Glaucoma surgery requires careful consideration of anesthesia options to ensure patient comfort and safety. Over the last decade, our approach to anesthesia has changed in terms of the agents and approaches used. Previously, most cases were performed under general anesthesia, but today it’s far more common for patients to undergo surgery with a combination of topical and injected anesthesia. In this article, I’ll discuss the anesthesia techniques for trabeculectomy, tube shunts and minimally invasive glaucoma surgeries, and how verbal anesthesia can increase patient cooperation and comfort.
Options
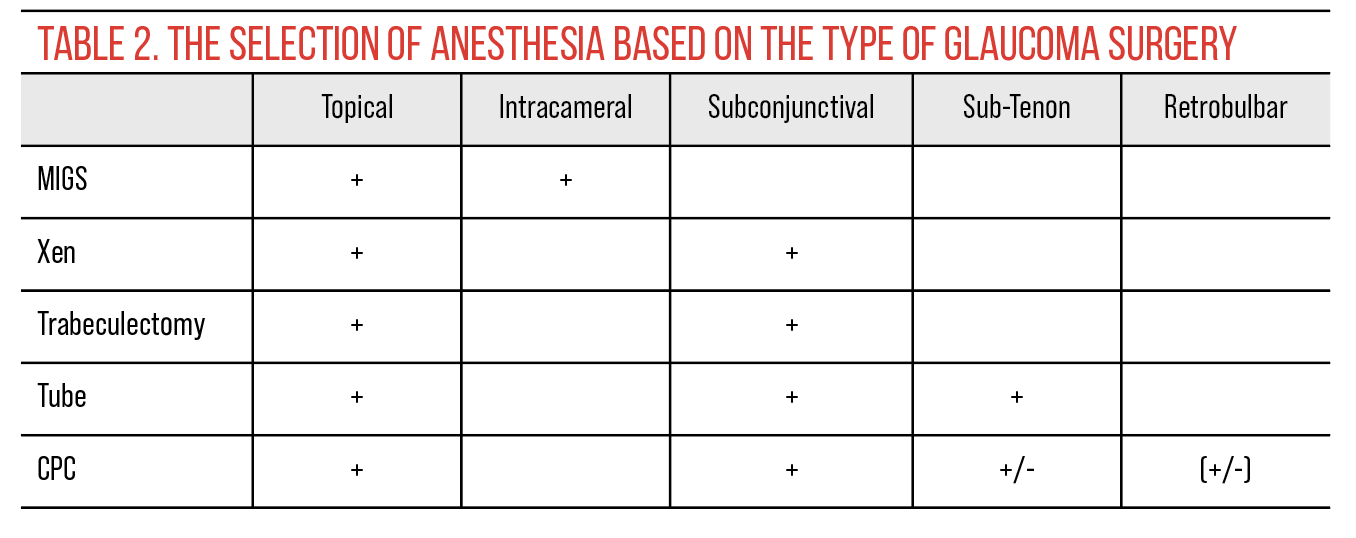
The most common techniques we use these days are topical, sub-Tenon peribulbar and subconjunctival injections. These anterior approaches provide adequate analgesia with reduced risk of sight-threatening complications. Surgeons must carefully evaluate patient tolerance, surgical requirements and the need for additional sedation with these approaches.
Retrobulbar anesthesia isn’t as commonly used as it once was, but we prefer to avoid the use of retrobulbar injection. While this posterior approach provides excellent akinesia and anesthesia, it carries a higher risk of sight-threatening complications, including globe perforation, especially in myopic patients who have larger eyes; optic nerve injury; brainstem anesthesia; and retrobulbar hemorrhage. The chance of retrobulbar hemorrhage seems to be higher in patients on any blood thinners, even a prophylactic dose of aspirin.
 |
Anesthetic Agents
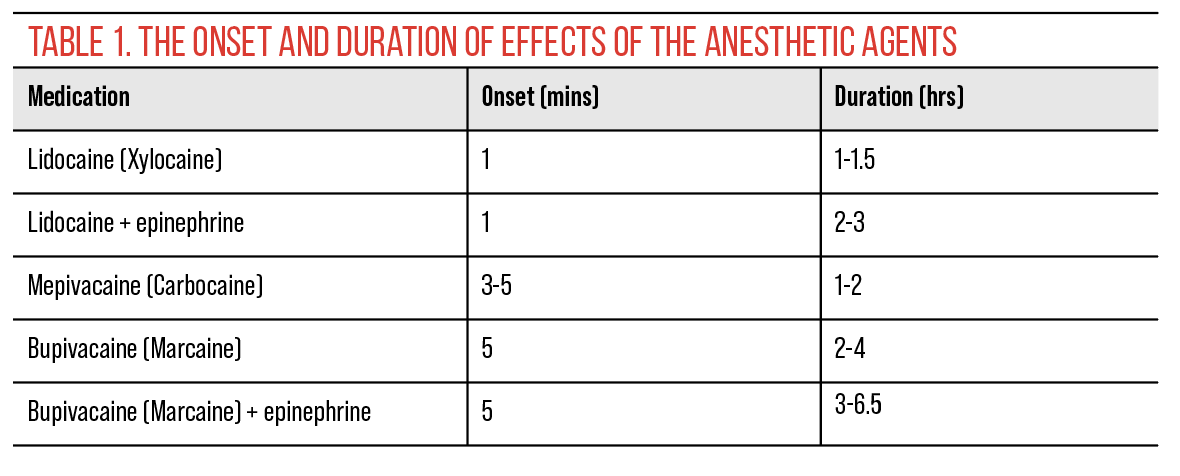
Anesthetic agents play a crucial role in patient comfort during surgery. Local anesthetics such as lidocaine, carbocaine, bupivacaine and ropivacaine are commonly used to achieve effective anesthesia. These may be administered alone, combined with each other, or with other agents such as epinephrine to increase duration of action and improve anesthesia.
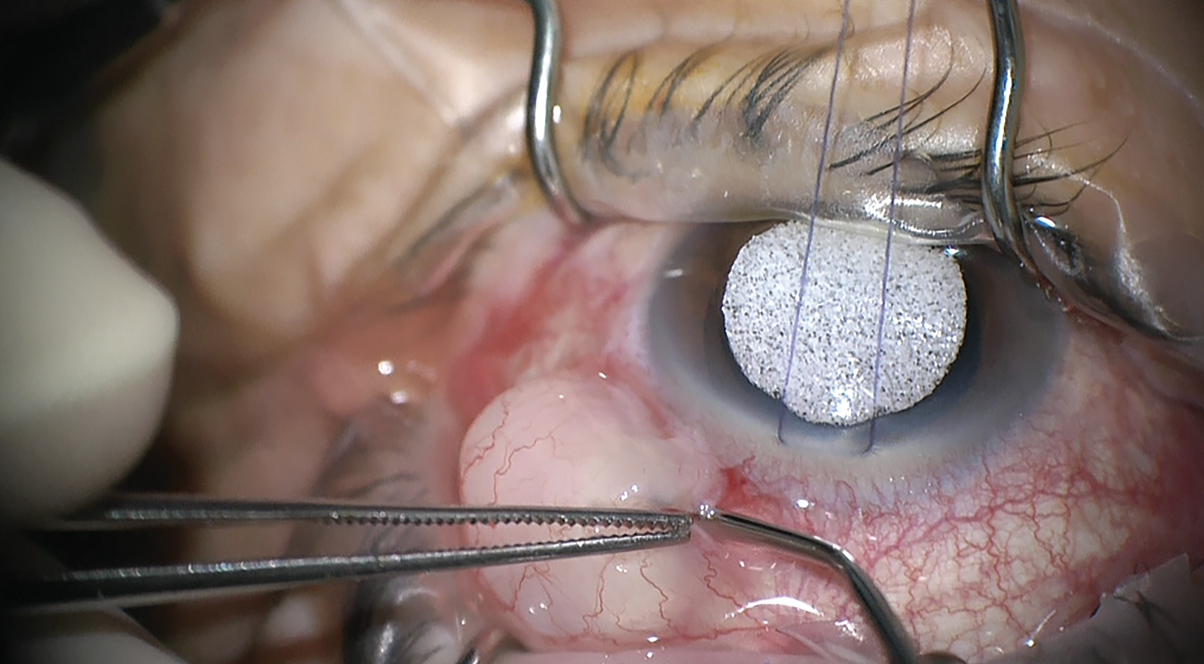
Trabs and Tubes
Subconjunctival and sub-Tenon injections are both suitable options for trabeculectomies and tube shunts. In trabeculectomy, it’s common to combine lidocaine with mitomycin and inject into the superior subconjunctival space. This provides enough anesthesia to complete the trabeculectomy.
All patients undergoing cataract or glaucoma surgery today also receive topical anesthetic agents, such as proparacaine or tetracaine and lidocaine gel. The gel provides anesthesia to the conjunctiva and the eyelid and helps during the initiation of surgery.
For the Xen procedure, we also use a combination of lidocaine and mitomycin. Some physicians consider using lidocaine plus epinephrine, which causes vasoconstriction, to decrease the chance for any subconjunctival hemorrhage during Xen implantation. This anesthetic agent combination is also used during trabeculectomy or tube revision to decrease the chance of bleeding.
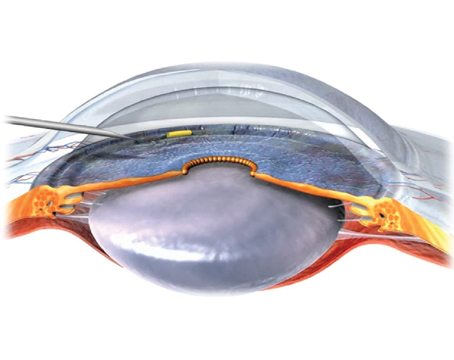
Sub-Tenon injections are widely used during tube shunt surgery. After making a small peritomy, a combination of lidocaine 2% plus bupivacaine 0.75% is instilled under Tenon’s. Many surgeons will add additional anesthetic after dissecting Tenon’s posteriorly, using a large blunt cannula to administer anesthesia in the retrobulbar and intraconal space before placing the shunt.
For any sub-Tenon injection, it’s safer to use a cannula rather than a needle after making a small peritomy. This decreases the chance for potential complications such as perforating vessels causing subconjunctival hemorrhage or globe penetration. The peritomy could be at the site of the tube implantation or inferonasally 4 to 5 mm posterior to the limbus.
 |
| The injection of anesthetic agent is performed using a cannula after making a small opening on the conjunctiva at the limbus. |
MIGS
MIGS procedures, due to their less invasive nature, often lend themselves to topical or intracameral anesthesia, though certain cases may warrant sub-Tenon injections or other approaches, depending on patient and surgical factors.
During the MIGS procedure we need patient cooperation to look away from the surgeon to get a good view to the angle, therefore no akinesia anesthesia is the preferred method. In MIGS patients, we generally use a topical agent, such as proparacaine, tetracaine or lidocaine gel, and inject preservative-free lidocaine 1% in the anterior chamber. Any intracameral anesthetic agents must be preservative-free to avoid complications such as toxic anterior segment syndrome or corneal endothelial toxicity.
Assessing Risks and Benefits
When selecting anesthesia techniques for glaucoma surgery, surgeons must carefully evaluate the potential risks associated with each option. A tailored approach may be needed in patients with significant comorbidities or anxiety, or in the event of complications.
During a phaco-MIGS procedure, for example, if the posterior capsule opens and the surgery requires more time to finish, sub-Tenon anesthesia may be needed to provide more comfort for the patient.
For patients undergoing cyclophotocoagulation, which is often painful even after the surgery, injecting subconjunctival bupivacaine is helpful. This gives the patient at least several hours of comfort after the procedure. Similarly, for tube shunts, because we perform more dissection and do device implantation, I also use bupivacaine combined with lidocaine or carbocaine to provide more patient comfort for a few hours postoperatively.
 |
Verbal Anesthesia
In addition to pharmacological anesthesia techniques, verbal anesthesia plays a key role in enhancing patient comfort and reducing anxiety during surgery. Effective communication with the patient and surgical team in the operating room can help clarify expectations and build trust.
Talking with patients before surgery in the preoperative area to give them an idea of what’s going to happen in the operating room will prepare them for the surgery and decreases their anxiety. During the procedure, offer encouragement. Telling patients things like “You’re moving” or “You’re not looking straight,” may elicit a negative response from the patient and induce more anxiety and stress, leading to a vicious cycle. Even in patients who aren’t cooperating, I find that encouragement helps them do better during the surgery. I usually tell patents, “You’re doing great. Everything looks good. We just need you to look at this light” or “You’re amazing. You’re one of my best patients.” Encouraging phrases like these help patients cooperate and feel less stress.
In summary, anesthesia management in glaucoma surgery requires weighing the advantages and disadvantages of certain techniques against patient-specific factors and surgical considerations. Understanding the nuances of each anesthesia option and using encouragement in the operating room can optimize outcomes and enhance the overall experience for patients undergoing glaucoma procedures.
Dr. Razeghinejad is a glaucoma specialist and director of the Glaucoma Fellowship Program at Wills Eye Hospital in Philadelphia. His institution has received research grants from Olleyes and Equinox.
Dr. Singh is a professor of ophthalmology and chief of the Glaucoma Division at Stanford University School of Medicine. He is a consultant to Alcon, Allergan, Santen, Sight Sciences, Glaukos and Ivantis. Dr. Netland is Vernah Scott Moyston Professor and Chair at the University of Virginia in Charlottesville.