When health-care practices that provide care under Medicare and Medicaid were first mandated to adopt electronic health records years ago, many would admit it was a headache going from paper to digital. Looking in the rearview mirror, they’d also tell you the experience was worth it for the efficiencies it created across all departments of a practice.
However, those initial efficiencies may be losing their luster after so many years, leading physicians to explore new platforms and features. Embarking on another transition can be a daunting task for practices, and it’s not uncommon for them to push this off to avoid the inevitable monopolization of time and energy, not to mention cost. “Many practices choose to stick with their current systems because the process of switching can seem overwhelming and problematic,” says Barbra Dey, OD, COE, the CEO of Seattle-based Dey Ophthalmic Consulting, and a member of the American Society of Ophthalmic Administrators’ Mentorship Committee. “Effective switching requires meticulous organization and careful planning.”
“I’d put us in that category,” says Guido Piquet, MBA, COE, the COO at Mann Eye Institute in Houston. “We probably held on to our previous product longer than we should have for that very reason, knowing it was going to be a painful transition. However, we eventually reached a point where the pain of staying with the old system outweighed the pain of making the switch because we didn’t feel like we were moving forward.”
According to the doctors, practice administrators and consultants we spoke with, there are some unavoidable challenges in the process of switching EHR systems, but they pale in comparison to the long-term benefits. Read on to find out about their experiences, lessons learned and top pearls for making a successful transition.
Considerations for Switching
Whatever the cause, EHR migration can be a labor intensive commitment that’s not undertaken lightly.
“There’s usually significant factors that make a practice want to switch,” says Julia Lee, JD, principal consultant for NorthStar Vision Partners, located in the Philadelphia region, and chair of the American Academy of Ophthalmic Executives. “Probably the most common is if their current platform is just not keeping up with new development, or isn’t yet providing the support required, or even just sunsetting.”
The ophthalmology specialty has seen considerable consolidation in the EHR market, according to Michael V. Boland, MD, PhD, assistant chief medical information officer at Mass Eye and Ear and associate professor at Harvard Medical School. “Despite this consolidation, many vendors remain, including smaller ones that may struggle to adapt to changes in regulations, clinical practices, and user preferences,” he says. “It’s understandable that some practices, initially incentivized to adopt EHRs in the mid-2010s, have since decided to transition away from those systems.”
Another scenario is more along the lines of want vs. need, especially when it comes to integration.
“Most of the reasons for inefficiencies within the system stem from poor integration between different software systems,” says Ms. Dey. “In ophthalmology, practices typically use a practice management system to handle billing, patient outreach, scheduling and other tasks. Additionally, they use an EHR system. If the practice has an optical component, there’s yet another optical software system involved. Ideally, these systems should communicate with each other seamlessly, but in reality, they often don’t. This is where the biggest frustrations come in.”
Infrastructure is another consideration. Practices want to move from managing server-based solutions to cloud-based solutions. “I know a lot of practices that say, ‘Wow, keeping up with all of these IT infrastructure requirements is becoming increasingly burdensome and costly. We’d like to go to some type of subscription model,’ ” says Ms. Lee.
This was a top priority for Tri-Century Eye Care in Southampton, Pennsylvania. The practice had recently merged, with each entity using different EHR and practice management systems. “Part of the reason for migrating to a new system was to unify the entire practice onto a single platform,” says Zach Kushner, MBA, MSIT, COE, the CEO of Tri-Century. “We could’ve simply integrated half of the practice into the system used by the other half. However, each software had its own inherent challenges. For me, the main driver was transitioning to a cloud-based platform. I wanted to move away from the hardware cycle of replacing servers every three to five years. I wanted a system that our doctors could access from anywhere on the web without needing to VPN into our data center. ”
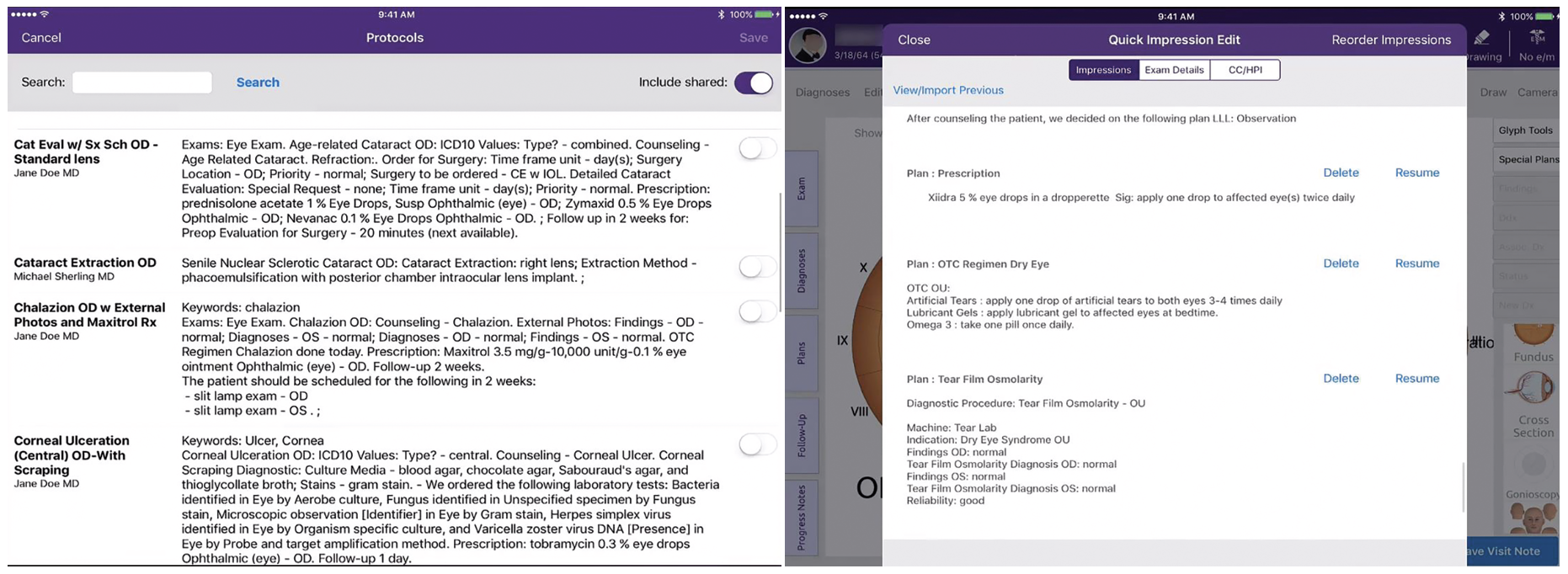 |
| In the EHR software system used by Mann Eye Institute there’s a feature called “Protocols,” which helps physicians create pre-built plans that allow them to chart an entire exam in seconds. Once these protocols are applied, the physician can then make the few changes that apply to that specific patient. |
For Mann Eye Center, it was less about one specific feature and more about finding a vendor who could be viewed as a partner. “One of the biggest reasons we decided to switch to a new product was our need for a solution we could build upon for the next 10, 15, even 20 years,” says Mr. Piquet. “We were looking for a company that was making sufficient investments in improving their product. We understood that no one product is perfect, but we wanted to partner with a vendor who was going to be here for the long run and continue to invest in their product and work with us as a partner. We didn’t really have that type of relationship with our previous platform, which is why our strategy was more about long-term potential rather than finding an immediate perfect fit.”
Despite having these concrete goals and wishes, it can take years for practices to commit to the project of switching.
“I think the biggest barriers to switching are probably time and resources, meaning the time and effort required to manage a successful transition, because no matter what resources the vendor will provide, there’s always going to be a heavy lift required of the practice,” says Ms. Lee. “You really need somebody very strong and on top of it internally who’s going to coordinate and make sure that the implementation steps are happening successfully within the practice on the ground.”
At Tri-Century, Mr. Kushner says the prospect of merging onto a single system was discussed, but not prioritized, between 2019 and 2020. “It wasn’t until 2021 that we seriously considered it,” he says. “After six months of due diligence on various platforms and facing staffing difficulties due to the pandemic, the project was put on pause. We revisited the discussion in late 2022 and early 2023. We eventually implemented the new system in August 2023. This lengthy process was due to misalignment among doctors and staffing challenges, leading to a protracted timeline.”
Most-requested Features
As practices begin the investigation phase, one of the most important—and sometimes complicated—steps is to get all departments on the same page about their expectations.
“To ensure a successful transition, a high-functioning team that includes representatives from all relevant departments should be assembled,” Ms. Dey says. “This team should develop a comprehensive plan, including must-have and nice-to-have features for the new EHR system.”
When evaluating EHR systems, practices commonly look for features that enhance efficiency and simplicity. “Questions often center on how well the system interfaces with diagnostic equipment, tracks patient time from check-in to check-out, and integrates with billing and point-of-sale systems,” says Ms. Dey.
 |
| When upgrading to a new EHR system, hardware is another important component to consider. Practices should prepare to invest in technology such as tablets, new credit card machines and reliable internet connectivity. |
Some of the most commonly asked questions when researching systems are:
- Does it automatically send out registration paperwork?
- Does it send it by text?
- Do appointment reminders go out by text, robocall and/or email?
- How many minutes is the check-in process?
- Does the system track how many minutes each step in the process takes, total time?
- Does it interface with our other diagnostic equipment? Is that built in or is it an add on?
- How much clicking does the doctor need to do?
- Are diagnoses pre-loaded with coding suggestions?
- How do we submit claims?
- How does it integrate with my POS and is the charge reflected in my PM system? and
- Can patients e-sign to reduce paper?
Provide vendors with these requirements in advance to ensure they can meet them, advises Ms. Dey. “Organize a team call where you talk through each of them and ask the vendor to tell you how it will work in the new system,” she suggests. “It’s important to have a clear understanding of the vendor’s capabilities and limitations to avoid disappointments later.”
“In the research phase, I was the primary person responsible for evaluating different options and meeting with vendors,” recalls Mr. Piquet. “I had some key criteria in mind for each vendor: efficiency; scalability; and future technological investments, including automation and artificial intelligence. It was important to see which vendors were ahead in these areas and had concrete plans for future advancements.”
In addition to wanting a cloud-based system, Mr. Kushner says they also wanted a little bit of simplicity. “It’s a tough dynamic, simplicity vs. complexity,” he says. “You want a system that’s complex enough to handle your workflows and your documentation needs, at the same time you want it simple enough where the software is working for you and you’re not working for the software.”
One concept that rose to the top of their list was “point of thought” data points, explains Mr. Kushner. “Doctors need intuitive entry points for data as they proceed through their workflow,” he says. “Our previous platform had different templates for each thing. Glaucoma had an independent template, retina had an independent template, contact lens had an independent template. If they’re in the middle of a complete exam and also doing a contact lens check, doctors have to juggle a couple different templates to document all of the pieces of that exam. On our new system, everything is on a single-scroll page, so all they’re doing is hitting their mouse wheel and moving up and down within that same page. It’s almost like a long web page, and everything is visually right there.”
Financial Considerations
System costs may not vary dramatically in the industry, but practices should be aware of how fees are structured by vendors and how the initial investment might compare to monthly fees and add-ons.
“Vendors should be clear about any future cost increases and the financial implications of system upgrades,” says Ms. Dey. “Typically, all of this information is on the cloud now, and that requires a monthly subscription fee. Those fees can change over time. Have the conversation up front with your vendor about how long that monthly fee will last, and what percentage increase you should expect over time. Also, as their product gets upgrades, would those be considered add-ons for a separate fee? What if it’s a feature you told them you wanted and they said it’s in the works? Will you be charged?”
This was a consideration of Mr. Kushner’s. “Older systems had significant upfront costs but lower ongoing maintenance costs, while newer systems operate on a subscription model with higher monthly costs but lower upfront investment,” he says.
There was also the matter of hardware, which can’t be overlooked even though systems are on the cloud. “Planning for hardware needs, including computers and internet connectivity, was also essential,” continues Mr. Kushner. “You need to evaluate and make sure that your hardware is up to snuff with the software that you’re choosing. Do you have scanners? Do you have credit-card machines? Do you have the appropriate computers around your offices? Is your internet connection strong enough and reliable enough for a web-based platform? Previously, we had our servers in house. If our internet went down, we could still function. With a web-based platform, if our internet goes down, we’re dead in the water. The resiliency of backup internet connectivity is important.”
Migrating data from the old system to the new one can also be a significant cost, says Ms. Lee. “This is one of the biggest surprises for practices going from one EHR to another,” she says. “There are varying philosophies, but typically, data migration is handled by a third-party company. This company should ideally have proficiency working with both systems, because they’re going to have to extract from the one and map it over to the other. But that cost is a pretty significant variable, depending on what data you want to migrate over and how much of it.”
The discrepancies between vendors adds to confusion. “Each EHR has its own method for storing data, and there’s no standardized way to migrate all data seamlessly,” says Dr. Boland. “When considering migrating to a new EHR system, it’s crucial to ask the current vendor how to handle data extraction. This process will likely involve costs, either for the new vendor’s services or for hiring external assistance.”
In Mann Eye Center’s case, Mr. Piquet says they incorrectly assumed they’d be able to keep their old system as a reference for about a year, once all patients had been seen on the new platform. “We were able to migrate all of the patient demographics and medical data in the form of a PDF chart note, but no discrete data,” he says. “A couple of the big things that we weren’t able to get were financial data and past appointments. However, we decided to prepare and implement an EHR archive solution, which now gives us the ability to retain all of that important financial information and past appointment data. In hindsight, I would have created a larger team to assist with the data migration component, which could have made each patient appointment a little more efficient.”
Training and Going Live
Once practices have committed to the new EHR system, training is the next step and there’s more than one way to go about it.
“Depending on the internal team’s capabilities, the decision might be to either train a few key individuals who then train the rest of the staff or to bring in trainers from the vendor,” says Ms. Dey. “If you choose to train the trainer, this person is now in charge of an EHR transition while also being responsible for their own daily job tasks. Can they give their full attention to this transition?”
There are pros and cons to both, says Mr. Kushner, and he’s had experience with both. “For our previous EHR, we did the train the trainer model and we took small groups aside at various points during the day and we also had staff come after hours, so there was a time investment on our core team outside of normal operating hours, but it also gave us the flexibility to juggle things and not have to shut down patient schedules,” he says.
For this latest EHR implementation, they chose to have the vendor train everyone. “We shut down the practice for two hours each morning over two weeks,” says Mr. Kushner. “Every doctor and every staff member attended every session, whether it pertained to them or not. Doctors learned the PM side, call center and front desk staff learned the EHR—everybody saw the same thing. I wanted them to have that broad brushstroke picture of the way the systems interact. I wanted them to understand what their peers within the practice were dealing with, so that it’s not an us vs. them type of mentality.”
Training and implementation may take longer than expected, notes Mr. Piquet. “We initially went in with a goal of going live within six months, but it became clear that it was going to take longer than anticipated,” he says. “Based on our experience, I now recommend adding three to six months to your initial estimate—this is dependent on the size and scope of an organization. As you start the investigation process, you’re going to unearth problems you didn’t know you had, and they have to be addressed. For us, the process ultimately took nine months.”
Mr. Kushner says his practice had a six-month runway, which allowed them to manage training, go-live dates, and hardware delivery and installation without extreme time pressure. “This time flexibility was a significant advantage, helping us avoid the tight deadlines that vendors often impose,” he says.
During the implementation, it’s beneficial to have a beta-test environment where departments can test the system with test patients and identify potential issues before going live, says Ms. Dey. “This allows for adjustments and ensures the system is fully integrated and functional.”
Mann Eye Center implemented a gradual ramp-up strategy for patient scheduling, according to Mr. Piquet. “We started with 50 percent of our usual patient load and increased to 75 percent over a few weeks, aiming to reach full capacity within three months,” he says.
Experts recommend having vendors on site during the initial go-live phase to address immediate issues and support staff. “When the trainers initially told us how long they’d need to stay on site, I was skeptical,” says Mr. Piquet. “But they told us to trust their recommendation, so we did. And they were right. Our users were quickly able to get up to speed. Especially when you have employees who all learn at different paces, we were able to focus on those who were struggling and give them additional support.”
Training doesn’t stop after that initial week or month, continues Mr. Piquet. “We did additional training sessions, followed by an optimization visit at the one-year mark where we brought the trainers back in to retrain people and find even more efficiencies,” he says. “At that point we started to get over the hump of the pain of the change and we started to see those efficiencies, with some providers seeing three to five additional patients a day. The staff are more efficient because of the new tools they have but it’s an investment in time and patience, and it takes resolve. It’s crucial to have people in leadership who are a voice of support and will help people see the end goal.”
On the Other Side
From Mr. Piquet’s perspective, he says it could take at least a year to realize the efficiencies that are better than what you had before. “Even with a great system, it just takes time for all of those components to flow through the practice from every level and for people to continue learning,” he says. “We’ve been on the system for two years and we finally hit a stride.”
No one goes through the process unscathed, says Ms. Lee. “I’d say the majority of practices are excited about the new functionalities they have access to on their latest and greatest system. If you’ve done your vetting and your selection process, if you’ve gone through that thoughtfully, then by the time implementation comes around, a lot of it is just frustration in terms of that last-mile differences between how your practice used to do something and what the new platform can accommodate.”
“Every administrator wants the system to be perfect before you go live, and we tried, but it’s never going to be perfect on day one,” Mr. Piquet says. “Whenever I get referral calls from other people looking to make a switch, I tell them that switching to a new EHR is less about finding the perfect software and more about finding a product you can grow with. ”
Top Pearls for Success
We asked our sources to provide their most important pieces of advice for those who are considering a new EHR platform. Here’s what they said:
• Lean on peers. “My initial step was to reach out to industry contacts to gather opinions and then narrow down our choices to two main contenders,” says Mr. Piquet. “Getting advice and hearing experiences from peers in the industry was huge in the beginning. Once I had that feedback it helped me go in a certain direction.”
Shadowing another practice that uses the same system can be beneficial. “It’s advisable to ask for references and visit those practices to get a better sense of the system’s effectiveness,” recommends Ms. Dey. “However, it’s important to remember that each practice’s environment is unique, and what works for one may not work for another. Many practices aren’t fully satisfied with their EHR systems, and better planning and understanding of limitations can help manage expectations and reduce frustration.”
• Invest in “super users.” “One thing that we’ve implemented within the past six months is the creation of an internal group called ‘super users,’ ” Mr. Piquet says. “This group consists of individuals who receive additional training and are considered the strongest users within our practice. A key strategy was to include physicians on the super-user team. When physicians provide efficiency tips to their peers, the advice is often received better than if it came from an administrator or trainer.
“This group also finds out what areas they’d like to see improved and what’s working well,” he continues. “This feedback helps us mold the system to better fit their workflows and provides tips for greater efficiency and accuracy to use the system as intended. ”
Change management happens from the top down, adds Ms. Lee. “You really need physician champions and key users from each group, from front desk to medical records to billing to technicians, and all the providers. Having your ‘super users’ in place and really using them as internal resources to help reduce staff anxiety and be the go-to folks on the ground during those first weeks and months when everyone’s acclimating.”
• Budget for a slowdown. ‘We started an escrow account early in the due diligence process to accumulate funds for the project,” says Mr. Kushner. “This helped cover revenue losses during training and go-live periods. You’re going to have a schedule reduction when you go live to allow staff enough bandwidth to get acclimated while they’re dealing with live patients. This inevitably leads to a revenue downturn. You need cash on hand, and the longer lead time you give yourself for that buffer to build up, the better off you’ll be.”
• Look at the process holistically. “We use the term ‘EHR migration’ almost like shorthand, but it’s really more accurately ‘system migration’ because quite often EHR migration will involve practice management migration,” says Ms. Lee. “Maybe there’s new payment processing that comes along with it. There’s certainly going to be new patient engagement tools that come along with it, and billing, and perhaps even a new clearing house for your claims. If it’s the EHR that’s driving the migration, obviously that should be front and center, but please don’t forget all of these other very, very important practice functions that are going to be impacted.”
• Don’t ignore the human aspect. “Change is difficult for everyone, and managing the human aspect of the transition is as important as the technical aspects,” says Ms. Dey. “Employees go through various stages of adaptation, from denial to acceptance, and eventually excitement. Supporting them through this process and recognizing the different paces at which people adapt can help ensure a successful transition and maintain staff morale.”
Dr. Boland, Ms. Dey, Mr. Kushner, Ms. Lee and Mr. Piquet have no disclosures related to this topic.





