The term dry-eye syndrome (DES) refers to a heterogeneous set of conditions, all characterized by inadequate lubrication of the ocular surface. Most commonly, a deficiency of one or more of the tear-film layers (aqueous, mucin or lipid) is involved, due to low tear production by the lacrimal glands (aqueous deficiency) or poor tear quality/tear-film instability involving meibomian gland dysfunction (evaporative loss). Dry-eye signs and symptoms can be caused by certain drugs, lid abnormalities or epithelial cell defects from infection or trauma. Dry eye can also be associated with systemic diseases such as Sjögren's syndrome.
The symptoms of dry eye vary considerably from patient to patient. Most patients have mild to moderate symptoms, including ocular discomfort, foreign body sensation, burning, stinging, grittiness, photophobia, blurring, tired eyes and contact lens intolerance. In some patients, symptoms are debilitating. Either way, DES is one of the main reasons that patients visit eye doctors in the United States.1
Determining the prevalence of DES is complicated by the lack of a gold standard for diagnosis; moreover, each study seems to use different criteria. In addition, the results of clinical tests for dry eye, such as staining with fluorescein, sometimes do not match up with patients' reports of symptoms. This may be related to how the disease progresses. For example, in the early stages, there is less ocular surface damage and the cornea is still quite sensitive, resulting in less staining but worse symptoms. In later stages, patients may show severe ocular surface damage, but their decreased corneal sensitivity means their discomfort may actually be less. (Casavant J, et al. IOVS 2005;46:E-Abstract 4455)
Depending on how it is defined and the population studied, the prevalence of DES is anywhere from 6.7 percent (among women ages 49 to 89, with severe symptoms or a previous clinical diagnosis) to 28.7 percent (for both sexes, age under 10 to over 80, who self-reported symptoms at optometry clinics).2,3 Women are 1.5 to three times more likely than men to have the condition.4,5 Most cases are seen after menopause, but women with premature ovarian failure also have a higher risk of dry eye.6 There also appears to be an increased incidence in pregnant and lactating women, although further research is needed to establish a clear connection between associated low androgen levels and dry eye with these physiological states.7
Historically, researchers thought that low estrogen levels after menopause must be to blame for the higher rates of DES in older women. However, more recent research has explored the role of androgens. You'll recall that androgens are sex hormones that are present in both men and women, and their levels decrease as we age. Because women have lower levels of androgens to start with, age-related decreases may push levels below the amount needed for optimum eye health.
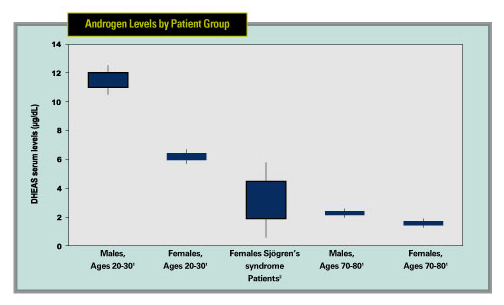 |
| Dehydroepiandrosterone sulphate (DHEAS) is one of the main adrenal androgens. Serum levels of DHEAS are lower in women with Sjögren's syndrome, older men and older women. Although these data are from different studies and populations, the data are suggestive of a trend. Because androgens regulate the lacrimal and meibomian glands, some researchers have theorized that androgen levels play a part in dry eye. 1. Labrie F, Belanger A, Cusan L, et al. Marked decline in serum concentrations of adrenal C19 sex steroid precursors and conjugated androgen metabolites during aging. J Clin Endocrinol Metab 1997;82:8:2396-402. 2. Valtysdottir ST, Wide L, Hallgren R. Mental wellbeing and quality of sexual life in women with primary Sjogren"s syndrome are related to circulating dehydroepiandrosterone sulphate. Ann Rheum Dis 2003;62:9:875-9. |
Recent studies have suggested that androgen deficiency may be the main cause of the meibomian gland dysfunction, tear-film instability and evaporative dry eye that are characteristic of Sjögren's syndrome, which occurs almost exclusively in women.8 Androgens are known to regulate the immune system, as well as the morphology and secretory functions of lacrimal glands. Androgens also regulate the meibomian glands, which are the primary tissues involved in maintaining tear-film stability and preventing tear-film evaporation.9 Receptors for androgens, estrogens, progesterone and prolactin have been identified in several ocular tissues in rats, rabbits and humans. Human meibomian and lacrimal glands contain androgen receptor mRNA, androgen receptor proteins and several enzymes that may convert testosterone or metabolized androgens into other androgenic forms.10
Some dry-eye patients have immunological disorders, such as lymphocyte infiltration into the lacrimal gland and conjunctiva. In one study, patients with poor reflex tearing were shown to be more likely to have autoantibodies and lymphocytic infiltration.11 This may be due to ocular distress from desiccation, leading to damaged cells and the release of pro-inflammatory cytokines. The resulting inflammatory response exacerbates the symptoms of dry eye. Since hormones normally suppress inflammation and proteolytic enzymes, a hormone imbalance may cause these proteases to be more active.
The influence of hormone replacement therapy in menopausal women remains unclear, as some authors support the idea that it improves the quality and the volume of the tear film, whereas others have shown that it increases the risk of dry eye. It's possible that HRT may alleviate postmenopausal dry-eye symptoms by increasing goblet cell density.12 However, other studies suggest that HRT worsens dry-eye symptoms in some cases, and estrogen-only HRT seems to be worse than a combined estrogen and progesterone therapy. Data from the Women's Health Study suggests a 69-percent increased risk of dry eye associated with post-menopausal estrogen therapy and a 29-percent higher risk for women taking estrogen plus progesterone therapy.13
Treating Dry Eye
Over the last 10 years, there have been many advances in dry-eye drug therapy, including the introduction of numerous over-the-counter artificial tears such as Systane (Alcon), Soothe (Alimera), GenTeal Gel (Novartis) and the Refresh line of products (Allergan). The arrival of prescription Restasis (Allergan) was another welcome addition for severe dry-eye patients, and clinicians eagerly await new developments from the drug pipeline, such as Inspire's diquafosol tetrasodium and Novartis' pimecrolimus.
Systane occupies a niche between tear substitutes and prescription treatment, and is available over-the-counter. Systane contains the demulcents polyethylene glycol and propylene glycol, along with the gelling agent hydroxypropyl guar (HP-guar). In the eye, the emulsion forms a matrix that holds the lubricants in place on the ocular surface. This helps provide a soft, protective coating, lubricating the blinking process and facilitating tissue repair. In an Alcon-sponsored study, the combination of ingredients in Systane resulted in a very low coefficient of friction and very high lubricity rating.14
Allergan is also conducting clinical trials in Europe and the United States to see if topical androgens are effective in treating dry eye. Given what we now know about androgen deficiencies in Sjögren's syndrome and other dry-eye disorders, it seems plausible that rectifying endocrine imbalances may prove beneficial for patients with lacrimal and meibomian gland dysfunction and associated dry eye. It has been shown that testosterone levels correlate positively with tear function in postmenopausal women and negatively in younger patients, suggesting that postmenopausal women with DES may benefit from testosterone replacement.15
There have not yet been any published results of using testosterone replacement specifically for dry eye, but a few case reports seem to suggest the approach could have merit.16,17 Additionally, in a recent retrospective case series study of 11 postmenopausal women who received a combination HRT consisting of esterified estrogen and methyl testosterone, 91 percent noticed a decrease in their dry-eye syndromes after an average of 4.1 months of therapy.18
Looking at all the evidence, it seems clear that hormones in general, and androgens in particular, represent an important trophic factor for the ocular surface, and that their deficiency predisposes to inflammation. Knowledge of these interactions between hormones and the lacrimal and meibomian glands may become increasingly essential for understanding dry-eye diseases. Further study of these relationships may result in new and improved treatments.
Dr. Abelson, an associate clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at Schepens Eye Research Institute, consults in ophthalmic pharmaceuticals. Ms. Lines is a medical writer at ORA Clinical Research and Development in North Andover.
1. Lemp MA. Epidemiology and classification of dry eye. Adv Exp Med Biol 1998;438:791-803.
2. Caffery BE, et al. The Canadian dry eye epidemiology study. Adv Exp Med Biol 1998;438:805-6.
3. Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am J Ophthalmol 2003;136:318-326.
4. Chia EM, Mitchell P, Rochtchina E, et al. Prevalence and associations of dry eye syndrome in an older population: The Blue Mountains Eye Study. Clin Exp Ophthalmol 2003;31:3:229-32.
5. Moss SE et al. Prevalence and risk factors for dry eye syndrome. Arch Ophthalmol 2000;118:9:1264-8.
6. Smith JA, Vitale S, Reed GF, et al. Dry eye signs and symptoms in women with premature ovarian failure. Arch Ophthalmol 2004;122:2:151-6.
7. Schecter JE, Pidgeon M, Chang D, et al. Potential role of disrupted lacrimal acinar cells in dry eye during pregnancy. In: Sullivan D, ed. Lacrimal Gland, Tear Film, and Dry Eye Syndromes 3. Boston: Kluwer Academic/Plenum Publishers, 2002:153-157.
8. Sullivan DA, Belanger A, Cermak JM, et al. Are women with Sjogren's syndrome androgen-deficient? J Rheumatol 2003;30:11:2413-9.
9. Sullivan DA, Yamagami H, Liu M, et al. Sex steroids, the meibomian gland and evaporative dry eye. Adv Exp Med Biol 2002;506A:389-99.
10. Sullivan DA, Sullivan BD, Ullman MD, et al. Androgen influence on the meibomian gland. Invest Ophthalmol Vis Sci. 2000 Nov; 41:12:3732.
11. Tsubota K. Decreased reflex tearing is associated with lymphocytic infiltration in lacrimal glands. J Rheumatol 1996;23:2:313-20.
12. Pelit A, Bagis T, Kayaselcuk F, et al. Tear function tests and conjunctival impression cytology before and after hormone replacement therapy in postmenopausal women. Eur J Ophthalmol 2003;13:4:337-42.
13. Schaumberg DA. Hormone replacement therapy and dry eye syndrome. JAMA 2001;286:2114.
14. Christensen MT, Stein JM, Stone RP, et al. Evaluation of the effect of tear film break-up time extension by artificial tears in dry eye patients. Abstract presented at 23rd Biennial Cornea Research Conference. Oct 3-4, 2003.
15. Mathers WD, Stovall D, Lane JA, Zimmerman MB, Johnson S. Menopause and tear function: The influence of prolactin and sex hormones on human tear production. Cornea 1998;17:4:353-8.
16. Bizzarro A, Valentini G, Di Martino G, et al. Influence of testosterone therapy on clinical and immunological features of autoimmune diseases associated with Klinefelter's syndrome. J Clin Endocrinol Metab 1987;64:32–36.
17. Worda C, Nepp J, Huber JC, Sator MO. Treatment of keratoconjunctivitis sicca with topical androgen. Maturitas 2001;37:209–212.
18. Scott G, Yiu SC, Wasilewski D, et al. Combined esterified estrogen and methyl testosterone treatment for dry eye syndrome in postmenopausal women. Am J Ophthalmol 2005;139:6:1109-10.



