Researchers evaluated risk factors for intraocular pressure spikes in glaucomatous eyes following cataract surgery using the IRIS Registry, as part of a retrospective clinical cohort study.
Adults with IRIS Registry data who underwent standalone phacoemulsification between January 1, 2013, and September 30, 2019, were included.
An IOP spike was defined as a postoperative IOP >30 mmHg and >10 mmHg from baseline within the first postoperative week. Odds ratios for demographic and clinical characteristics were calculated with univariate and multivariate logistic regression analyses. Main outcome measures included incidence and OR of IOP spike.
Researchers analyzed data from 1,191,034 eyes (mean age: 71.3 years; 61.2 percent females, 24.8 percent with glaucoma). Here are some of the findings:
• An IOP spike occurred in 3.7 percent of all eyes, 5.2 percent of eyes with glaucoma and 3.2 percent of eyes without glaucoma (p<0.0001).
• Multivariable analyses of all eyes indicated a greater risk of IOP spike with:
– higher baseline IOP (OR, 1.57 per 3 mmHg);
– male sex (OR, 1.79);
– glaucoma (OR, 1.19);
– black race (OR, 1.39 compared to Asian; OR, 1.21 compared to Hispanic);
– older age (OR, 1.07 per 10 years) and complex surgery coding (OR, 1.22; (all p<0.0001).
• Diabetes (OR, 0.90) and aphakia after surgery (OR, 0.60) appeared to be protective against IOP spikes (both p<0.0001).
• Compared to glaucoma suspects, a greater risk of IOP spike was reported, with:
– ocular hypertension (OR, 1.55);
– pigmentary glaucoma (OR, 1.56); and
– pseudoexfoliative glaucoma (OR, 1.52).
• Compared to glaucoma suspects, less risk of IOP spike was reported, with:
– normal-tension glaucoma (OR, 0.55), primary angle closure (PAC suspects (OR, 0.67) and PAC glaucoma (OR, 0.81; all p<0.0001).
• More baseline glaucoma medications were associated with IOP spikes (OR, 1.18 per medicine) while topical beta-blocker use (OR, 0.68) was protective (both p<0.0001).
Researchers reported that higher baseline IOP, male sex, glaucoma, black race, older age and complex cataract coding were associated with an early postoperative IOP spike, while diabetes and postoperative aphakia were protective against a spike following standalone phacoemulsification. They added that glaucomatous eyes demonstrated different risk profiles dependent on glaucoma subtype and that the findings may help surgeons stratify and mitigate the risk of IOP spike after cataract surgery.
Ophthalmology 2024; Jan 19. [Epub ahead of print]
Lidder AK, Vanner EA, Chang TC, et al.
Possible Predictor of Visual Prognosis in Refractory AMD
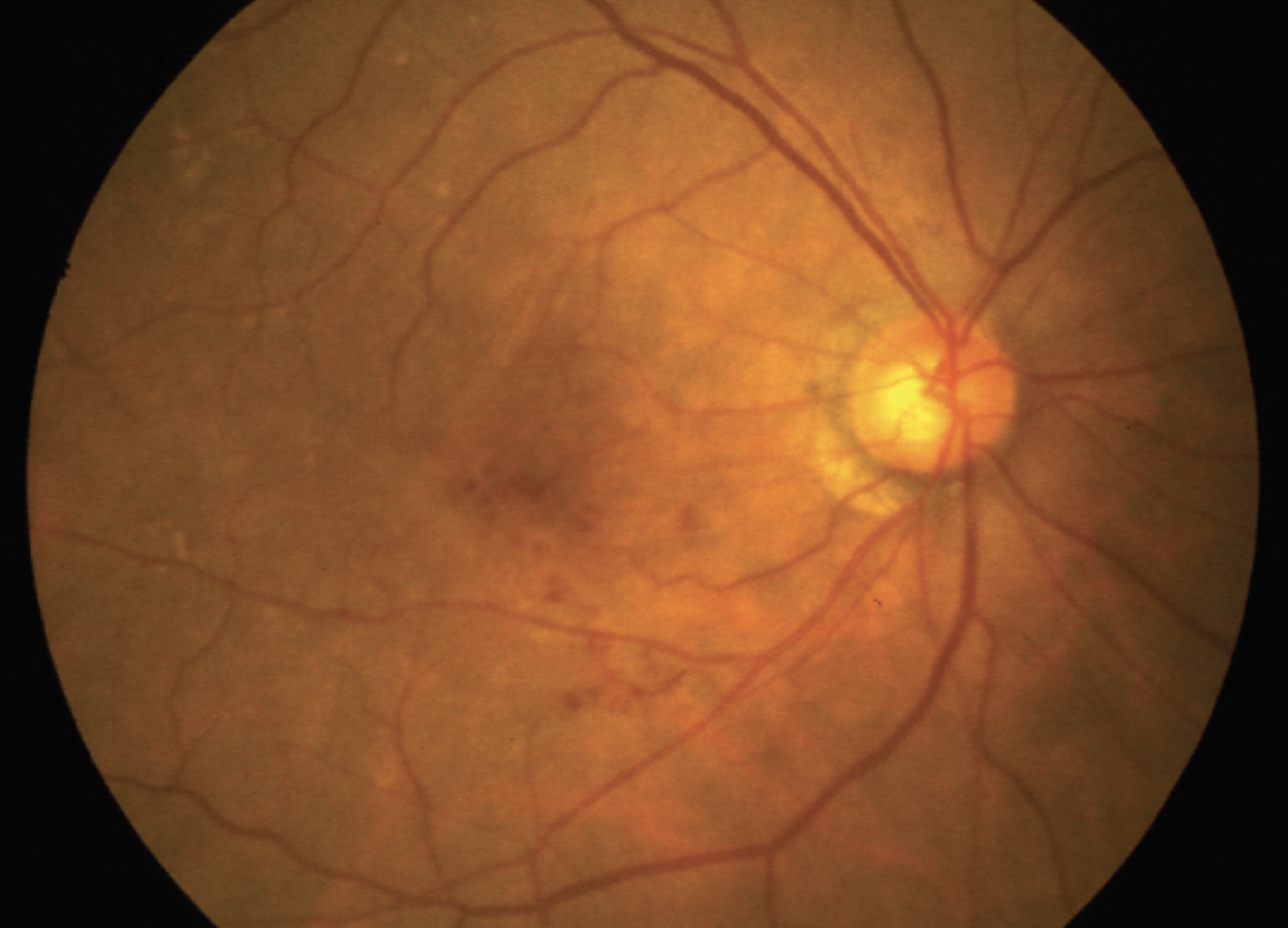 |
Since some patients with neovascular age-related macular degeneration respond insufficiently to anti-VEGF treatment despite maximal monthly intravitreal injections, researchers evaluated patients’ short-term responses between injections for extent and visual prognosis.
In the retrospective observational study, 45 eyes from 41 patients with refractory nAMD (who previously received at least 12 months of anti-VEGF treatment) were evaluated by optical coherence tomography in between monthly anti-VEGF injections. The fluid profile on OCT was evaluated before, and one week and one month after intravitreal injection using central retinal thickness (CRT), manual measurements and fluid-specific volumetric measurements performed by an automated AI-based algorithm.
Here are some of the findings:
• A significant improvement was found at week one in:
– CRT (p<0.0001);
– intraretinal fluid (IRF)(p=0.007);
– subretinal fluid (SRF)(p<0.0001); and
– pigment epithelium detachment (PED) volume (p<0.0001).
• Volumetric fluid measures revealed a >50 percent reduction at week one for IRF and SRF for approximately two-thirds of eyes.
• Poorer short-term response was associated with:
– larger exudative fluid amounts (IRF + SRF)(p=0.003);
– larger PED (p=0.007);
– lower visual acuity (p=0.004); and
– less anatomic changes at treatment initiation (p<0.0001).
• Univariate and multivariate analysis revealed that visual outcomes four and five years later were significantly worse with:
– weaker short-term responsiveness (p=0.005);
– presence of atrophy (p=0.01); and
– larger PED volumes (p=0.002).
Researchers wrote that incomplete responders to anti-VEGF showed a significant short-term response, identifiable at one week after injection, with rapid recurrence at one month. Weaker short-term responsiveness at one week was associated with poorer long-term visual prognosis. Researchers suggested such patients may need adjuvant treatment to improve their prognosis.
Eye (Lond) 2024; Jan 26. [Epub ahead of print].
Gigon A, Iskandar A, Kasser S, et al.
Ocular Surface Problems’ Effect on Cataract Surgery Outcomes
Scientists studied the visual outcome and postoperative complications of cataract surgery in patients with ocular surface disorders at a tertiary eye-care center in North India, as part of a retrospective observational study.
Patients with various ocular surface disorders with stabilized ocular surfaces who underwent cataract surgery during this period and had a minimum postoperative follow-up of six weeks were included. The primary outcome measures were postoperative best-corrected visual acuity at six weeks, best BCVA and postoperative complications.
The study included 20 men and 24 women. A total of 55 eyes were evaluated including those with the following issues:
• Stevens-Johnson syndrome (SJS)(35)
• ocular cicatricial pemphigoid (OCP) (4);
• dry eye (8);
• chemical injury (6); and
• vernal keratoconjunctivitis (VKC) (2).
Here were some of the findings:
• The mean duration of ocular surface disorders was 33.9 ±52.17 months.
• The median preoperative BCVA was 2.0 (IQR, 1.45 to 2).
• The median BCVA ever achieved was 0.50 (IQR, 0.18 to 1.45) at two months, and the median BCVA was achieved at six weeks was 0.6 (IQR, 0.3 to 1.5).
• Maximum improvement in BCVA was noted in patients with DED and SJS, with the least improvement in OCP.
• Phacoemulsification was performed in 47.27 percent of eyes, with intraoperative complications noted in 9 percent of eyes.
• Postoperative surface complications occurred in 12 eyes (21.82 percent).
• Other postoperative complications occurred in nine eyes (16 percent).
Scientists wrote that cataract surgery outcome can be visually beneficial in patients with ocular surface disorders provided ocular surface integrity is adequately maintained preoperatively and postoperatively.
J Cataract Refract Surg 2024; Jan 16. [Epub ahead of print].
Aggarwal M, Gour A, Gupta N, et al.
Efficacy and Safety of Faricimab for ME Due to RVO
Researchers evaluated the 24-week efficacy and safety of the dual angiopoietin-2 (Ang-2)/vascular endothelial growth factor-A (VEGF-A) inhibitor, faricimab, compared with aflibercept in patients with macular edema due to retinal vein occlusion, as part of two identically designed, Phase III, global, randomized, double-masked, active comparator-controlled trials: BALATON and COMINO.
Participants included patients ≥18 years of age with treatment-naïve foveal center-involved macular edema due to branch (BALATON) or central or hemiretinal (COMINO) RVO. Patients were randomized 1:1 to faricimab 6 mg or aflibercept 2 mg every four weeks for 24 weeks.
The primary endpoint was the change from baseline in best-corrected visual acuity at week 24. Efficacy analyses included patients in the intention-to-treat population. Safety analyses included patients who received at least one dose of study drug.
A total of 553 patients were enrolled in BALATON, and 729 patients were enrolled in COMINO. Here are some of the findings:
• The BCVA gains from baseline at week 24 with faricimab were noninferior to aflibercept in:
– BALATON (adjusted mean [95.03 percent CI change]: +16.9 letters; CI, 15.7 to 18.1 vs. +17.5 letters; CI, 16.3 to 18.6; and
– COMINO (+16.9 letters; CI, 15.4 to 18.3 vs. +17.3 letters; CI, 15.9 to 18.8).
• Adjusted mean (95.03 percent CI) central subfield thickness
reductions from baseline were comparable for faricimab and aflibercept at week 24, respectively, in:
– BALATON (-311.4 µm; CI, -316.4 to -306.4; and -304.4 µm; CI, -309.3 to -299.4); and
– COMINO (-461.6 µm; CI, -471.4 to -451.9; and -448.8 µm; CI, -458.6 to -439).
• A greater proportion of patients in the faricimab vs. the aflibercept arm achieved absence of fluorescein angiography-based macular leakage at week 24 in;
– BALATON (33.6 percent vs. 21 percent; nominal p=0.0023); and COMINO (44.4 vs. 30 percent; nominal p=0.0002).
• Faricimab was well-tolerated, with an acceptable safety profile comparable with aflibercept.
• The incidence of ocular adverse events was similar between patients receiving faricimab and aflibercept (20.4 percent [n=56] and 27.7 percent [n=100]) in:
– BALATON (16.3 percent [n=45]); and
– COMINO (23 percent [n=84]).
Researchers reported the findings demonstrated the efficacy and safety of faricimab, a dual Ang-2/VEGF-A inhibitor, in patients with macular edema secondary to retinal vein occlusion.
Ophthalmology 2024; Jan 25. [Epub ahead of print].
Tadayoni R, Paris LP, Danzig CJ, et al.




