 |
|
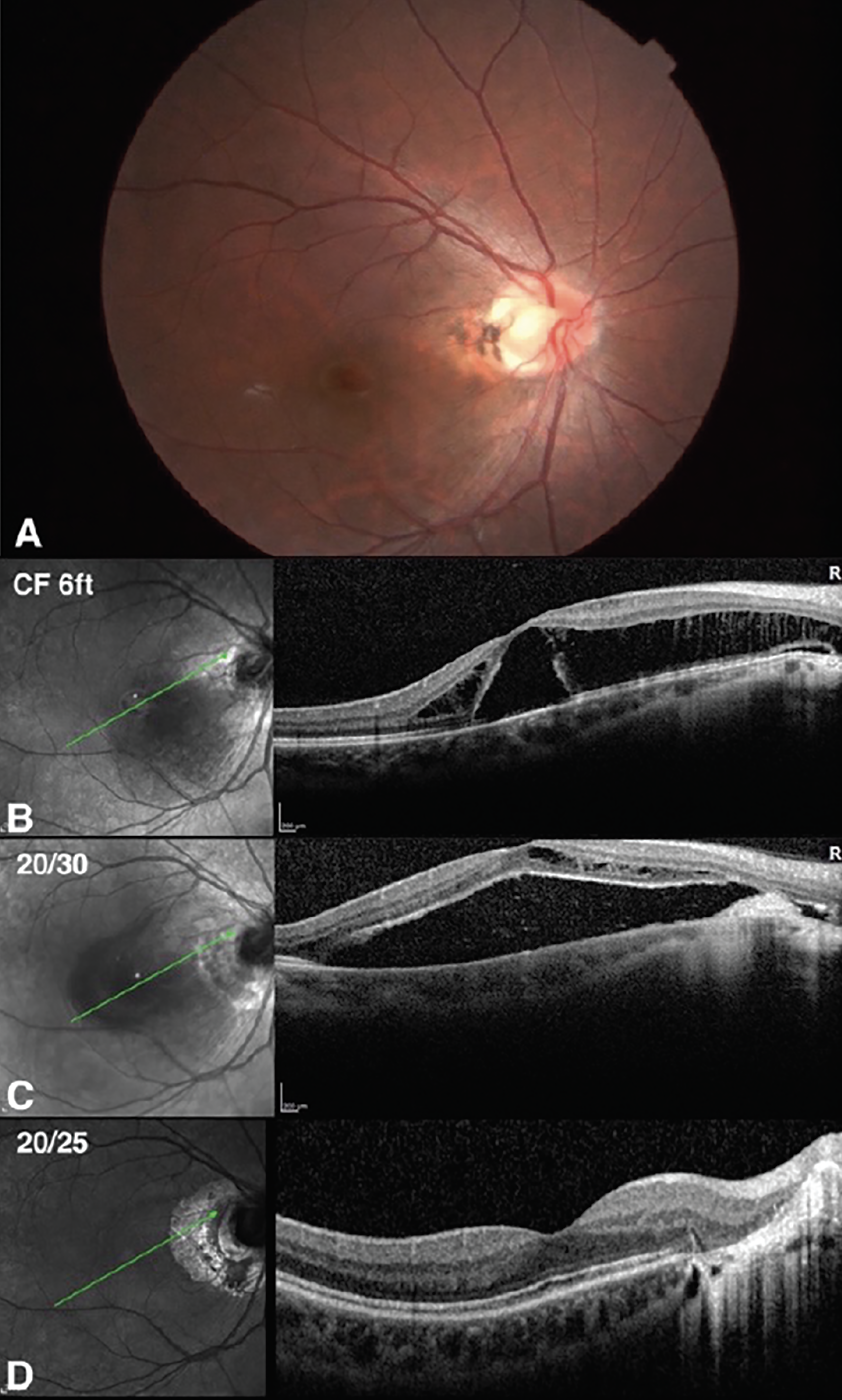
Figure 1. A 36-year-old female with optic disc pit maculopathy OD. Vision was CF 6ft. On presentation (A, B), she underwent focal barrier laser twice, with improvement in vision to 20/30 six months later, however, an increase in subretinal fluid was seen (C). The decision was made to proceed with vitrectomy and SF6 gas tamponade. Vision improved to 20/25 and remained stable (D). |
Optic disc pits are congenital unilateral excavations of the optic nerve head that may be associated with other abnormalities of the optic nerve and peripapillary retina.1 Their occurrence is typically sporadic, estimated at one in 10,000 individuals.1 In cases where the optic pit is asymptomatic, patients are advised to undergo regular follow-up appointments and comprehensive eye examinations, including dilated retinal evaluations.2 This is crucial, as 25 to 75 percent of cases may develop complications such as associated maculopathy, characterized by retinoschisis-like changes and serous macular detachment.2
Given the rarity of optic disc pit maculopathy, however, a definitive consensus on the optimal treatment approach remains elusive. A wide variety of treatment strategies have been described; however, most reports involve a small number of cases with limited long-term follow-up. In this discussion, we’ll explore the treatment options available.
Etiology
It’s been proposed that optic disc pit maculopathy begins with splitting within the inner retinal layers, similar to macular schisis, and progresses to serous macular detachment following the formation of a hole in the outer retinal layers. This hole allows fluid from within the retina to pass into the subretinal space.3 Both male and females are equally affected, and maculopathy typically emerges in the third or fourth decades of life, but can affect children also.1 Patients are encouraged to be aware of the signs and symptoms of maculopathy, such as metamorphopsia, dullness of colors, visual field defects and decreased vision (visual acuity ranges between 20/25 to counting fingers, depending on the extent and duration of maculopathy).4 They’re advised to perform home visual acuity assessments and Amsler grid testing to monitor for potential onset of maculopathy.5
Previously, it was advised to allow up to three months for spontaneous resolution before considering surgical options.6 Spontaneous improvement of optic pit maculopathy, usually following posterior vitreous detachment, can occur in up to a quarter of cases, with potential for visual improvement.2 Complete spontaneous resolution is rare—although fluctuations in the fluid are common, since the fluid is thought to be connected to the cerebral spinal fluid and vitreous. Visual outcomes can be poor, especially when the detachment is chronic, potentially resulting in permanent vision loss.2,7 Full-thickness macular holes can lead to irreversible visual impairment, and cystic changes in the foveola and degenerative alterations in the retinal pigment epithelium may also be observed.3 The integrity of the outer retinal structures is correlated with final visual acuity, making OCT a valuable tool for assessing visual prognosis and the possible need for surgical intervention.7 Other reports have indicated that the ultimate visual acuity is primarily influenced by the presenting visual acuity.8 Currently, however, waiting too long without action is generally not recommended, especially if there’s evidence of increasing fluid accumulation or deterioration in vision.2,9
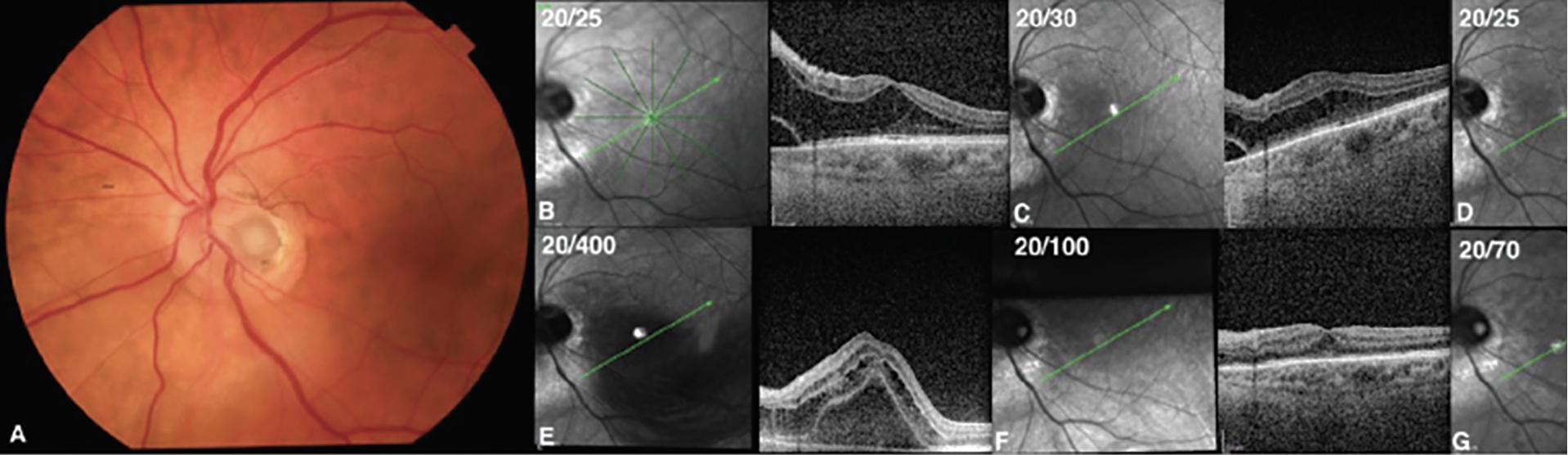 |
| Figure 2. A patient with optic pit maculopathy (A and B: baseline visit) who initially underwent a 25-gauge pars plana vitrectomy, internal limiting membrane peeling and flap technique, endolaser photocoagulation and SF6 gas tamponade. Despite these interventions, the patient’s maculopathy and visual acuity worsened over time (C: postoperative month 1, D: postoperative month 3, E: postoperative month 4). Consequently, the decision was made to perform a second surgery, utilizing scleral plugging using a scleral patch graft (Figure 3). In this surgery, additional internal limiting membrane was mobilized. Scleral patch graft was sized, cut and placed within the optic pit. The residual internal limiting membrane flap was then placed over the scleral plug. This combination of treatments led to a significant improvement in the patient’s maculopathy (F: postoperative month one, G: postoperative month two). |
The Options Explained
The retinal surgeon has several options for these cases:
• Laser photocoagulation. Laser, applied at the margin of the temporal disc, leads to the formation of a chorioretinal scar that’s thought to act as a barrier to prevent fluid from the optic disc pit from continuing to enter the subretinal space.10 This method involves creating one or several rows of laser burns, aiming for very light burns while minimizing collateral damage to the nerve fiber layer.1 However, the outcomes of laser treatment have been inconsistent, with an unpredictable—and often long—duration until improvement.2,10 Additionally, laser over the maculopapular bundle can cause blind-spot enlargement, leading to significant visual field defects. As a result, this method, particularly when used as a standalone treatment, has declined in popularity.
• Intravitreal gas injection. Injection of intravitreal gas can lead to the formation of a posterior vitreous detachment while simultaneously sealing the optic pit, leading to the reattachment of the macula.11 However, the success rate for achieving macular reattachment with this technique alone stands at 50 percent, and multiple injections are often required.11 Combining laser photocoagulation with intravitreal gas injections, on the other hand, has shown potentially more promising results. In one small patient series undergoing this combined treatment approach, there was reported improvement in vision and reduction of fluid in all treated eyes, with a complete resolution of intraretinal and subretinal fluids observed in 75 percent of cases.12
• Macular buckling surgery. This technique involves attaching a buckling element to the sclera along the 6-to-12 o’clock meridian, inducing a buckling effect beneath the macula.13 Scleral buckling adjusts the direction of posterior hyaloid traction from anterior to posterior, facilitating the reattachment of the macula.1 Reports indicate that this approach leads to complete fluid resolution in approximately 85 percent of cases, alongside notable enhancements in visual acuity and visual field.14,15
Longitudinal studies, tracking patients who underwent this surgery, have shown that buckling’s effectiveness persists for more than 10 years, with minimal complications or recurrences and sustained improvements in vision. Furthermore, OCT imaging has confirmed the restoration of the foveal outer retinal layer structure.16 While these outcomes are promising, it’s important to acknowledge that the surgery requires specialized skills and equipment, including the use of intraoperative B-scan for precise placement of the macular buckle, leading to a limited adoption of this method.2 Despite being introduced 20 years ago, the technique hasn’t become popular, with all published outcomes originating from the same research group.13,17
• Vitrectomy. Recently, the role of vitreous traction has gained recognition as a significant element in the development of optic disc pit maculopathy, leading to pars plana vitrectomy being widely adopted as the main treatment strategy, either alone or in combination with other techniques.18,19 Induction of a complete posterior vitreous detachment to remove vitreous traction on the optic pit is thought to be a critical step for macular reattachment. However, additional surgical interventions such as laser photocoagulation, gas tamponade, internal drainage and peeling of the internal limiting membrane over the macula continue to be debated. Successful outcomes have been documented using different combinations of these techniques. Time to complete macular reattachment following vitrectomy can be variable and take up to a year to achieve.20
• Endolaser. This approach carries the same risk of laser scar enlargement and visual field defect and should be approached with caution if performed. Gas tamponade has been suggested to help seal the optic pit and displace the subretinal fluid.18,19 Endodrainage of the subretinal fluid or intraretinal fluid from within the schitic cavities using an intraretinal cannula with or without active aspiration has been also proposed.17,21 Internal limiting membrane peeling can help to completely eliminate any tangential traction, however the presence of extremely thin internal retinal layers and schisis cavities may increase the risk of iatrogenic macular hole formation during attempts to peel the internal limiting membrane.22 The value of adding internal limiting membrane peeling to the standard surgical procedure to enhance surgical and functional outcomes is subject to debate, as good results without internal limiting membrane peeling have also been reported.3
• Covering/plugging the pit. Other surgical techniques include directly covering or plugging the optic disc pit with an internal limiting membrane flap or plug, autologous scleral tissue flap or plug, autologous fibrin from the patient’s own blood, fibrin glue or human amniotic membrane.23-27 Covering the optic disc pit is thought to prevent fluid from leaking into the subretinal space through the pit, yet it doesn’t necessarily halt cerebrospinal fluid from infiltrating this space. Plugging the pit with a suitable material is thought to block both potential fluid sources from entering the subretinal area. Risk factors associated with unfavorable surgical outcomes include eyes with fluid present in multiple layers, subretinal fluid that extends beyond the vascular arcades and increased central foveal thickness.23
A technique involving the use of an autologous inverted internal limiting membrane flap has been shown to effectively prevent fluid from the vitreous from reaching the subretinal space. This method involves staining and peeling the internal limiting membrane within the temporal arcades while leaving a section near the optic disc edge attached, creating a pedicle-like structure.28 A small internal limiting membrane flap is sufficient to cover the pit.29 This approach can lead to quick absorption of subretinal fluid, potentially resulting in early macular reattachment and improvement in visual acuity.28
Peeling of the internal limiting membrane flap from the temporal side of the disc and inserting it into the pit with a diamond-dusted membrane scraper is another technique that has been reported. This approach has been applied in cases of chronic or refractory optic disc pit maculopathy, where the pit was sealed with either a relocated or grafted internal limiting membrane flap combined with gas tamponade.30 An anatomical success rate of 55.6 percent was observed after an average follow-up period of 10 months, with a mean time to reattachment of 6.5 months, and an average improvement in best-corrected visual acuity of three lines.30 In one comparative case series, filling the optic pit with the internal limiting membrane led to faster fluid resolution compared to merely peeling the internal limiting membrane alone.31 Nonetheless, both the anatomical and visual outcomes between the two methods were comparable.31
Autologous scleral flaps can be used to plug the optic pit. In one series, this technique led to successful anatomical results in two of two eyes with prior failed vitrectomy with internal limiting membrane peel, and 17 of 18 eyes not previously treated.23,32 The addition of the scleral plug is hypothesized to lead to a quicker resolution of subretinal fluid (mean of 4.5 months versus mean of 12 months) and achieves normal central foveal thickness.32 Similar results have been achieved with a scleral plugs compared to inverted internal limiting membrane flap plug, (85.7 versus 87.5 percent one-year anatomical success, respectively) while ILM peeling alone resulted in suboptimal outcomes in comparison (25 percent one-year anatomical success).23
Figure 2 illustrates the case, courtesy of Sunir Garg, MD, of Mid Atlantic Retina at Wills Eye Hospital, of a patient with optic pit maculopathy.
Use of autologous platelet-rich plasma layered over the pit followed by long-acting gas tamponade and face-down positioning was described in a patient with failed prior vitrectomy and endolaser therapy.33 Subretinal fluid resolution was observed along with significant visual improvement from 20/100 on presentation to 20/50 eight months later.33 In two reported cases of failed vitrectomy with internal limiting membrane peeling, the authors used autologous fibrin glue to seal the persistent pits.24 This procedure was successful in achieving retinal reattachment at the final visit at one year in one patient. Final visual acuity was 20/50 from 20/400 on presentation. In the second patient, at two years, final visual acuity was 20/200, stable from preoperative.24
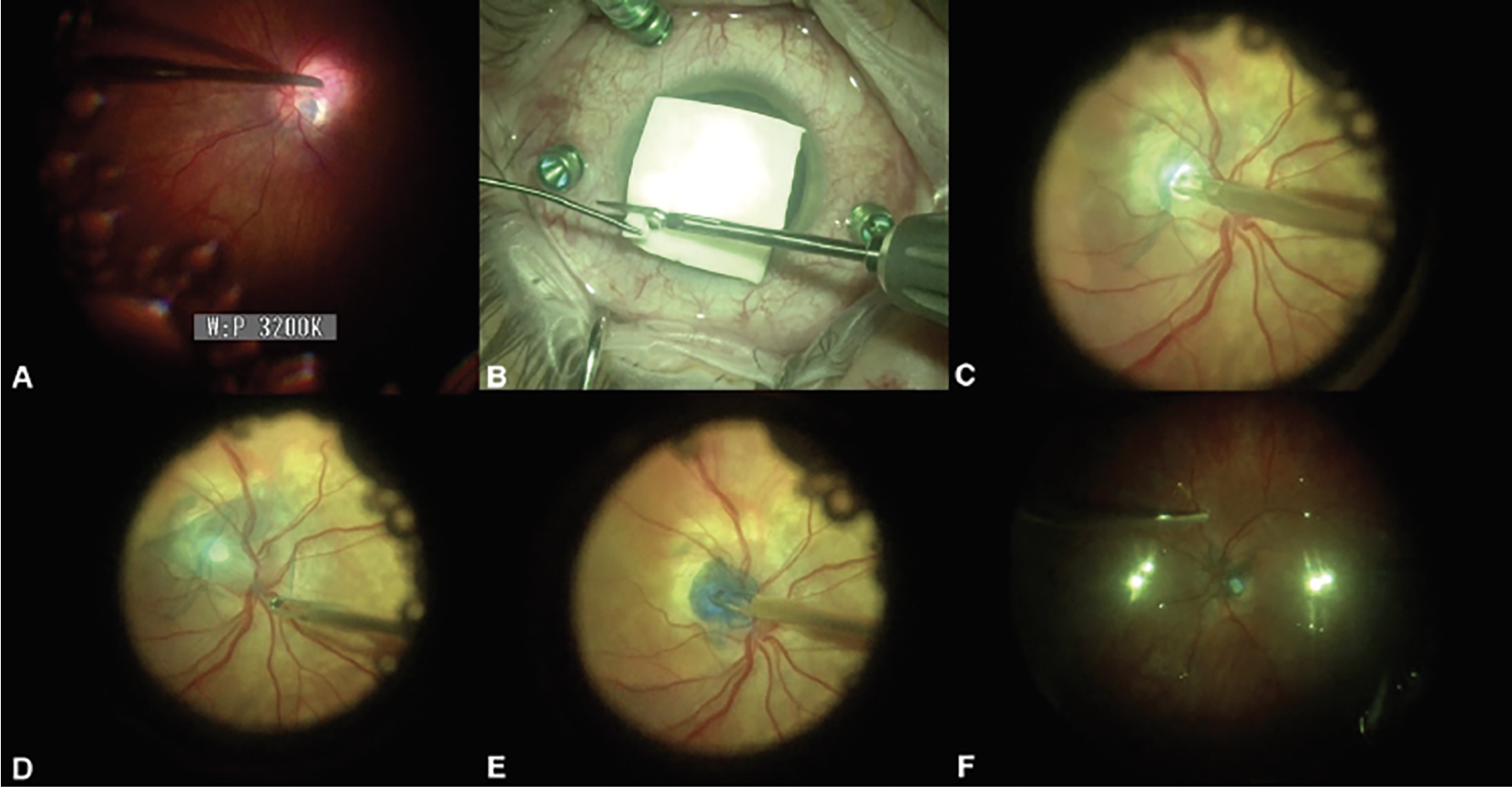 |
| Figure 3. This patient underwent 25-gauge pars plana vitrectomy with endolaser photocoagulation around the pit (A), placement of scleral patch graft plug (B and C), a Brilliant Blue-assisted internal limiting membrane flap (D) and plugging (E), and C3F8 gas tamponade (F). |
Human amniotic membrane patch can also be used to plug the optic pit.26 In a recent prospective study, 11 eyes of 11 patients underwent 25-gauge pars plana vitrectomy with placement of a human amniotic membrane patch into the optic disc pit, followed by air tamponade.26 At one-year follow-up, mean visual acuity improved from 20/80 to 20/30 in nine of 11 eyes (82 percent) with complete subretinal and intraretinal fluid resorption and no reported recurrences or complications.26 However, longer follow-up and close observation is needed, as one report described a case of human amniotic membrane-plugged optic disc pit that was successful at one year postoperatively with 20/60 vision, however six months later showed recurrence of intraretinal fluid with decline in visual acuity to 20/160.27
A combination of intravitreal fibrin glue and internal limiting membrane abrasion has been proposed to treat optic disc pit maculopathy.25 Internal limiting membrane abrasion is performed as an alternative to internal limiting membrane peeling that aims to reduce damage to subjacent structures. This is followed by the introduction of intravitreal fibrin glue (Tisseel) to seal the optic pit, and gas-air exchange.25 This technique has been done in only three eyes and only the three months postoperative outcomes have been reported. The long term visual and anatomical outcomes are still unknown.
In summary, diverse surgical techniques have been explored for addressing optic disc pit maculopathy. The choice of technique often hinges on the surgeon’s preferences and expertise, alongside the accessibility of medical and surgical materials and equipment. It’s crucial to note that while the majority of surgical techniques have been used to attain the intended anatomical and functional results, these improvements typically take several months to attain during the postoperative period. Complete resolution may take up to six to 12 months, and the timeframe is contingent upon the specific surgical technique employed.23 In instances of refractory cases, re-operation remains a viable option, and successful outcomes following re-operation have been reported.
Dr. Momenai and Dr. Mansour are research fellows at Wills Eye Hospital in Philadelphia.
Dr. Sivalingam is in practice at Mid Atlantic Retina/Wills Eye Hospital.
Dr. Regillo is the director of the Retina Service of Wills Eye Hospital, a professor of ophthalmology at Thomas Jefferson University School of Medicine and the principle investigator for numerous major international clinical trials.
Dr. Yonekawa is an assistant professor of ophthalmology at Sidney Kimmel Medical College at Thomas Jefferson University. He serves on the Education Committee of the American Society of Retina Specialists and on the Executive Committee for the Vit Buckle Society, where he is also the vice president for academic programming.
1. Ravi S, Singh J. Diagnosis and management of congenital optic pit. https://www.aao.org/eyenet/article/diagnosis-management-of-congenital-optic-pit. Accessed February 2024.
2. Moisseiev E, Moisseiev J, Loewenstein A. Optic disc pit maculopathy: When and how to treat? A review of the pathogenesis and treatment options. International journal of retina and vitreous 2015;1:1-9.
3. Avci R, Yilmaz S, Inan U, et al. Long-term outcomes of pars plana vitrectomy without internal limiting membrane peeling for optic disc pit maculopathy. Eye 2013;27:12:1359-1367.
4. Anglo M. Topical review: Optic disc pits and associated maculopathy. Optometry and Vision Science 2020;97:7:531-535.
5. Brown GC, Shields JA, Goldberg RE. Congenital pits of the optic nerve head: II. Clinical studies in humans. Ophthalmology 1980;87:1:51-65.
6. Georgalas I, Ladas I, Georgopoulos G, Petrou P. Optic disc pit: A review. Graefe’s Archive for Clinical and Experimental Ophthalmology 2011;249:1113-1122.
7. Parikakis EA, Chatziralli IP, Peponis VG, et al. Spontaneous resolution oflong-standing macular detachment due to optic disc pit with significant visual improvement. Case Reports in Ophthalmology 2014;5:1:104-110.
8. Sugar HS. Congenital pits in the optic disc and their equivalents (congenital colobomas and colobomalike excavations) associated by submacular fluid. American Journal of Ophthalmology 1967;63:2:298-307.
9. Shah SD, Yee KK, Fortun JA, Albini T. Optic disc pit maculopathy: A review and update on imaging and treatment. International ophthalmology clinics 2014;54:2:61-78.
10. Mustonen E, Varonen T. Congenital pit of the optic nerve head associated with serous detachment of the macula. Acta Ophthalmologica 1972;50:5:689-698.
11. Akiyama H, Shimoda Y, Fukuchi M, et al. Intravitreal gas injection without vitrectomy for macular detachment associated with an optic disk pit. Retina 2014;34:2:222-227.
12. Lei L, Li T, Ding X, et al. Gas tamponade combined with laser photocoagulation therapy for congenital optic disc pit maculopathy. Eye 2015;29:1:106-114.
13. Theodossiadis GP, Theodossiadis PG. The macular buckling technique in the treatment of optic disk pit maculopathy. Semin Ophthalmol 2000;15:2:108-15.
14. Georgopoulos GT, Theodossiadis PG, Kollia A-CK, Vergados J, Patsea EE, Theodossiadis GP. Visual field improvement after treatment of optic disk pit maculopathy with the macular buckling procedure. Retina 1999;19:5:370-377.
15. Theodossiadis GP, Theodossiadis PG. Optical coherence tomography in optic disk pit maculopathy treated by the macular buckling procedure. American Journal of Ophthalmology 2001;132:2:184-190.
16. Theodossiadis GP, Grigoropoulos VG, Liarakos VS, Rouvas A, Emfietzoglou I, Theodossiadis PG. Restoration of the photoreceptor layer and improvement of visual acuity in successfully treated optic disc pit maculopathy: A long follow-up study by optical coherence tomography. Graefe’s Archive for Clinical and Experimental Ophthalmology 2012;250:971-979.
17. Theodossiadis GP, Chatziralli IP, Theodossiadis PG. Macular buckling in optic disc pit maculopathy in association with the origin of macular elevation: 13-year mean postoperative results. European Journal of Ophthalmology 2015;25:3:241-248.
18. Travassos AS, Regadas I, Alfaiate M, Silva ED, Proença R, Travassos A. Optic pit: Novel surgical management of complicated cases. Retina 2013;33:8:1708-1714.
19. Rizzo S, Belting C, Genovesi-Ebert F, et al. Optic disc pit maculopathy: The value of small-gauge vitrectomy, peeling, laser treatment, and gas tamponade. European journal of ophthalmology 2012;22:4:620-625.
20. Hirakata A, Okada AA, Hida T. Long-term results of vitrectomy without laser treatment for macular detachment associated with an optic disc pit. Ophthalmology 2005;112:8:1430-1435.
21. El Rayes EN, Habib AM, Soliman AH, Ibrahim OM, El Sawwah KM. Novel technique for treatment of foveoschisis associated with optic disk pits: Active aspiration of intraretinal fluid. Retina 2022;42:7:1406-1410.
22. Shukla D, Kalliath J, Tandon M, Vijayakumar B. Vitrectomy for optic disk pit with macular schisis and outer retinal dehiscence. Retina 2012;32:7:1337-1342.
23. Babu N, Kohli P, Ramasamy K. Comparison of various surgical techniques for optic disc pit maculopathy: Vitrectomy with internal limiting membrane (ILM) peeling alone versus inverted ILM flap ‘plug’versus autologous scleral ‘plug’. British Journal of Ophthalmology 2020;104:11:1567-1573.
24. Ozdek S, Ozdemir HB. A new technique with autologous fibrin for the treatment of persistent optic pit maculopathy. Retinal Cases and Brief Reports 2017;11:1:75-78.
25. Almeida DR, Chin EK, Arjmand P, Velez G, Evans LP, Mahajan VB. Fibrin glue and internal limiting membrane abrasion for optic disc pit maculopathy. Ophthalmic Surgery, Lasers and Imaging Retina 2018;49:12:e271-e277.
26. Caporossi T, D’Amico G, Tartaro R, et al. Optic disk pit maculopathy treatment using a human amniotic membrane patch: One-year results. American Journal of Ophthalmology 2022;240:30-36.
27. Vaiano AS, Greco A. Optic disc pit treated with human amniotic membrane: Is it a lasting solution? Acta Scientific Ophthalmology 2022;5:5:71-73.
28. Mohammed OA, Pai A. Inverted autologous internal limiting membrane for management of optic disc pit with macular detachment. Middle East African Journal of Ophthalmology 2013;20:4:357.
29. Hara R, Tsukahara Y, Simoyama T, Mori S. Refined internal limiting membrane inverted flap technique for intractable macular detachment with optic disc pit. Case Reports in Ophthalmology 2017;8:1:208-213.
30. Pastor-Idoate S, Gómez-Resa M, Karam S, et al. Efficacy of internal limiting membrane flap techniques with vitrectomy for macular detachment associated with an optic disc pit. Ophthalmologica 2019;242:1:38-48.
31. Ravani R, Kumar A, Karthikeya R, et al. Comparison of inverted ILM-stuffing technique and ILM peeling alone for optic disc pit-associated maculopathy: Long-term results. Ophthalmic Surgery, Lasers and Imaging Retina 2018;49:12:e226-e232.
32. Khatri A, Shrestha SM, Prasai G, et al. Minimally invasive procedure for optic disc pit maculopathy: Vitrectomy with scleral plug and analysis on pattern of resolution. Scientific Reports 2023;13:1:15724.
33. Todorich B, Sharma S, Vajzovic L. Successful repair of recurrent optic disk pit maculopathy with autologous platelet rich plasma: Report of a surgical technique. Retinal Cases and Brief Reports 2017;11:1:15-17.



