Accuracy in refractive surgery is a paramount goal for both surgeon and patient. “As refractive surgeons, the pressure has always been on us to get an exact result,” says Andrew I. Caster, MD, a refractive surgeon in Beverly Hills, California. “We’ve always told patients that there’s some degree of variability and that a certain percentage are going to need to have a touch-up done, but the onus of keeping that touch-up number as low as possible has always been on us.”
Nomograms can help better predict the outcomes of corneal-refractive surgery and can minimize the need for enhancements. These equations may be adjusted depending on various factors, including laser, patient demographics, surgeon and environment, to name a few. And although many surgeons in the early days of refractive surgery may have relied on Excel spreadsheets for their personal nomograms, they can now take advantage of nomogram software that synthesizes data from more surgeons and makes it accessible to others.
We spoke with a few refractive surgeons about the necessity of nomograms, the variables to consider when making adjustments and how shared nomograms are impacting results.
The Role of Nomograms
Commercially available laser systems take into account their own technical specifications, as well as surgical technique, operating room environment and patient demographics.1
“In medical procedures, calculations and processes are established to produce a desired outcome,” says Kevin M. Miller, MD, of the Stein Eye Institute at the University of California Los Angeles. “However, realized outcomes often differ from desired outcomes because biological and environmental differences from person to person, site to site, and machine to machine exist. Variability in wound healing from one individual to another is an example. A nomogram considers the actual outcomes of a procedure and modifies either the inputs to the calculations and processes, or the calculations and processes themselves, in an endless feedback loop that drives the system toward the desired outcome with each iteration.”
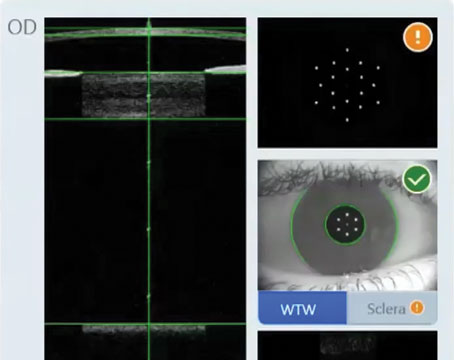
 |
| Shared nomogram software, such as this one from SurgiVision (enlarged to show detail), is constantly updated with data and can be personalized with different variables. Here, the software shows the surgeon the amount to program and the predicted outcome, as well as the results of the most recent eyes they operated on. (Courtesy Kevin M. Miller, MD) |
Nomograms also evolve constantly as techniques and technology change over time. “When I first started performing LASIK, which was back in 1996, I wrote my own program for nomograms, but it just did a linear analysis,” recalls Dr. Caster. “Now the new programs do binomial analyses so they’re more accurate.”
Nomograms can’t be developed without the diligent tracking of outcomes, says Lisa McIntire, MD, CEO of Speck Eye Care in Austin, Texas. “In the early days, the best surgeons—the ones who got the best outcomes and did the best work—were tracking their outcomes in an Excel spreadsheet,” she says. “And I say the very best ones because not everybody did it. Not everybody tracked outcomes at all, and not everybody tracks outcomes today and that is the truth. Not everybody does it. It’s the best way to get the best results, but it takes more time and it takes effort. You need to hire someone to upload data into these nomograms and use technician time to take these extra steps or maybe do it yourself. But I believe that it’s of the utmost importance as we try to standardize and universally improve outcomes across our industry that we really hold ourselves accountable to these higher standards.”
Dr. Miller says surgeons feed those outcomes into a nomogram and the nomogram adjusts the inputs so that the desired outputs are achieved. “Even knowing that lasers become better with each successive generation, there will always be variables that make one laser different from another laser, and outcomes with the same laser differ from one part of the world to another,” he says.
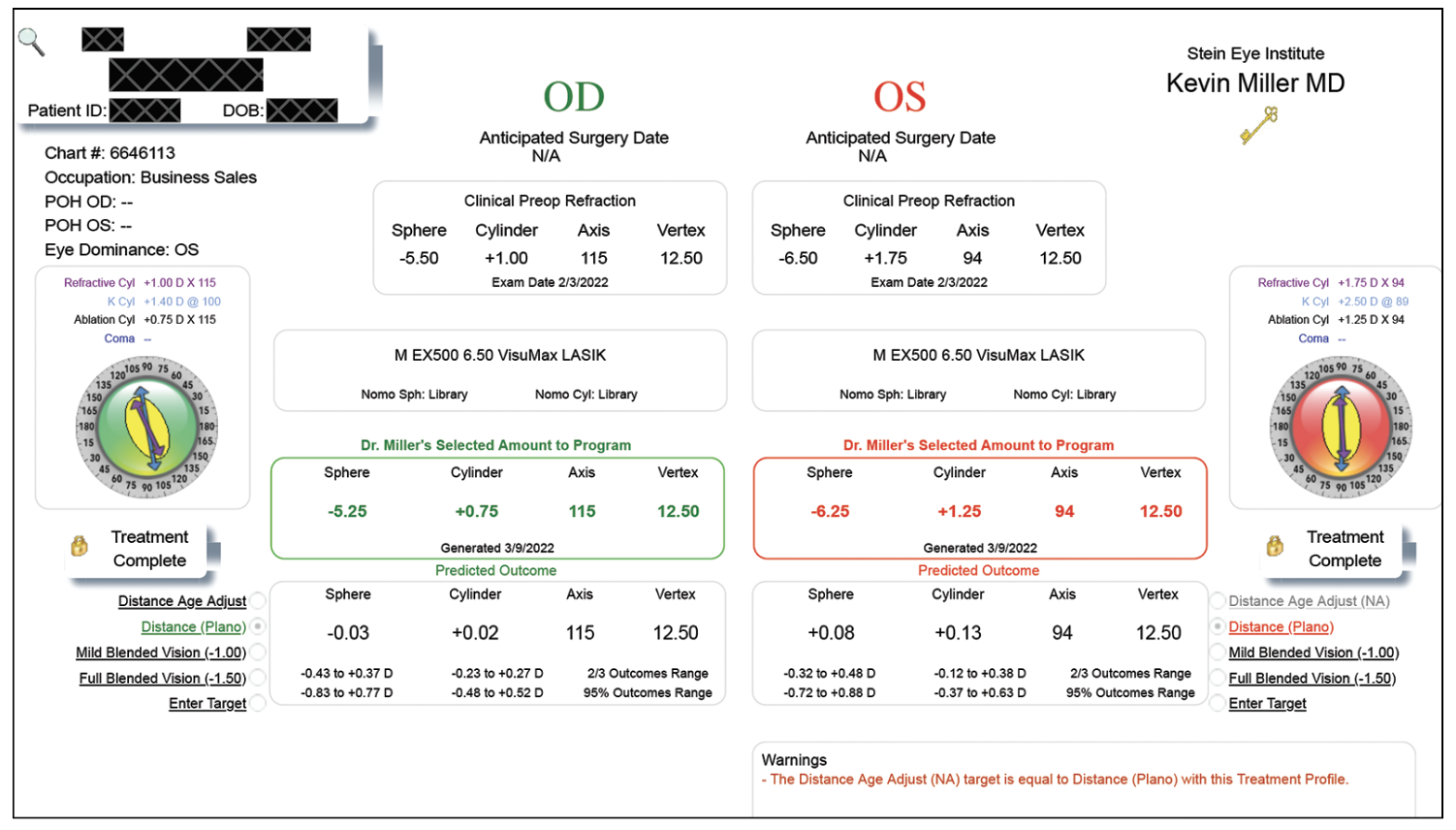
 |
| An example of the IBRA refractive nomogram software that shows the proposed treatment plan for the surgeon to program based on the nomogram chosen and the predicted outcome. (Courtesy Mitra Nejad, MD) |
Variables to Consider
There’s no one right way to design a nomogram, but the more variables a surgeon includes in the equation, the more likely the outcome is to be successful.
The basis for any refractive surgery nomogram must include the variables for manifest refraction values: sphere; cylinder; and axis.
“In the case of refractive surgery (LASIK, PRK, SMILE), the primary input to a laser is the patient’s refractive error,” says Dr. Miller. “Surgeons enter the spherical and cylinder errors and the axis of the cylinder, and these entries constitute the primary basis for treatment. Optical zone diameter and flap or cap thickness, in the case of LASIK and SMILE, are secondary inputs. Now, if a surgeon enters the refractive error ‘straight up’ with no adjustment, odds are the laser he or she uses will produce a slightly different outcome than the expected one. The greater the refractive error, especially the cylinder error, the greater likelihood of an outcome error.”
Most lasers will be very precise and produce the exact same output every single time they fire, he continues. “This may not be true, however, if a laser is out of calibration or the temperature and humidity in the treatment room are out of range,” says Dr. Miller. “Because biological and environmental variations exist, however, even if one enters the same correction for 100 different eyes with the exact same refractive error, after the treatments are done, one will observe variability in the outcomes, both in terms of accuracy and precision. So, to improve the results, the surgeon has to look at the mean resultant error, determine how much it’s off, and figure out how to tweak the inputs or the treatment calculations to get the desired output.”
Dr. Caster adds that nomograms can counter those situations when a laser isn’t completely accurate. “For instance, with the EX500 (Alcon) that I use, the laser runs a little cold on the lower end of the myopia range and it runs a little hot on the upper range,” he says.
“All lasers tend to be pretty accurate at treating low spherical errors, but at higher spherical and cylinder errors, they tend to start benefiting from nomogram adjustments,” says Dr. Miller. “This is especially true of high cylinder errors.”
In a retrospective analysis,1 a group of researchers constructed seven nomograms based on the sphere, cylinder and axis of 150 consecutive eyes treated with LASIK for myopic astigmatism (Table 1).
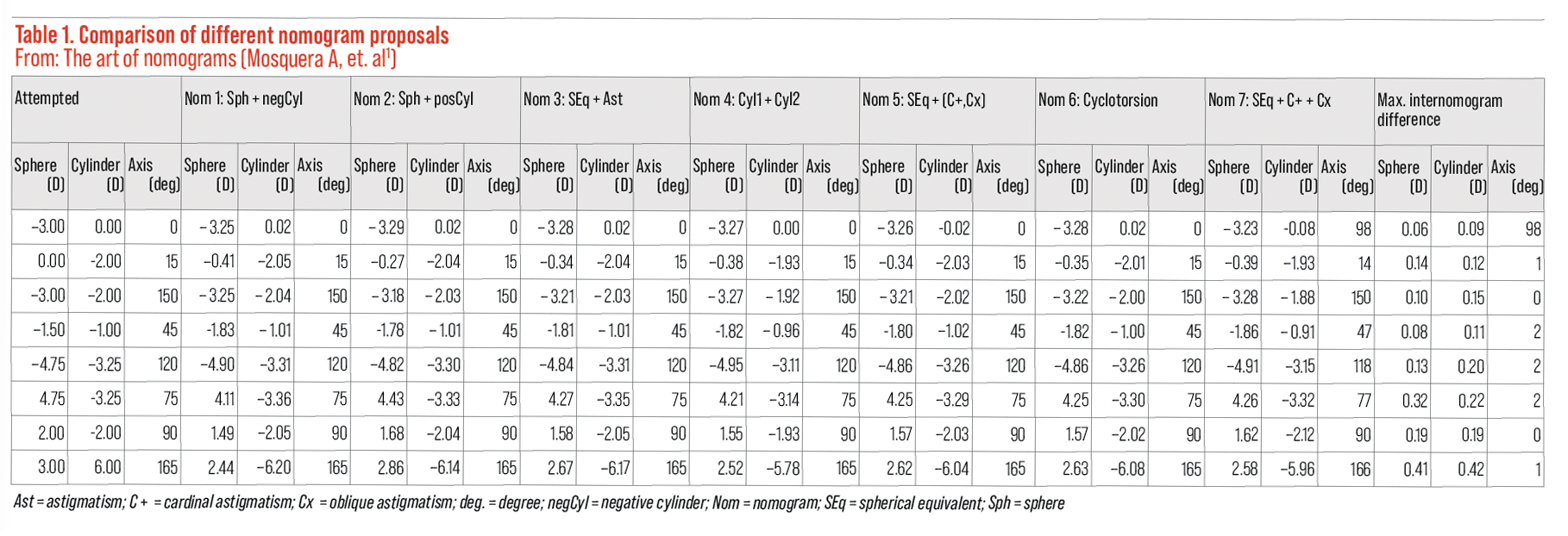 |
| A group of researchers constructed seven nomograms for eyes treated with LASIK for myopic astigmatism and found nomograms 5, 6 and 7 detected significant astigmatic differences. They concluded that their nomograms suggested minor improvements vs. actual observed outcomes. Click image to enlarge. |
All nomograms detected subtle differences in the spherical component (p<0.0001). Nomograms 5 and 7 (using power vectors) and 6 (considering axis shifts) detected significant astigmatic differences (nomogram 5, p<0.001; nomogram 6, p<0.05; nomogram 7, p<0.005 for cardinal astigmatism, p=0.1 for oblique astigmatism). The researchers observed mild clinically relevant differences (~ 0.5 D) in sphere or astigmatism among the nomograms; differences of ~ 0.25 D in the proposals for sphere or cylinder weren’t uncommon, and concluded that all nomograms suggested minor improvements versus actual observed outcomes.
The location of your practice also plays a role in nomograms. “Modern lasers provide excellent results in clinical trials for a wide range of refractive errors, however, surgical technique and operating environment, including ambient humidity, altitude, and other factors can affect outcomes,” says Y. Ralph Chu, MD, of the Chu Vision Institute in Bloomington, Minnesota. “For LASIK and PRK, the excimer laser platform is sensitive to ambient humidity and hydration levels of the stromal bed. Being aware of where the surgical practice is located such as altitude and humidity level is important to consider when looking at a surgical nomogram.
“Whether the surgeon likes to perform an ablation on a dry stromal bed or with slight moisture on the bed is also important when evaluating a nomogram,” he continues. “When using a femtosecond laser to create ablations like in the SMILE procedure, the femtosecond laser is less dependent on the ambient humidity and the environment. While monitoring outcomes is important because each laser has its own specific characteristics, environmental conditions are less of a consideration when looking at nomogram development during the SMILE procedure.”
The other factor to consider when developing a nomogram is the age of the patient. “This is because healing characteristics change as patients age,” says Dr. Chu. “The general consensus is that younger patients may have a slightly higher tendency toward regression of refractive effect as compared to older patients. Younger patients also tend to tolerate residual refractive error because of their accommodative ability. Older patients may prefer a slight undercorrection towards myopia given the need for improved depth of focus for reading. This isn’t surgeon- or laser-dependent; it’s patient-specific variables that come into consideration when developing a nomogram.”
Dr. McIntire says to be cognizant not to over-minus young patients. “It’s easy to do because their accommodation is still intact,” she says. “We can use this to our advantage a little bit when we do our procedure. The nomograms will all account for this; they will often give a slightly more minus treatment to a young person than to an older person who’s lost their ability to accommodate. The reason for this is that the young person is able to accommodate so they’re going to see well and automatically accommodate right through whatever is there, maybe it’s -0.25 or less of residual myopia. Over time, as the epithelium starts to remodel it’ll give the patient a little bit more of a long-lasting effect. We wouldn’t do that in somebody who’s in their 40s or presbyopic because they can’t accommodate and they’re not going to be happy with the answer that their epithelium is going to remodel—they just want to see.
“Also, the 40-year-old has less time to live with that treatment, because most likely in the next 15 to 20 years that person is going to have a lens replacement surgery and their refraction will be addressed by a new procedure,” she continues. “Whereas, an 18-year-old might have 40 years to live with this procedure so we give them a little bit more wiggle room by adding some minus there.”
Dr. Caster also adjusts for age. “For a younger myope I aim to overcorrect them to make them a little hyperopic because, first of all, they’re not going to object to being a little hyperopic, and there’s a tendency to drift towards myopia over the years,” he says. “In an older patient, I’m going to shoot pretty much for plano in the distance eye. In hyperopic patients, I definitely like to leave them plano or just a touch on the hyperopic side because I’ve found that hyperopic patients hate to be nearsighted in a distance eye. You don’t want to overcorrect them—they tend to not like that.”
A retrospective study of 345 myopic LASIK eyes2 treated with a Nidek EC-5000 evaluated the variables that are most likely to contribute to enhancements. It measured the patients’ refractive correction, corneal curvature using an Alcon EH-290 topographer, the patient’s age and Nidek excimer laser ablation optic and transition zone size, and found the most significant variable contributing to enhancements was an optical zone of 6.5 mm with a transition zone of 7.5 mm. The smaller optical zone was associated with a smaller refractive overcorrection after LASIK surgery (mean for 5.5 mm optical zone, +0.71 +/- 0.29 D; mean, for 6.5 mm optical zone, +1.27 +/- 0.50 D, paired t-test p<0.0001). The steeper preoperative corneas had a greater chance of enhancement (mean of sample 44.48 +/- 1.47 D and mean of enhancements 45.30 +/- 1.65 D, p=0.01, independent sample test).
Nomograms also have to account for surgical technique, even on the same laser, says Dr. Miller. “Let’s say there are two surgeons using the same laser,” he says. “Surgeon A lifts the flap and within five seconds is doing the ablation. Surgeon B is a little slower. They lift the flap, admire the beauty of the stromal bed, dry the bed with endless sponges, and overall take 30 seconds before they get around to doing the ablation—so, five seconds versus 30 seconds. After 30 seconds, surgeon B is going to dry out the corneal stromal bed quite a bit, so each pulse of the laser is going to remove more tissue. If both surgeons input -3 D of spherical correction, surgeon B might actually be doing a -4 D correction by the time the cornea is dry. So, that individual’s nomogram on the same laser might have to enter less treatment to achieve the desired result.”
Most nomograms start producing useful feedback after about 30 cases. “But if you do 30 cases but none of them has a high sphere or high cylinder, you might have to accumulate many hundreds of cases before you realize a benefit for these eyes,” Dr. Miller advises.
Shared Nomograms
The surgeons we spoke with say that the nomograms available on laser platforms have improved since the earlier days of LASIK, but they’re not perfect.
“As laser technologies mature, these devices do get better at delivering the corrections we desire, but they’ll never be perfect,” says Dr. Miller. “Some lasers run hotter and take off more tissue per pulse. Some lasers work in environments where the humidity is higher, meaning that as the laser beam travels through the air, moisture in the air steals away some of the energy. The humidity and temperature of the treatment room, altitude, whether patients wear perfume or not—these are things for which laser manufacturers can’t fully compensate.”
Dr. Caster encourages doctors to develop their own surgeon-specific nomogram and compare it to the shared nomograms, but with a bias towards the shared nomograms because they involve a lot more data. “Each type of laser will have its own nomogram that will be different, and each individual laser within a type runs slightly different from each other,” he says. “That’s why a good personal nomogram will be better than the shared nomogram, but the personal nomogram is going to suffer unless you’re really accurate at collecting the postop data and you don’t have too many people lost to follow-up exams because they’re happy.”
Despite the value of personal nomograms, not many refractive surgeons are developing their own personal nomograms because it would be technically difficult to do, according to Dr. Miller. “Most tend to use commercial nomogram services,” he says. “The commercial nomograms give the surgeon access to data from hundreds or thousands of surgeons using the same laser device. This eases the transition to using a new device. The surgeon gets the benefit of everyone’s collective experience with that particular laser. Over time, the surgeon adds data for his or her own site, and the nomogram is improved for their particular use. It should also be remembered that the same laser changes over time. A six-month-old laser is going to run differently than the same laser 10 years later. The optics might get a little dirty; there might be a smudge mark on a mirror somewhere; or the laser cavity may just run colder. Nomograms are designed to keep up with these changes.”
Commercial nomograms are exclusive to the laser platform and to the optical zone size. “The program I use is SurgiVision, created by Guy Kezirian, MD,” says Dr. Caster. “It’s available for Alcon lasers, among others. I think it’s a very good program, but you have to be careful to use it properly. For example, with a higher correction, I use the smaller optical zone. For the lower corrections, I use a larger optical zone. I end up with two different formulas: one for the lower corrections and one for the higher corrections. When the data crosses over, the two nomograms will actually get different results. There’s judgment involved in using this.”
Dr. Caster also performs SMILE procedures and uses the Zeiss Visulyze nomogram service. “With the Zeiss nomogram I was told to start by increasing everything by 10 percent,” he says. “That’s the nomogram that seems to work and that’s what my data has shown. So, my data just confirmed that general rule. It seems a little simpler on the SMILE side with the nomogram.”
Dr. McIntire is also familiar with SurgiVision, as well as IBRA (Internet-based Refractive Analysis), both on the Alcon lasers. “They’re pretty widely used and it’s in the interest of the laser manufacturer that surgeons do a good job with their laser so they provide access to these different nomograms,” she says.
“I haven’t found a discernible difference in my outcomes when I use one versus the other,” continues Dr. McIntire. “If the surgeon has standards set within their clinic, they ought to be able to get reliable outcomes with either one. I think they’re both very robust, and there’s a large amount of data in both of those platforms. The most important thing is that the information that’s going into these algorithms is standardized. Someone might be able to get four or five or maybe more refractions that can get a person seeing 20/20, but if the only guideline in the practice is to enter the refraction that gets the patient seeing 20/20, that doesn’t create a standardized process for data collection. There are better ways to do that.”
Dr. McIntire uses binocular balanced refraction. “Sometimes, patients can see 20/15, sometimes they can see 20/10, in which case 20/20 is quite blurry for them,” she says. “Binocular balance prevents them from being over-minused and gets a very robust, repeatable, accurate refraction that multiple different technicians or physicians could emulate for the same result. There are many methods of using the phoropter and achieving a manifest refraction, and this one takes a little bit more time, but it’s robust, it’s repeatable. That data would be entered into manifest refraction on IBRA or SurgiVision. It’ll ask demographic information and patient name, age, corneal curvature, and give a place to report if there’s any other ocular pathology.
“It will want to know the same preop and postop, so you want to enter refraction and best corrected visual acuity and then you’ll enter what your target is because the target isn’t always plano,” she continues. “Planos can see well in the distance without glasses, but sometimes people want to see up close without correction. All of that helps give the algorithm the information that it needs to tell the surgeon ‘to get this outcome, this is what you need to program into the laser.’ It’s going to be somewhere a little bit more or less than what the refraction is just depending on all of the other variables. If there’s a new surgeon coming in to use one of these platforms, they don’t have any personal historical data to tell them ‘here’s how my laser operates.’ What the program will do instead is create a generalized outcome. It will say, ‘based on all of these hundreds of thousands of procedures that have been done by other surgeons in other places, here’s a good place to start.’ As the surgeon enters more data, it will eventually rely on the surgeon’s own outcomes to tweak their nomogram.”
The next most important step is the postop data. “Again, if technicians are only checking the 20/20 line, that’s not sufficient,” Dr. McIntire says. “Ideally, we’ll be doing another postop binocular balance refraction on everybody a few weeks after surgery and using that for the postop data. Over time with volume, these nomograms will help each surgeon and each laser calibrate the nuances from one machine to another, because they’re not all exactly the same—they’re pretty darn close. So if all you want to achieve is ‘good,’ then they’re pretty close, but if you want ‘excellent,’ and you want repeatable, reliable excellence, then these numbers become really important.”
Artificial intelligence is going to play a bigger role in nomogram development. “I think the future of nomogram development lies in artificial intelligence,” says Dr. Chu. “The ability to gather data across multiple platforms and multiple surgeons in different environments and analyze those variables to provide real-time automated information to guide the treatment is the future of nomogram development. Integrating clinical measurements such as topographical assessment will also be part of the future.”
One study found the AdaBoost machine learning model to perform very well in the prediction of the sphere, cylinder and astigmatism axis nomograms for SMILE with root-mean-square errors of 0.1378, 0.1166, and 5.17 for the sphere, cylinder and astigmatism axis nomograms, respectively.3 In the analysis of 3,034 eyes, the feature with the highest importance was preoperative manifest refraction for all nomograms, and for the sphere and cylinder nomograms specifically, the surgeon was the next most important feature in outcomes.
No matter what software program or personalized nomogram you choose to use, Dr. Caster emphasizes it all comes down to data collection and common sense. “It’s hard to get good data,” he says. “First of all, your happy patients tend to come in less often and they often drop out, therefore your nomogram is going to be biased towards the unhappier patients. You have to spend a lot of time with every refraction that you’re going to use in your nomogram analysis and there has to be effort put into that. In general, you have to use nomogram analyses, but you also have to use common sense when looking at the results. If the nomogram is telling you something that your experience tells you isn’t right, then I would look at my past experience and factor that in.”
Dr. Caster has no disclosures. Dr. Chu is a consultant for Zeiss. Dr. McIntire and Dr. Miller have no disclosures.
1. Arba Mosquera S, de Ortueta D, Verma S. The art of nomograms. Eye and Vision 2018; 5,1-13.
2. Feltham MH, Wolfe RJ. Some variables to consider to avoid the need for LASIK surgical enhancements. Clin Exp Optom 2000;83:2:76-81.
3. Park S, Kim H, Kim L. et al. Artificial intelligence-based nomogram for small-incision lenticule extraction. BioMed Eng OnLine 2021;20:38.