If you look hard enough most medications will have some ocular effects. Over time, as I’ve seen more unusual-appearing corneal deposits and edema patterns, I’ve become attuned to more thoroughly reviewing a patient’s systemic medications. Since web searches for this topic can lead you down a rabbit hole of medications no longer in clinical practice (e.g., gold salts) or newly discontinued medications (e.g., belantamab mafodotin-blmf which was on an FDA REMS protocol)—I’d like to share with you cases I’ve compiled of patients presenting with corneal side effects of their systemic medications and presented in order of most frequent to least frequent that I’ve seen in my practice.
 |
|
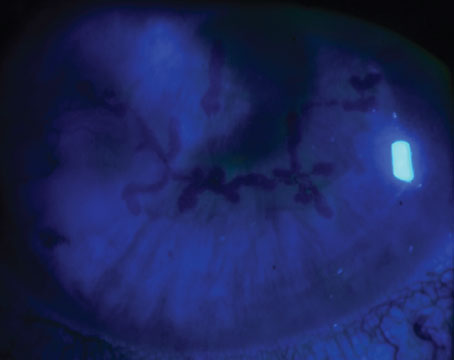
Ocular surface disease from dupilimab use is thought to be related to a reduction in goblet cells. |
Dupilumab (Dupixent)
A 25-year-old patient was referred by his allergist for evaluation of chronic red eye accompanied by tearing. He was treated initially for nasolacrimal duct obstruction without relief. He only found relief while he was on oral prednisone. This patient had started taking dupilumab injections for his severe eczema and, though his skin condition was improving, his ocular redness and inflammation continued to worsen.
Dupilumab is a human monoclonal antibody that inhibits the action of IL-4 and IL-3. It’s approved for patients over the age of 6 with refractory atopic dermatitis. Patients usually self-inject the medication every two to four weeks.
Dupilumab associated ocular surface disease has been reported in up to 34 percent of patients; sometimes this is directly drug related, and other times it’s an exacerbation of pre-existing ocular surface disease. The mechanism of the ocular surface disease has been evaluated by impression cytology and is thought to be related to a reduction in goblet cells. Case reports have shown a myriad of findings, ranging from mild disease and conjunctivitis to severe ulcerative keratitis. Most patients showing this side effect usually have underlying atopic dermatitis.
I vary the treatment based on the intensity of the symptoms. For milder disease profiles, I would consider topical ketotifen for the eye and topical tacrolimus for the lids. This usually helps to control the symptoms in most patients. Moderate intensity symptoms can be managed with topical cyclosporin (which has been shown to increase goblet cell density) and topical low-potency steroid (loteprednol 0.5% four times daily). If the disease course is more fulminant, then I’d favor starting crisaborole ointment for the lids with high-potency topical steroids (difluprednate 0.05% four times a day) and trying to taper the potency and frequency based on clinical response.
Amiodarone (Pacerone, Cordarone and Nexterone)
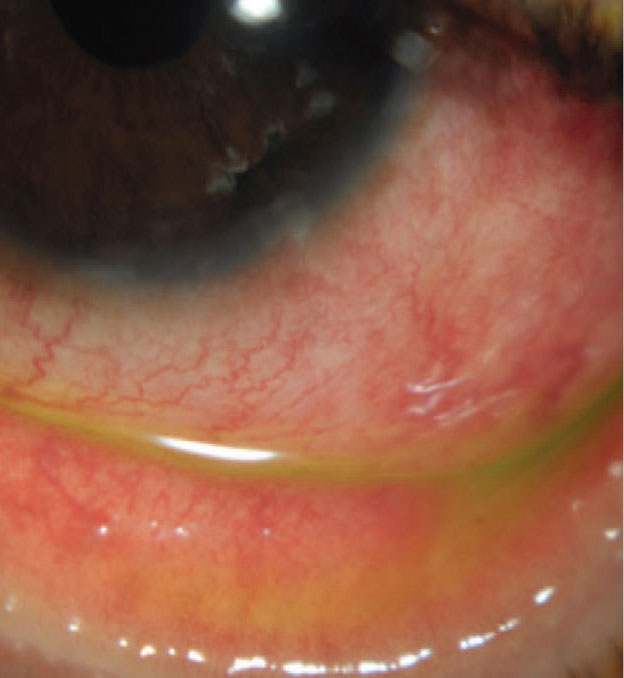
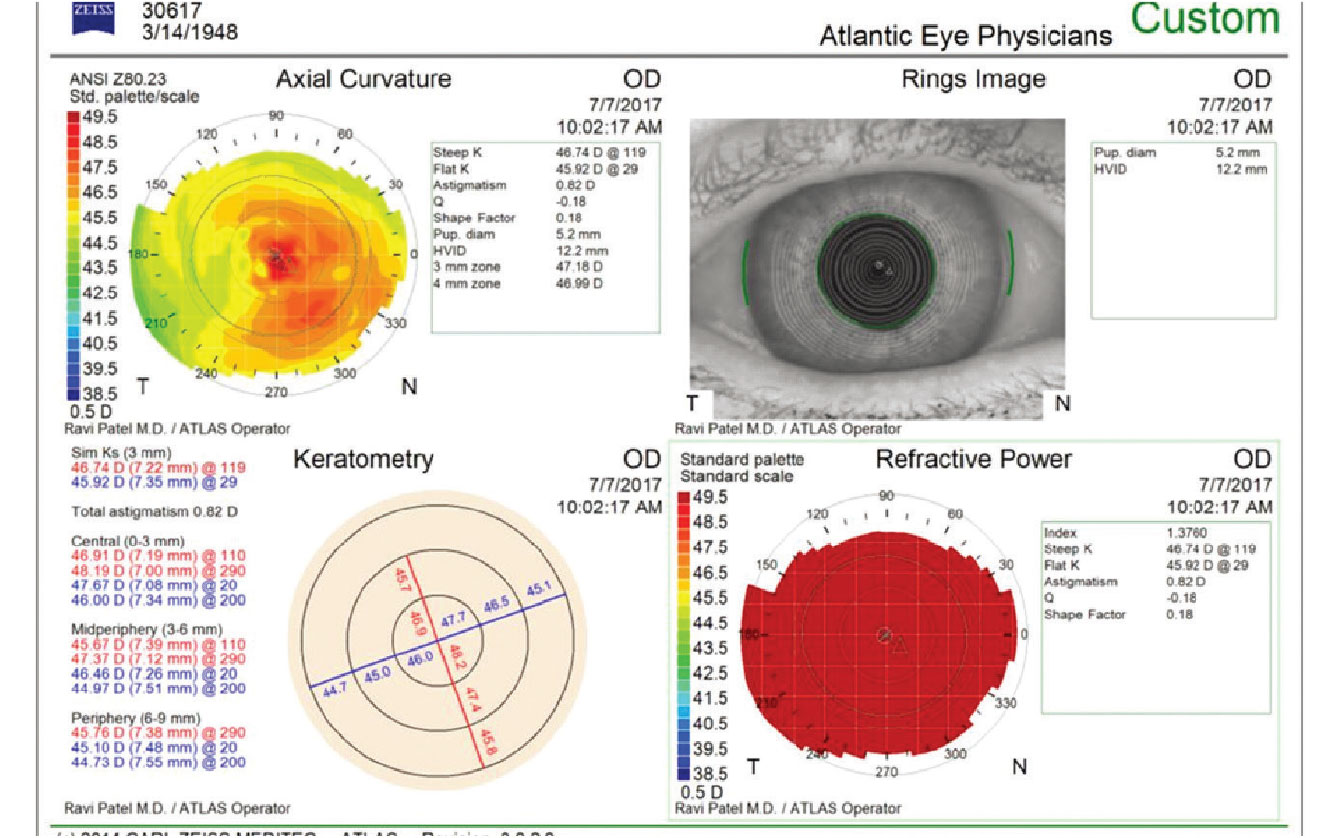
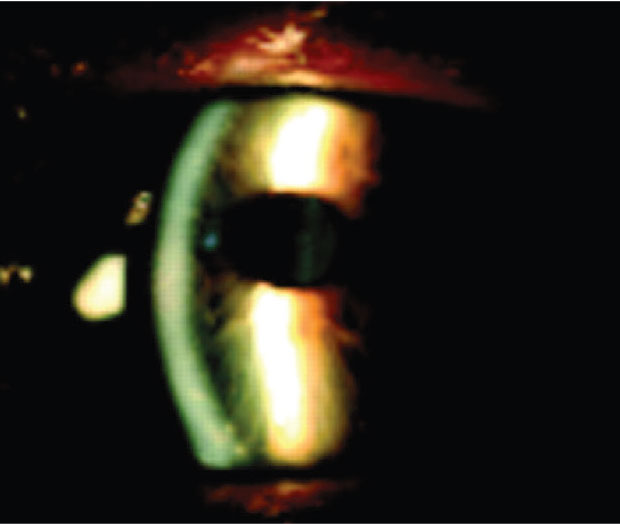
A 72-year-old patient presented for consultation with worsening of blurry vision since bilateral cataract surgery. His BCVA was 20/30 with his spectacles. His past medical history was significant for seasonal allergies, hypertension and atrial fibrillation following ablation. The patient has many allergies and she reports allergies to all preservatives as well as all hormones in meats. In the office, for many of these patients I’ll perform a diagnostic RGP refraction, which in this case showed improvement to 20/20. The topography showed irregular astigmatism. Exam showed the typical vortex keratopathy and, upon further questioning, the patient was treated with amiodarone for several years prior to her ablation.
Amiodarone is an Class III antiarrhythmic medication used to treat numerous cardiac dysrhythmias including potentially fatal ones. It’s part of ACLS life-saving protocols for cardiac arrest and can be used chronically for other arrhythmias. Besides the eye, it can deposit in the lungs, thyroid, liver, skin and peripheral nerves.
Amiodarone is an amphiphilic medication (which includes chloroquine, suramin, clofazimine, etc.), a class of drugs which has been long associated with whorl-like epithelial opacities. These were traditionally thought to be non-visually significant but I’ve seen many cases where these patients have irregular astigmatism and image blur from it. With improvements in technology to measure higher-order corneal aberrations, we’re finding that symptomatic patients who have abnormal topographies or corneal aberrations often benefit from treatment. There are recent reports of using topical heparin successfully to remove amiodarone related deposits. But this can be difficult to get compounded. So, I’ll offer these patients superficial keratectomy, particularly if they’re now off the offending agent. For most patients this is an office procedure with a rapid recovery. I most certainly do warn patients that this can cause a shift in their refractive error and will likely need an update in their spectacles after the procedure.
Amantadine (Symmetrel)
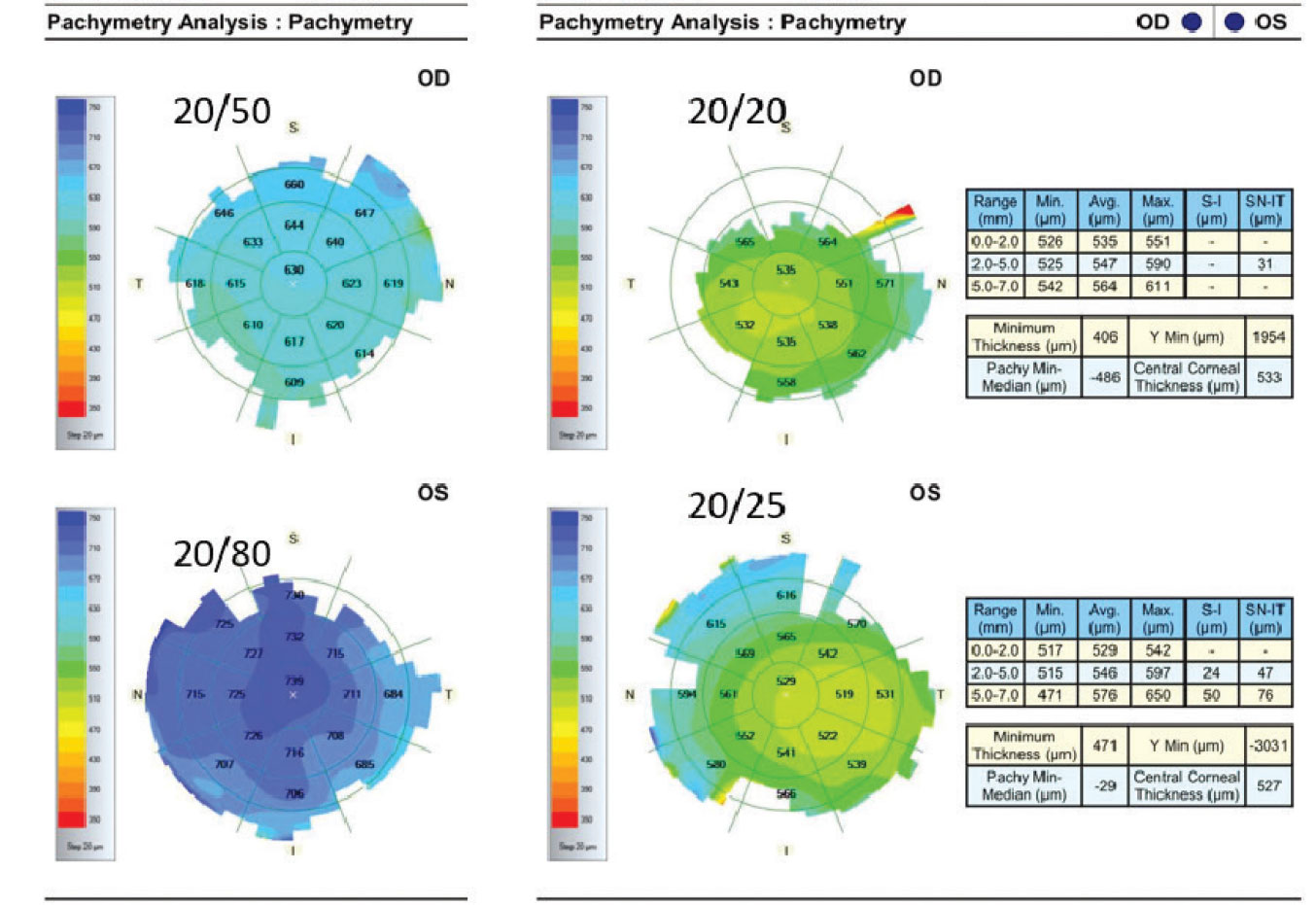
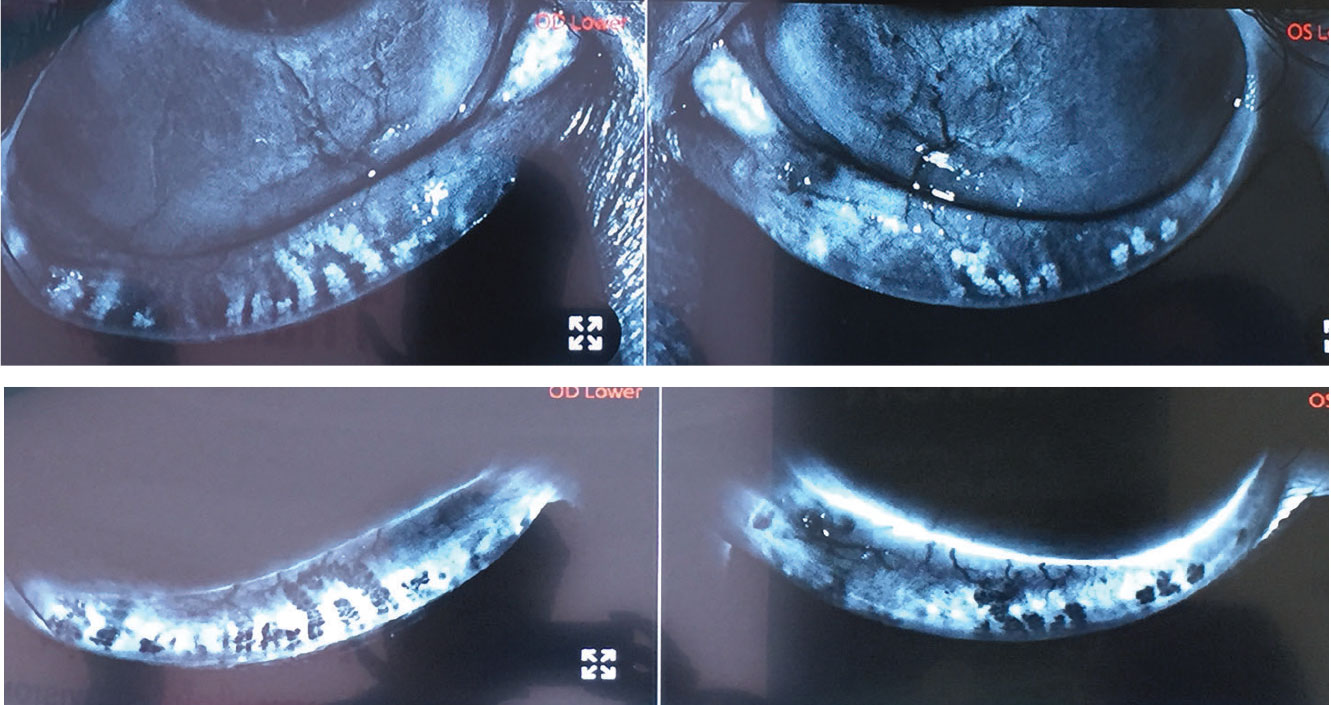
A 58-year-old man was referred by his primary eye doctor for evaluation for possible endothelial keratoplasty due to progressive corneal edema. He was treated with hypertonic saline drops and prednisolone acetate 1% drops without any improvement. He was subsequently tried on oral valacyclovir presuming bilateral herpetic keratitis without improvement. The patient’s wife noticed he developed extraocular edema and was prescribed neo-poly-dex ointment. He had no relevant ocular history. He’s currently under the care of his neurologist for early-onset Parkinson’s Disease and has a stent placed for coronary artery disease. His examination reveals diffuse stromal edema with endothelial folds and some asymmetry in both eyes. His visual acuity is 20/50 OD and 20/80 OS and his IOP is 20 mmHg OU.
Initially, I was quite perplexed how this younger man with no ophthalmic history had progressive edema which was non-responsive to medical therapy. The referring doctor went down the pathway as I usually would, considering some traumatic event, hypotony (but his IOP was normal), viral illness (most are unilateral), inherited disease (Fuchs’ endothelial dystrophy without guttata—very rare) and post-surgical sequelae. I finally reviewed his medication list and saw amantadine on the list.
 |
|
The whorl-like epithelial opacities often associated with the use of the cardiac drug amiodarone can result in irregular astigmatism and image blur. |
Amantadine is a nicotinic antagonist/noncompetitive NDMA antagonist which was initially used a prophylaxis for influenza A. It was learned this medication can reduce dyskinesias from dopamine medications and therefore it has since been FDA approved for treatment of Parkinsonian dyskinesias. My initial treatment was to call the movement-disorder specialist to recommend cessation of amantadine. I added topical steroids and topical timolol to aid in his corneal recovery. As you can see by the attached OCT pachymetry maps his corneal edema and vision improved over two months back to 20/20 and 20/25. Since I initially saw this case, I’ve seen numerous patients with the same side effect both as outpatient and inpatient/emergency room consultations for blurry vision.
Osimertinib (Tagrisso)
A 63-year-old nonsmoker presented for evaluation of blurred vision. He had a history of retinitis pigmentosa and took brinzolamide three times a day. His past medical history was relevant for Stage 4 non-small cell lung cancer. His ocular surface showed a severe vortex keratopathy in both eyes. His visual acuity was limited by his retinitis pigmentosa to 20/80 and 20/40, but he was subjectively aware of a decline.
Osimertinib is a third-generation EGFR tyrosine kinase inhibitor which is used as a first-line therapy for T790M mutation EFGR-positive NSCLC. It’s a daily oral agent capable of producing impressive improvements in progression-free survival.
Epithelial growth factor receptor (EGFR) inhibitors can cause side effects to any epithelial cells. Therefore, side effects include diarrhea, skin rash/inflammation, low blood cell counts and interstitial lung disease. Dry eye and whorl-like keratopathy are common in these patients. Since this is noninflammatory, steroids are of very limited use in the treatment of this condition. Many patients will become resistant to osimertinib within 10 months of treatment commencement and the condition is reversible with cessation of therapy. I have anecdotally found lubrication, bandage lens and amniotic membrane transplant can be helpful in select cases. Rarely, this class of medications can cause stromal deposits as well. As with any medication, this is one where it’s especially important to balance the impact of drug cessation/modification weighed against the risk of systemic disease progression.
Isotretinoin (Common brands: Accutane, Zenatane, Absorica)
A 22-year-old patient presented for consultation for laser vision correction. He had a stable refraction for several years, is mostly a spectacle wearer due to contact lens intolerance. He has no relevant family history and is a moderate myope with otherwise normal tomographies. He takes no medications and has no allergies. Careful examination of this eyelids showed severe meibomian gland dropout and you can see this on meibomography. Upon further questioning he admitted to isotretinoin use as a teenager for acne.
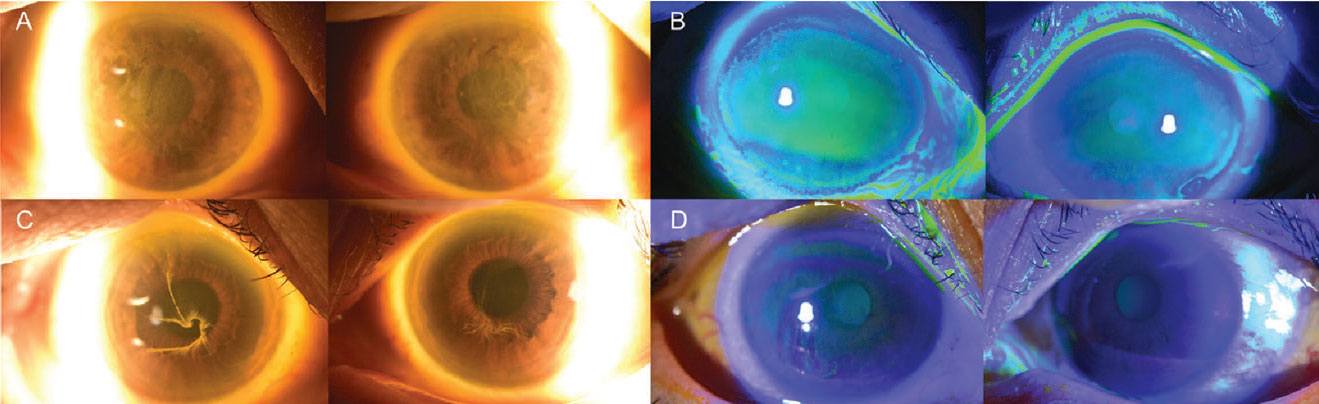 |
|
Osimertinib (Tagrisso), an oral medicine for lung cancer, can cause serious side effects to epithelial cells. Lubrication, bandage lenses and amniotic membrane transplant can be useful in certain cases. |
Isotretinoin is also known as 13-cis-retinoic acid and is used to treat severe acne which is refractory to other treatments. It’s been used in a variety of other dermatologic conditions, and its side effects resemble Vitamin A toxicity. As a fat-soluble essential vitamin the effects are diverse throughout the entire body. Prescribing is highly restricted and monitored through a website called iPLEDGE due to is teratogenic effects.
Isotretinoin is linked to blepharitis, conjunctivitis and dry-eye disease. Very rarely can it lead to cataract, color blindness, night blindness, contact lens intolerance, corneal opacification/keratitis and even papilledema. In this case the patient’s reported symptom of contact lens intolerance and meibomography showing severe loss of meibomian glands is consistent with his previous use of isotretinoin. Unfortunately, there’s no treatment to reverse this toxicity and conventional therapies for blepharitis are his only option.
Rifabutin (Mycobutin)
A 74-year-old smoker with COPD presents with a recent diagnosis of mycobacterium avium complex pulmonary infection. He was started on ethambutol and is following up for his scheduled screening exam. He’s pseudophakic and takes lifitegrast 5% topically for dry-eye disease and has undergone SLT laser treatment for ocular hypertension. On exam his acuity was 20/30- and his IOP was 17 in each eye. He had normal color vision and no evidence of optic pallor on exam. His corneal exam showed peripheral circumferential yellow-brown deposits deep in the cornea. His entire medication list was reviewed and he was on a three-drug regimen which included ethambutol, rifabutin and clarithromycin.
Rifabutin is an antibiotic in the rifamycin family of medications which blocks RNA production in bacteria. It’s typically used to treat tuberculosis and MAC, but is also employed in the treatment of Bartonella and Babesia colonies.
In the cornea, these yellow-brown deposits, which usually start peripherally then can progress to involving the central cornea, are actually deep stromal lesions. Confocal microscopy has shown they don’t deposit in the endothelium, therefore they’ve not been associated with endothelial dysfunction. The prognosis of these lesions is unknown as they’re rare and don’t resolve with discontinuation of the medication. However, in an effort to prevent further progression, I spoke to the patient’s infectious disease specialist about modifying his treatment and discontinuation of the rifabutin. Rifabutin has been linked to uveitis and retinal dysfunction, both of which are presumed to be reversible with discontinuation of the medication.
Tamoxifen (Common brands: Nolvadex, Soltamox)
A 79-year-old woman’s primary eye doctor referred her for evaluation of corneal changes. Patient’s presenting complaint was progressive photophobia. Her past medical history included hypertension, osteoarthritis, breast cancer (and subsequent mastectomy) and radiation at age 62. Her visual acuity was 20/40 OU BAT to 20/100 OU. On examination she had refractile subepithelial deposits consistent with a drug-induced keratopathy. Tamoxifen was listed during a review of her systemic medications.
 |
|
A patient on amantadine for Parkinson’s had diffuse stromal edema and endothelial folds and some asymmetry bilaterally. His acuity was 20/50 in the right eye and 20/80 in the left (maps on the left). After cessation of the amantadine and the use of topical steroids and timolol, in two months the vision improved (right). |
Tamoxifen is a selective estrogen receptor modulator used to prevent breast cancer. The most common side effects reported from its use are endometrial cancer, thromboembolism and hepatotoxicity. Most patients are treated for five years for secondary prophylaxis of breast cancer.
Tamoxifen is usually associated with dry-eye disease but rarely can cause keratopathy, retinopathy and cataracts. In this case, my patient had classic corneal findings which are rarely reported. This keratopathy is typically reversible with cessation of therapy. The patient was continued on the medication inadvertently as she had transitioned through oncologic care through relocation and retirement of her doctors. I spoke with her medical oncologist to ascertain if this was necessary for her ongoing treatment. Ultimately, since it has been more than 10 years of treatment, the patient was advised to discontinue the therapy. Her photophobia improved dramatically within the first three months. Over the following year most of her deposits resolved with surface lubrication and topical cyclosporin 0.05%.
Indomethacin (Common brands: Indocin and Tivorbex)
A 63-year-old patient was referred to see me for progressive corneal changes in both eyes with concern for monoclonal gammopathy of undetermined significance (MGUS) or multiple myeloma. Past medical history included lung cancer, skin cancer, hypertension, well-controlled diabetes mellitus type 2 and rheumatoid arthritis. The patient had visual acuity of 20/25- in both eyes and has been treated for dry-eye disease with topical lubricants. On examination he was found to have fine specks throughout the stroma. As a patient with a previous history of lung cancer his rheumatologic ailments were being managed with oral NSAIDs in lieu of biologic agents and of course he found the best relief with indomethacin.
 |
|
Isotretinoin, used to treat severe acne, has been linked to blepharitis, conjunctivitis and dry eye. This patient showed severe loss of meibomian glands, most likely due to a history of isotretinoin use. |
Indomethacin is one of the most potent NSAIDs available for joint disease, headache, fever and most importantly pain relief. Indomethacin is used acutely in most cases and rarely are side effects from chronic use encountered. Indomethacin is unique from other NSAIDs in that in addition to its role as a COX inhibitor it’s been found to reduce cerebral blood flow through vasoconstriction and nitric oxide pathways, making it helpful in treatment of certain headaches. It’s a tocolytic that’s helpful in delaying premature labor and it can cross the placenta and be used for treatment of polyhydramnios.
Indomethacin can cause a whorl keratopathy as well as stromal deposits. There’s some evidence that this drug can cause a pigmentary retinopathy, including bulls-eye retinopathy. In this case the findings were limited to the cornea and, though paraproteinemic keratopathy was in the differential for a patient with previous malignancies, I ordered an SPEP and UPEP to rule out MGUS and myeloma. I decided to first discuss alternative treatment options with his rheumatologist to see if we could reduce the dose or even stop the indomethacin. The patient was very reluctant since he knows how disabling his arthritis can become. Eventually he did a trial of corticotropin gel injection and there was some improvement of his deposits, but this was short-lived as he didn’t like doing injections twice weekly, so he ended up back on indomethacin.
 |
|
The antibiotic rifabutin can cause yellow-brown corneal deposits that are actually deep stromal lesions, and can involve the central cornea. |
In summary, this list isn’t exhaustive or even comprehensive, but is simply a cross-section of patient referrals I’ve seen in clinical practice. However, being familiar with it can be helpful: You might become a “zebra hunter” when looking for some of these conditions, but if there’s evidence of an unusual finding in the cornea, a careful review the patient’s systemic medications just may result in a surprise.
Dr. Patel is on the cornea service at Wills Eye Hospital in Philadelphia, and is a clinical assistant professor, Sidney Kimmel College of Medicine at Thomas Jefferson University.
Suggested Reading
Hollander DA, Aldave AJ. Drug-induced corneal complications. Curr Opin Ophthalmol 2004;15:6:541-8.
Blomquist PH. Ocular complications of systemic medications. Am J Med Sci 2011;342:1:62-9.
Raizman MB, Hamrah P, Holland EJ, Kim T, Mah FS, Rapuano CJ, Ulrich RG. Drug-induced corneal epithelial changes. Surv Ophthalmol 2017;62:3:286-301.
Sahyoun J, Sabeti S, Robert M. Drug-induced corneal deposits: an up-to-date review. BMJ Open Ophthalmology 2022;7:e000943. doi: 10.1136/bmjophth-2021-000943
Popiela MZ, Barbara R., Turnbull AMJ, et al. Dupilumab-associated ocular surface disease: Presentation, management and long-term sequelae Eye 2021;35:3277–3284.
Frings A, Schargus M. Recovery from amiodarone-induced cornea Verticillata by application of topical heparin. Cornea 2017;36:11:1419-1422.
Jeng BH, Galor A, Lee MS, Meisler DM, Hollyfield JG, Schoenfield L, McMahon JT, Langston RH. Amantadine-associated corneal edema potentially irreversible even after cessation of the medication. Ophthalmology 2008;115:9:1540-4.
Shin E, Lim DH, Han J, et al. Markedly increased ocular side effect causing severe vision deterioration after chemotherapy using new or investigational epidermal or fibroblast growth factor receptor inhibitors. BMC Ophthalmol 2020;20:19.
Zhang P, Tian L, Bao J, Li S, Li A, Wen Y, Wang J, Jie Y. Isotretinoin impairs the secretory function of meibomian gland via the PPARγ signaling pathway. Invest Ophthalmol Vis Sci 2022;63:3:29.
Gurlevik U, Kemeriz F, Yasar E. The effect of isotretinoin on meibomian glands in eyes: A pilot study. Int Ophthalmol 2022;42:7:2071-2078.
Golchin B, McClellan K. Corneal endothelial deposits secondary to rifabutin prophylaxis for Mycobacterium avium complex bacteraemia. Br J Ophthalmol 2003;87:6:798-9.
Nayfield SG, Gorin MB. Tamoxifen-associated eye disease. A review. J Clin Oncol 1996;14:3:1018-26.