Even the best products and experiences in life will fall short of expectations from time to time: Your new sedan doesn’t shift gears crisply enough, the summer home’s air conditioning never seems to work when you want it to, and yes, sometimes, a patient’s vision with a new premium intraocular lens isn’t as good as he’d hoped it would be. Whether the problem is with the patient, the surgery or a mix of both, it’s your job to ferret out the cause and correct it as best you can. In this article, I’ll share some techniques that will help.
A Rare Problem
The reality is that the vast majority of patients receiving premium intraocular lens implants are very happy and would have the procedure again. In fact, patients are very likely to recommend a modern premium lens to friends and family—as many as 94 percent in the Concerto Study and 98 percent in the Harmony Study.1 In the U.S. FDA trials for newer-generation multifocal IOLs, 94 to 97 percent would choose to have the lens again as compared to only 88 percent with a monofocal lens.2 But, for those who aren’t fully satisfied with their quality of vision, uncorrected vision or function after premium lens implants, we need to be able to address our patients’ concerns and symptoms.
Preop Measures
There’s an old maxim among playwrights who are struggling with a script: “Third-act problems are actually first-act problems.” The same is true in many cases of less-than-successful premium IOL surgery. Thoroughly discussing the pros and cons of the procedure with patients ahead of time, and performing a careful exam, can avoid many postop issues.
• Talk to the patient. The first step to better patient satisfaction with premium IOLs is to talk and listen to the patient and understand what she expects to achieve through the surgery. Be sure to conduct a thorough exam, review all of the patient’s measurements and engage in a detailed discussion about the surgical options. During this discussion, it’s important to get to know the patient’s personality, occupation, hobbies and visual needs. The surgeon should also explain to the patient what each lens or surgical procedure is capable of achieving and the true limitations of the technology, with a heavy emphasis on the fact that no surgery or lens can do everything for everyone.
It’s also very important to understand what the patient’s goals are after surgery—not just what your goals are for him. Some individuals are perfectly fine wearing glasses after surgery and don’t feel the need to spend the extra money on premium lenses or femtosecond l
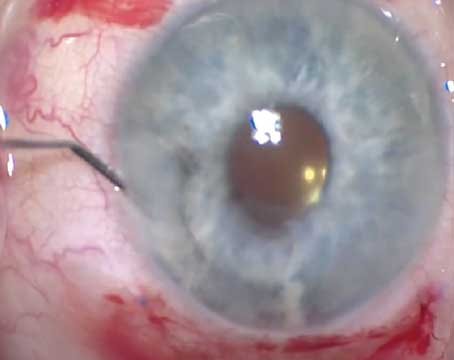
 |
| When preparing the ocular surface for premium surgery, conditions such as this pterygium must be treated. |
asers. Others would prefer to see well at near and wear glasses for distance activities, while some patients prefer high quality daytime and night vision with glasses rather than good vision without correction for near and distance. Along these lines, I’m reluctant to recommend MF IOLs when the patient is very happy with monovision; the use of multifocal IOLs not only adds the need for the patient to neuro-adapt to manage postop tasks, but patients also have to pay extra for the lenses.
• The exam. Preoperatively, you have to evaluate every patient carefully, looking at everything from the ocular surface to the macula. When considering IOLs, be sure to choose the correct technology for a patient’s current refractive error and his visual needs and wants. In the end, patients may not be good candidates for premium lenses due to either their clinical findings or their expectations and ability to function within the limitations of the current premium IOL technology.
On clinical examination, I look for ocular surface issues like dry eyes, poor tear film, epithelial basement membrane dystrophy, Salzmann’s nodular degeneration and pterygium. If any of these are present, I address them preoperatively. I’ll initiate aggressive dry-eye treatment with artificial tears, lid hygiene, oral omega-3 fatty acids and topical anti-inflammatory drops (i.e., Lotemax, Restasis or Xiidra). If there is EBMD or SND present, I treat these surgically with a burr keratectomy preoperatively and won’t proceed with surgery until the ocular surface is healthy and the refraction is stable. We’ve seen refractive improvements of up to 1.25 D (mean: 0.64 D) after EBMD treatments, and up to
6 D sphere (mean: 1.71 D) and 4.5 D of cylinder (mean: 1.57 D) after treating SND. (For more on these treatments, see “The Benefits of Pre-treating Corneas” in Review’s April 2010 issue).
If there’s any significant pterygia present, we prefer to treat these first with excision and conjunctival autografts. It takes two to three months for the refraction to stabilize after these procedures—sometimes longer if there is any concurrent dry eye or lid margin disease.
A detailed dilated exam is important for ruling out any macular or optic nerve disease. The most common finding that prevents the implantation of premium IOLs is visually significant epiretinal membrane formation or macular degeneration. Not only can ERM affect patients’ best-corrected vision and quality of vision, there is also a higher risk of cystoid macular edema that should alter your postoperative drop regimen to include an NSAID for at least six weeks postop.3,4
If the ERM is mild, optical coherence tomography can help determine if it’s clinically significant. Due to some loss of contrast sensitivity with multifocal IOLs (less so with extended-depth-of-focus lenses) and imaging artifacts, the visual function and postop OCT measurements may be less reliable. There may also be zonular instability in glaucoma patients that could affect the long-term centration of the IOL. The other concern is that the ERM or glaucoma can progress, so even mild cases of ERM or glaucoma may not have excellent long-term outcomes with multifocal and EDOF lenses. For these reasons, we’re cautious in recommending multifocal and EDOF lenses in patients with macular or optic nerve diseases. I’m more comfortable with monofocal toric IOLs in these cases, as long as there’s no zonulopathy.
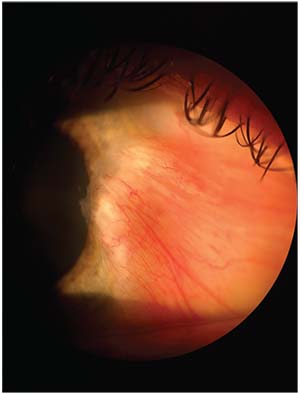
Once we determine that the patient is a good candidate for a premium lens based on the clinical exam, we then review all the measurements and studies to rule out irregular astigmatism, abnormal topography and high Purkinje vs. limbal chord lengths. Regarding the last factor, I evaluate the distance between the center of the limbus, or horizontal white-to-white measurement, (i.e., the optical center) and the corneal apex (i.e., the visual axis). If this distance is greater than 0.5 mm, then there will be some induced higher-order aberrations and decreased quality of vision. In my own case series, we found a higher percentage of 20/20 uncorrected visual acuity at near and distance when this value was less than 0.5 mm. This measurement is also helpful with toric IOLs and even aspheric monofocal IOLs—not just multifocal/EDOF lenses.
If the topography shows irregular astigmatism or signs of ectasia, I avoid presbyopic IOLs; however, I may consider a toric IOL to reduce the cylinder, but only after a detailed discussion explaining the “off-label” use and the expectation of some residual astigmatism.
Premium IOL surgery is, in effect, refractive
 |
| If the distance between the optical center and visual axis (angle alpha) is greater than 0.5 mm, more aberrations will be induced. This multifocal IOL is centered on the visual axis and has a low angle alpha measurement. |
surgery, and patients should be screened in the same way as they would for a LASIK evaluation, since enhancements must be an option to correct any residual refractive error. This means that the ocular surface and topography/tomography should be normal and that there should be no contraindications for laser vision correction. If the patient is not an LVC candidate, then he should be educated preoperatively that there may be limited options after surgery to fully correct his vision.
The extra time and effort taken to educate the patient preop will reduce the number of postop issues and also help screen out patients that may not be a good fit for premium lenses.
• Formula factors. Although enhancements are a reality with IOL surgery, by using modern IOL formulas like the Hill-RBF and the Barrett Universal formula, advanced biometry from the IOL Master 700 or Lenstar, and multiple K readings, you can reduce the number of refractive surprises you experience. I personally use multiple formulas and review the K readings from three different devices (IOL Master 700, Pentacam and Tracey iTrace) before calculating the IOL power. If the measurements have outliers, such as long or short axial lengths, high or low Ks, or narrow chamber depths, inform the patient that she is more likely to need an enhancement once the refraction is stable. If there’s a big difference between the two eyes or between the measurements, then this may be a sign that the ocular surface is unstable.
Intraoperative Tips
“Perfect” cataract/intraocular lens surgery without complications is always the goal, especially with premium IOL implants. To make the surgery as precise as possible, we prefer to use a femtosecond laser, the Catalys, for all premium IOL cases. We address corneal astigmatism with an intrastromal astigmatic keratotomy procedure or make preop corneal marks to facilitate toric IOL alignment. We also reduce the capsulotomy from a standard diameter of 5 mm down to 4.8 mm for toric IOLs (both monofocal and extended-depth-of-focus) to reduce the incidence of IOL rotation postoperatively. In addition, I prefer to fragment the lens in order to reduce elapsed phaco time and achieve clear corneas on postop day one.5,6,7
The Postop Period
Even when you follow the aforementioned advice, there may still be the occasional patient who is unhappy.
When meeting with a dissatisfied premium IOL patient, you shouldn’t become defensive or dismissive of his complaints. It’s critical to listen to his issues early and often in order to understand his concerns and create a game plan to address the issues. I’ve seen a handful of unhappy premium IOL patients whose visual function could have been markedly improved with a couple of very simple treatments—but they were either not offered or the patient didn’t understand what he was being offered.
It’s also important to understand the duration and timing of the complaints, since some issues will improve over time with neuroadaptation and some may be chronic and need to be addressed. For instance, night-vision disturbances and learning how to function better at near tasks definitely improve during the first three to six months postop. In many cases in which premium IOL patients are unhappy with their results, after listening to them carefully and being their advocate, we’re able to allay their fears and regain their trust. This helps us educate them on the limitations of the lens technology that they had implanted. In doing so, we’ve been able to improve their visual function. Since no premium lens is perfect, there may be cases in which the best solution is to exchange the lens for a standard IOL. This is the exception, however, and I typically only recommend this if all the other less-invasive options have been exhausted.
In the postop period, there are several areas that can be addressed to improve patient satisfaction and function with premium lenses:
• Ocular surface disease. The ocular surface can severely affect the quality of vision, patient comfort and visual function, and any problems with the surface should always be treated aggressively. Dry eyes are very common, and the ocular surface should be fully rehabilitated to improve patient satisfaction, and to prepare the eye for an enhancement, if needed.
• Residual refractive error. This is the most common reason patients aren’t functioning well without correction postop. Residual refractive error affects everything: near; intermediate; distance; and night vision. If there’s a high spherical refractive error, then an IOL exchange or secondary piggyback IOL are good options. I prefer an IOL exchange over piggyback lenses unless the capsule or zonules aren’t intact.
For compound or mixed astigmatism, LASIK and PRK are excellent options. I prefer LASIK if the patient is a good candidate, due to the quicker visual recovery and comfort. If the patient has mixed astigmatism with an essentially plano spherical equivalent, then you can offer an AK or LRI, either of which works well if the cylinder is undercorrected from the surgery.
If there’s residual cylinder after a toric IOL, I determine if the IOL is on the ideal postop axis; if it isn’t, then I’ll use one of the many online calculators (such as www.astigmatismfix.com and www.assort.com) or instrumentation that assesses the proper alignment of the lens and the expected residual refractive error (such as the iTrace or the OPD-Scan III from Nidek). If I determine that there will still be significant residual refractive error even after ideal alignment of the IOL, then I prefer an LVC enhancement to avoid needing two separate surgeries.
If a cornea-based enhancement is necessary, the ideal time is about six weeks postop to allow for the refraction and ocular surface to stabilize. If you’re going to be rotating a toric IOL, I recommend doing this one to two weeks postop but not earlier, as the IOL can shift again if the rotation is performed too soon postoperatively. If there is any zonular instability or decentration of the lens or high axial lengths/WTW measurements, I prefer to place a capsular tension ring at the time of the rotation to reduce the risk of recurrent rotation.
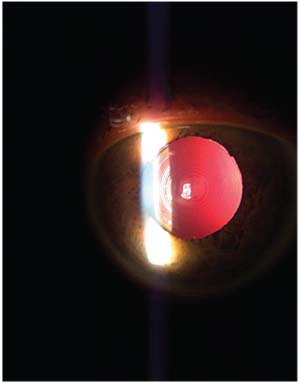
• Posterior capsular opacification. If there’s any significant PCO present and there are night-vision difficulties or quality-of-vision complaints, a YAG capsulotomy is indicated. This can be performed as soon as six weeks postoperatively, but it’s best to wait longer to ensure that the IOL is stable and to reduce the potential for developing CME. You should also wait on performing a posterior capsulotomy if you’re still considering an IOL exchange or rotation.
• Cystoid macular edema. An SD-OCT is indicated to rule out CME; if detected, CME must be treated until fully resolved. If ERM is present and thought to be a cause of persistent CME or decreased quality of vision, then consider a referral to a retinal specialist.
• Neural adaptation. We expect patients’ near vision and night vision to improve over time. It may take them three days, three months or six months to adjust and learn how to adapt to their new vision. Some patients may not ever adapt and, for them, we should be ready to exchange a multifocal or EDOF lens for a monofocal IOL.
• Good surgery, wrong patient. Often, the surgery is nearly perfect, with excellent outcomes as predicted … but the patient still isn’t satisfied. Maybe he’s not tolerant of night-vision difficulties or isn’t willing to give his problems a chance to resolve over time, or maybe he expected a perfect range of vision from near to far during both day and night. Many patients are disappointed if they need glasses for any function, even if you informed them multiple times preoperatively that they shouldn’t expect to be 100-percent free of spectacle correction for all activities. For these patients, it’s a challenging discussion after surgery and, therefore, it’s best to do all you can preoperatively to avoid these situations, and then do all you can after surgery to optimize their outcomes, given the inherent limitations of the technology we have available today.
In summary, premium IOLs have come a long way in the past decade, and can provide excellent visual function and spectacle independence for the great majority of patients. Some, however, will not be happy with their outcomes. A detailed history, examination, biometry/IOL calculations and discussion are critical to preventing misunderstandings and poor outcomes with premium lens implants. In completing this process, treat a premium lens patient like a refractive surgery patient in terms of her preop evaluation, and make it a point to rule out conditions that may lead to poor outcomes or limit her options for improving her vision after surgery.
The only way to completely eliminate unhappy postoperative premium lens patients from our practice is to not perform the surgery. However, by using the preop, intraop and post-op management tips outlined in this article, you can expect very high success rates and patient satisfaction with premium IOLs. REVIEW
Dr. Piracha is an associate professor of ophthalmology at the University of Louisville and the University of Kentucky. He is a consultant to Carl Zeiss Meditec.
1. DOF2016CT0024 (Concerto Study Report) and DOF2015OTH0009 (Symfony Harmony Observational Study).
2. Patient information brochure: J&J Tecnis ZKB00 and ZLB00.
3. Henderson BA, Kim JY, Ament CS, et al. Clinical pseudophakic cystoid macular edema. Risk factors for development and duration after treatment. J Cataract Refract Surg 2007;33:9:1550-1558.
4. Wittpenn JR, Silverstein S, Heier J, et al. A randomized, masked comparison of topical ketorolac 0.4% plus steroid vs steroid alone in low-risk cataract surgery patients. Am J Ophthalmol 2008;146:4:554-560.
5. Conrad-Hengerer I, Hengerer FH, Al Juburi M, Schultz T, Dick HB. Femtosecond laser-induced macular changes and anterior segment inflammation in cataract surgery. J Refract Surg 2014;30:4:222-6.
6. Hengerer FH, Dick HB. Corneal endothelial cell loss and corneal thickness in conventional compared with femtosecond laser-assisted cataract surgery: Three-month follow-up. J Cataract Refract Surg 2013;39:1307–1313.
7. Takacs AI. Central corneal volume and endothelial cell count following femtosecond laser-assisted refractive cataract surgery compared to conventional phacoemulsification. J Refract Surg 2012; 28:387–39.