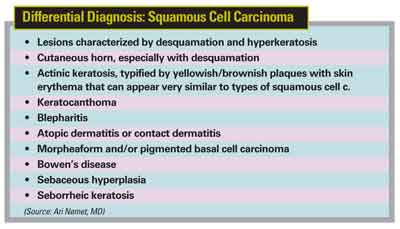
(For the most common differential diagnoses for squamous cell carcinoma, see the boxed text below.)
Dr. Nemet says keratocanthoma is a clinical entity that can look very similar to squamous cell carcinoma, and that some clinicians refer to it as "low-grade squamous cell carcinoma." Keratocanthomas appear suddenly and then grow quickly, reach a size of 0.5 cm to 2 cm, then regress over a period of weeks to months. They appear as smooth, crimson to flesh colored, dome-shaped papules with a central crater filled with a keratinous plug.7
A biopsy would be mandatory to differentiate squamous cell from other lesions, and it may be worth checking the rest of the face, neck, scalp and dorsum for other tumors, as squamous cell patients frequently have additional tumors in regions vulnerable to actinic radiation damage.6
Sebaceous Gland Carcinoma
This is an aggressive tumor that, fortunately, is rarer than basal cell or squamous cell carcinoma, accounting for between 1 and 5 percent of lid tumors,10 though it is more common on the lids than elsewhere on the body.11 It afflicts women more frequently than men, is usually diagnosed in patients in their 60s and 70s, and typically occurs in the upper lid.6
Dr. Nemet says it's worth considering the diagnosis of sebaceous gland carcinoma when a patient presents with unilateral blepharoconjunctivitis or recurrent chalazion, classic "masqueraders." "Even the first recurrence should elevate the possibility of sebaceous carcinoma in the region," he says. "Especially in cases in which the eyelid is very swollen or inflamed, the growth should be biopsied to rule out carcinoma."
This tumor is commonly mistaken for chalazion, since it starts deep within the lid and just appears initially as a diffuse swelling with a firm or rock-hard texture. Patient history and presenting signs can be helpful in differentiating the two growths: it's unusual for chalazion to appear later in life without a history of it; the usual chalazion texture is more rubbery and less diffuse; and chalazion usually spares the eyelashes.6
Squamous cell carcinoma has been linked to long-term exposure to UV light and other forms of radiation.

Ari Nemet, MD
"The presentation of any yellowish material in a malignant-appearing lesion suggests sebaceous gland carcinoma," Dr. Nemet adds. "Also, if there is any multicentric spread for a lesion, in the same or even the opposite lid, you should suspect sebaceous cell."
Other diagnostic clues that help distinguish sebaceous gland carcinoma from basal cell and squamous cell carcinoma include the following:6
• Until the sebaceous carcinoma erupts out of the tarsus, the skin is, for the most part, movable over the lesion, while both basal cell and squamous cell tumors move with the skin;
• As a meibomian carcinoma grows toward the surface, the layers of the lid fuse into one mass;
• Basal cell and squamous cell carcinomas originate more superficially, frequently with ulcerations, surface irregularities and hyperkeratosis, while a meibomian gland carcinoma will often simply have smooth, taut lid skin covering it.
"If a patient's biopsy comes back positive for sebaceous cell carcinoma, I'd recommend the general ophthalmologist not try to excise it himself," says Dr. Chapman. "It's a very aggressive lid cancer that poses a risk of 'skipping'—or spreading—and there might be a lot more tissue involvement than what is evident to the untrained eye." Squamous cell carcinoma's appearance can vary from case to case, but fissuring of the skin is one of the possible signs.

Ari Nemet, MD
Diagnostic Pearls
In addition to the specific differential diagnosis considerations for the individual tumors, Drs. Nemet and Chapman list some general signs to help weed out the malignant from the benign:
• Alteration is typical for malignant lesions over time, whereas benign growths often look similar from visit to visit;
• Malignant lesions usually aren't painful when touched since they're not inflammatory, though they may be red;
• In general, malignancies tend to be firm to the touch;
• An irregular border and asymmetric shape are typical signs of a malignant growth, while it's not uncommon for benign lesions to be quite symmetrical;
• Malignancies frequently cause distortion or irregularity of the lid margin or disrupt the gray line that separates the anterior from the posterior part of the lid;
• Watch for sun damage on the patient's face, as that can be a clue to a patient at risk for skin cancer.
Paying attention to these signs, along with a familiarity with the typical appearance of the various tumors, will serve you well as you examine suspicious lesions.
1. Pons M, Quintanilla M. Molecular biology of malignant melanoma and other cutaneous tumors. Clin Trans Oncol 2006;8:7:466-474.
2. Rossi R, Puccioni M, Mavilia L, Campolmi P, Mori M, et al. Squamous cell carcinoma of the eyelid treated with photodynamic therapy. J Chemother 2004;16:3:306-309.
3. Shields JA, Demirci H, Marr BP, Eagle RC Jr, Shields CL. Sebaceous carcinoma of the eyelids: Personal experience with 60 cases. Ophthalmology 2004;111:12:2151-2157.
4. Leibovitch I, Selva D, Huilgol S, et al. Intraepithelial sebaceous carcinoma of the eyelid misdiagnosed as Bowen's disease. J Cutan Pathol 2006;33:4:303-308.
5. Garcia L, Nagore E, Llombart B, et al. Basal cell carcinoma of the nasolabial fold: An apparently 'benign' tumour that often needs complex surgery. J Eur Acad Dermatol Venereol 2006;20:8:926-930.
6. Beyer-Machule CK, Riedel KG. Basal cell carcinoma. In: Albert DM, Jakobiec FA, eds. Principles and Practice of Ophthalmology, Clinical Practice, vol 3. Philadelphia: W.B. Saunders Co., 1984:1724-1732.
7. Habif TP. Clinical Dermatology: A Colour Guide to Diagnosis and Therapy, 3rd ed. St. Louis: Mosby, 1996:649-664.
8. Hunter J, Savin J, Dahl M. Clinical Dermatology, 3rd ed. Malden, Mass: Blackwell Science, 2002:265-274.
9. Goldstein BG, Goldstein AO. Practical Dermatology. St. Louis: Mosby, 1992:136-142.
10. Vaughn GJ, Dortzbach RK. Eyelid malignancies. In: Yanoff M, Duker JS, eds. Ophthalmology. London: Mosby, 1999.7-12.4
11. Rao NA, Hidayat AA, McLean IW, Zimmerman LE. Sebaceous carcinomas of the ocular adnexa: A clinicopathologic study of 104 cases, with five-year follow-up data. Hum Pathol 1982;13:2:113-22.



