For the past several years, the role of mitomycin C in corneal refractive surgery procedures has been growing. Whether treating a patient with scarring from PRK, or perhaps using the agent during primary surgery as a prophylactic haze-prevention measure, surgeons are now able to improve outcomes in patients undergoing surface ablation. In this article, I'll describe the techniques that researchers here and abroad have developed to make the most effective use of MMC.
Renewed Interest
Despite the prevailing preference for LASIK, PRK remains an important refractive surgery option, especially for patients with thin corneas or large pupils. PRK avoids the potential flap complications associated with LASIK, which have been reported in up to 8 percent of LASIK cases, and may also reduce the incidence of ectasia. Wavefront studies suggest that PRK induces fewer aberrations than LASIK, and the emergence of LASEK has rekindled interest in surface excimer procedures. The question with PRK has always been, and remains, the significant risk for postoperative haze and loss of best corrected visual acuity.
 |
| Mitomycin C's alkylating properties enable it to inhibit DNA synthesis, and this may reduce existing symptomatic haze after PRK. |
Treating Existing Haze
Mitomycin C, an antibiotic/chemotherapeutic agent, has long been used in glaucoma surgery to prevent scarring and resultant bleb failure; in pterygium surgery; and in the treatment of corneal intraepithelial neoplasia. MMC's alkylating properties enable it to inhibit DNA synthesis, and this may reduce existing symptomatic haze after PRK, as demonstrated by several animal studies by Jonathan Talamo and others, as well as in the initial human series that my colleagues and I reported in Ophthalmology in 2000. Several further studies have corroborated the safety and effectiveness of MMC in reducing postop haze following PRK.
Prophylactic Uses of MMC
With the advent of newer-generation lasers, the incidence of postop haze following PRK has decreased, though the risk remains, especially in certain high-risk cases. In recent years, more surgeons are considering the prophylactic use of MMC, and several studies support the efficacy of this approach to PRK.
Certain patients may be at higher risk for developing postoperative haze with surface ablation. In the past, surgeons tended to look at higher attempted dioptric correction as a risk factor, and the conventional wisdom was that ablations of greater than 6 D would be considered a significant risk for the development of haze. The advent of flying-spot lasers and the ability to expand the treatment zone have made this guideline obsolete.
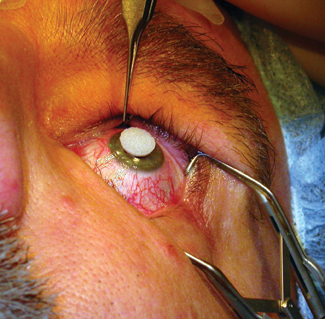 |
| After laser treatment, the sponge is placed on the central cornea, taking care to monitor the surface to avoid contact of the MMC with the limbus or conjunctiva. |
I prefer to think in terms of the total energy that's delivered to the cornea in the laser treatment as the variable most closely related to the development of haze. The total energy is directly correlated with the overall depth of ablation. A -4 D treatment with a small optical zone may remove a relatively small amount of tissue, but a -4 D treatment using a 7-mm optical zone may remove 100 µm of tissue. In our practice, we have developed a protocol that considers greater than 75 µm of tissue ablation to represent a risk for scarring or haze, and we will use MMC prophylactically in those cases.
Our initial unmatched case series of prophylactic MMC with PRK included 40 eyes of patients who underwent PRK and 34 who underwent LASEK. All had greater than -6 D spherical equivalent or insufficient corneal thickness for LASIK. In this study, just five patients (6.7 percent) developed haze which was visually insignificant (mean haze score 0.07 on a 0-4 scale).
An Italian study provided further support for MMC prophylaxis. The prospective, randomized study at the Carones Ophthalmology Center, Milan, included 60 eyes (60 patients) with a spherical equivalent correction between -6 and -10 D. After PRK, the study group eyes were treated with MMC 0.02% for two minutes. The control eyes did not receive this treatment. No eye in the treatment group had greater than 1 rating for haze during six months of follow-up, while 19 eyes (63 percent) in the control group did. Also at six months, 26 study group eyes (87 percent) and 14 control eyes (47 percent) were within ±0.50 D of the attempted correction. No study group eye had a BCVA loss during the follow-up, while seven control eyes had lost one to three lines at six months.
This same group presented a study at last year's American Society of Cataract & Refractive Surgery meeting that compared the same PRK/MMC treatment protocol to LASIK in patients with at least -6 D of myopia. At six months, 70 percent of the PRK group had a SE refractive error of ±0.50 D (and 95.7 percent, ±1.0 D) compared to 74.4 percent at ±0.50 D in the LASIK group (and 88 percent, ±1.0 D).
Preop Considerations
Informed consent with such patients must include a discussion of the risk of postoperative haze, either with or without MMC. Though we haven't had any cases of postop haze develop since we started using our protocol, it's important that patients understand that the possibility of developing haze despite MMC remains.
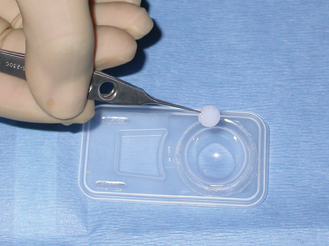 |
| A corneal light shield, a 6-8 mm circular Merocel sponge, is placed in the MMC solution. The shield gives more concentrated coverage than application by a Merocel spear. |
Though minimal, the use of MMC also carries the potential for toxicity and this should be discussed thoroughly. Surgeons can minimize this risk by assuring the accuracy of the formulation, the proper duration of exposure and careful attention to technique during the procedure.
In preoperative planning for the laser treatment, keep in mind that in terms of refractive outcomes, the use of MMC tends toward hyperopic over-response. This is most likely due to the inhibition of the compensatory wound healing that occurs after the laser treatment, which normally results in a reversal of any hyperopic shift in the early phase. I usually reduce my programmed spherical refraction 10 to 15 percent, depending on the patient's age and refractive error.
The Technique
Our protocol relies on an independent compounding pharmacy to assure the correct dilution of 0.02% (0.2 mg/mL) MMC. Though I'm aware of very few instances of MMC toxicity-associated complications among surgeons using this technique, those that have occurred tend to be related to incorrect compounding. We receive the MMC in 1-mL syringes, which can be frozen for up to a month and used as needed.
Before the surgery, the MMC is thawed and placed in a disposable contact lens vial. A corneal light shield, a 6-8 mm circular Merocel sponge, is placed in the MMC solution. After the laser treatment, I place the sponge, wet but not dripping, on the central cornea and leave it in place, taking care to monitor the surface to avoid contact of the MMC with the limbus or conjunctiva. The light shield tends to concentrate the MMC onto the central cornea and prevents it from spilling out onto the limbus, unlike a Merocel spear.
We initially used a two-minute duration of application, which was consistent with animal studies and our own early experience in treating pre-existing PRK haze. More recently, in an attempt to further reduce the potential for toxicity, shorter application times have been used. We are presently studying the efficacy of a 12-second and 60-second application. Though we have just six-month's follow-up on these cases, no eyes have developed postop haze.
Vigorous irrigation of the cornea post-exposure with approximately 30 cc of BSS is the final key to avoiding toxicity. Irrigate the surface, the fornices and the limbus to assure that no residual MMC is in contact with any of these structures. Despite earlier concerns that MMC would inhibit regrowth of epithelial cells, our experience has shown no delay in reepithelialization as long as there is no intraoperative contact of MMC with the stem cells at the limbus.
Postoperatively, the standard regimen for PRK cases applies, including steroid, antibiotic and a bandage contact lens. Once reepithelialization occurs, I usually will stop the antibiotics after a week, taper the steroids over one to two months, and watch the patient's progress.
Treating Flap Complications
LASIK flap complications such as buttonholed or partial flaps present a treatment dilemma. Waiting for a partial flap to heal may leave the patient to face several months of anisometropia and anxiety. In addition, a second microkeratome pass over a healed buttonhole is not without risks, including a second buttonhole, particularly when the cause of the initial buttonhole is unknown. Based on the successful use of MMC to treat haze after PRK, my colleagues and I decided to test the theory that PRK with adjunctive use of MMC to prevent corneal haze might be a better option than a second attempt at LASIK in these cases.
The technique can also be in combination with PTK for buttonholed flaps that develop fibrosis or scarring. In a recent study (in press), we evaluated transepithelial phototherapeutic keratectomy/photorefractive keratectomy (PTK/PRK) with prophylactic MMC following flap complications in LASIK.
The study looked at 10 eyes of 10 patients who sustained LASIK flap complications and underwent transepithelial PTK/PRK for correction of ametropia. The mean preoperative UCVA was 20/400 (range 20/40-counting fingers), mean preoperative BSCVA was 20/28.5, and spherical equivalent of refractive errors ranged from +4 to -10.75 D. Following laser ablation, we applied MMC 0.02% to the stroma for two minutes. After the procedure, the mean UCVA was 20/28, the mean BSCVA was 20/21 and spherical equivalent refractive errors ranged from +0.375 to -1 D. The mean follow up time ranged from eight to 28 months. No patients experienced delayed re-epithelialization, haze or other signs of toxicity.
Another group recently reported successful use of PRK with MMC to manage a LASIK flap complication after penetrating keratoplasty. The patient developed a buttonhole secondary to an attempted LASIK in an eye that had undergone prior PKP for keratoconus. Three months after the PRK/MMC procedure, the patient demonstrated a clear cornea and a BCVA of 20/20.
The keys to success with MMC include proper patient selection, a thorough informed consent discussion, and meticulous attention to the established protocol. I am confident that MMC will soon change our thinking about surface ablation in high-risk cases.
Dr. Majmudar is an assistant professor of ophthalmology at Rush University Medical Center and practices at Chicago Cornea Consultants, Ltd. Contact him at pamajmudar@chicagocornea.com, or (847) 882-5900, and (847) 882-6028 (fax).

1. Vigo L, Scandola E, Carones F. Scraping and Mitomycin C to Treat Haze and Regression After Photorefractive Keratectomy for Myopia. J of Refractive Surgery 2003;19:449-454.
2. Solomon R, Donnenfeld ED, Perry HD. Photorefractive keratectomy with mitomycin C for the management of a LASIK flap complication following a penetrating keratoplasty. Cornea. 2004;23(4):403-5.
3. Majmudar PA, Forstot SL, Nirankari VS, Dennis RF, Brenart R, Epstein RJ: Topical Mitomycin-C for Subepithelial Fibrosis after Refractive Corneal Surgery. Ophthalmol 2000; 107:89-94.
4. Lane HA, Swale J, Majmudar PA. Prophylactic Use of Mitomycin-C in the Management of Buttonholed LASIK Flaps. J Cataract Refract Surg 2003;29:390-392.
5. Muller LT, Candal EM, Epstein RJ, Dennis RF, Majmudar PA. Transepithelial phototherapeutic keratectomy/photorefractive keratectomy (PTK/PRK) with Adjunctive Mitomycin-C for Complicated LASIK Flaps, In Press for J of Cataract and Refractive Surgery.
6. Majmudar PA, The Role of MMC in Corneal Refractive Surgery, Techniques in Ophthalmology, Vol. 2, No. 2, June 2004, 43-9.



