There are as many types of nuclei a cataract surgeon may encounter as there are techniques to break them. Although some of these techniques are used more often than others, situations do occur when a less-employed technique comes in handy. We asked cataract surgeons about their personal preferences, honed over years of experience, and what makes them favorable compared to others.
Divide and Conquer
This continues to be the most widely used technique despite the arguments against its efficiency.
Introduced in 1991 by Howard V. Gimbel, MD, this technique involves creating a deep central groove in the nucleus, which is then manually cracked and then fragmented into sections before it’s emulsified.1 According to Dr. Gimbel, this technique makes it possible to use phacoemulsification on patients with small pupils or hypermature and brunescent cataracts who would otherwise not be candidates.
In a 2022 survey conducted by Review of Ophthalmology, 46 percent of respondents named divide and conquer as their preferred technique, with many citing its safety and application for multiple types of cataracts.
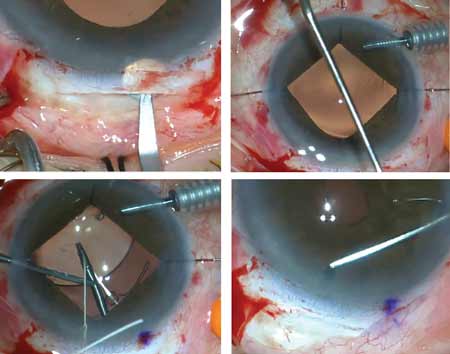
 |
|
Divide and conquer is the first technique residents are taught. The nucleus is divided into four quadrants before phacoemulsification. Some surgeons prefer this technique for its safety and usefulness on multiple types of nuclei, while others argue it’s too time consuming. (Courtesy Uday Devgan, MD) |
Another factor that plays into its popularity is that it’s usually the first technique taught to residents.
“I’m at a university and when we’re teaching residents how to perform phaco, we’ll initially do a four quadrant divide-and-conquer technique,” says Nick Mamalis, MD, a professor of ophthalmology at the John Moran Eye Center, University of Utah. “What this allows us to do is make two grooves 90 degrees apart, essentially dividing the nucleus into quadrants, manually separate the pieces, then phaco them. It’s a tried-and-true method of doing the nucleus disassembly and it’s a safe way of doing it. We start our residents doing this prior to going to the chop techniques.”
Cristos Ifantides, MD, MBA, who’s in private practice in Cape Coral, Florida, and an adjunct assistant professor of ophthalmology at the University of Colorado, says he was only taught divide and conquer during his residency. “I was never taught how to chop in residency,” he says. “I only learned chop in my fellowship at Wills, but every residency program is different.”
Surgeons speculate that their colleagues may continue to employ divide and conquer years after residency purely because of the comfort level, but most advance on to chop techniques.
“Divide and conquer puts a lot of energy into the eye, and it’s a slower, inefficient procedure,” says Uday Devgan, MD, FACS, who practices in Los Angeles and previously taught at UCLA. “It’s also riskier than chop because, when you make the phaco grooves, the tip is 1 mm or less from the posterior capsule. When performing a chop technique, you’re never near it.”
Phaco Chop
There are a few variations to the phaco chop, from the “stop-and-chop” to vertical and horizontal chop, and these have a bit more of a learning curve.
“Once a person has more experience and is more comfortable doing phacoemulsification, more comfortable using two hands rather than one hand, then they can go to a chop technique,” says Dr. Mamalis.
“I’ve taught surgeons in other parts of the world and chopping is a difficult skill to teach and it can be very difficult to learn, even with a good teacher and talented learner,” says Dr. Ifantides. “You need multiple cases to learn it and dozens of cases to get good at it. It’s more technical and can be frustrating.”
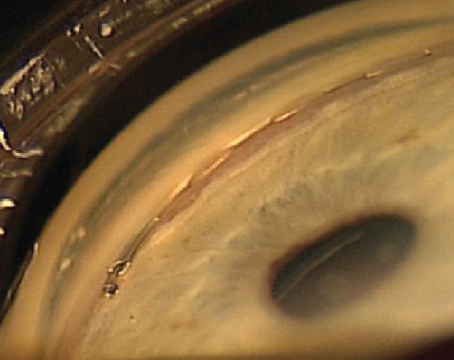
 |
|
For very dense cataracts, Cristos Ifantides, MD, describes this “Rotary Chop” technique in which pilot holes are created by the phaco tip around the periphery of the nucleus, which helps penetrate deeper into the posterior plate to propagate a crack. (Courtesy Cristos Ifantides, MD) |
Stop and chop is a good bridge between divide and conquer and phaco chop, says Dr. Devgan. Described in 1994 by Paul Koch, MD,2 this requires creating a trench in the nucleus to create two halves, similar to the beginning of divide and conquer, but then you switch to a phaco chop to crack the nucleus. “Instead of breaking it into four quadrants, we’ll break it down the middle and make two halves and then each half can be brought up to chop and it’s easier to do,” Dr. Devgan continues.
For those who are looking to advance their skills and increase their volume of cataract surgeries, the horizontal (or Nagahara) and vertical phaco chops are arguably the most efficient techniques. Kunihiro Nagahara, MD, presented the horizontal chop technique in 1995, which brings together the tips of the chopper and the phaco handpiece within the horizontal plane. The phaco tip holds the nucleus in place with the vacuum level building up to keep it secure, explains Dr. Devgan. “You then have a small window of about one to two seconds to perform the chop, otherwise the vacuum slowly breaks down the nucleus and you lose the grip,” he says.
Vertical chop is another option, this time performed in the vertical plane. Both Dr. Mamalis and Dr. Ifantides say vertical chop is their most common technique used.
“I do like the stop-and-chop technique, using a vertical chop,” says Dr. Mamalis. “I make a groove that’s no more than 1.5 phaco tips in diameter and about 80-percent depth of the nucleus. That gives me enough room that I can go in and do the vertical chop. Once I’ve made the groove, I crack the nucleus in half using the chopper through a sideport incision and then the phacoemulsification handpiece through the main incision. Once it’s cracked, I rotate the nucleus 90 degrees.
“Depending on the hardness of the nucleus, I’ll either do one or two chops to break up the nucleus either into quarters or into thirds just depending on how firm the nucleus is,” he continues. “If the nucleus is very firm, we want to really try to chop it into smaller pieces, so we use less phacoemulsification energy. When the nucleus is just moderately firm, we could even just chop it in half with a single chop on each hemi-section and then go ahead and use phaco to emulsify the piece of nucleus and take it out.”
Dr. Ifantides says he opts for this technique because it uses the least amount of phaco energy and can be employed in most cases. “It ends up being quite fast,” he says. “Chopping really depends on the chopper—the second instrument. For vertical chopping you want to be able to use a sharper second instrument that can impale the nucleus. With the phaco you burrow in and impale the nucleus, hold it in place with high vacuum and then the chopper gets buried into the nucleus as well and then you pull the two together. The vertical component is really the puncturing into the lens with the chopper and then bringing the two instruments together, propagating a crack.”
Dr. Mamalis says he likes the control of a vertical chop. “You can do it on most densities of nuclei, unless they’re severely dense, which is—at least nowadays in the United States—not that common,” he says. “But for most levels of nuclei density, I find that I get good control with a vertical chop. I like to use the stop and chop because I like to make a thin groove in the middle of the nucleus and then crack it in half, and then do the vertical chop. Many surgeons don’t do the groove—they just go right in and chop, but I like the little bit of room that it gives me when I make a small groove and crack the nucleus. Then it allows me to chop the hemi-sections more easily.”
For those who are in the process of learning the vertical chop, Dr. Mamalis says there are some pearls to keep in mind. “You want to make sure that your phacoemulsification tip has a good purchase on the piece of nucleus that’s being chopped, meaning that you have a high enough vacuum that the piece is fixated to the phaco tip to go ahead and to make the chop,” he says. “What we find when we’re teaching residents early is they’re just a little bit shy about keeping that vacuum power up high to keep that piece of nucleus held tightly so that you can make a chop. So, oftentimes, they’ll begin to chop and then the piece of nucleus falls off the phaco tip and they can’t complete the chop. Whenever you’re doing any kind of a vertical chop technique, it’s very important that you have the phaco tip adequately buried into that piece of nucleus and enough vacuum that it doesn’t let go of the nucleus as you’re doing the chop. Often, there’ll be a setting that you can set, depending on your phaco machine, either a quadrant setting or chop setting, and that has a much higher vacuum than does the setting that you use when you’re grooving the nucleus initially.”
One of the most important pearls of phacoemulsification is being aware not to disturb either the anterior capsule or going so deep that you risk rupturing the posterior capsule. “You always want to be aware in three dimensions of how deep you’re going with the phaco, where your chopper is, and sometimes in a darker nucleus or denser nucleus—again looking at residents when we’re training them—make sure to put that chopper in so it doesn’t disturb the anterior capsule,” Dr. Mamalis advises. “You don’t want to accidentally cause a tear to form in the anterior capsule with your chopper.”
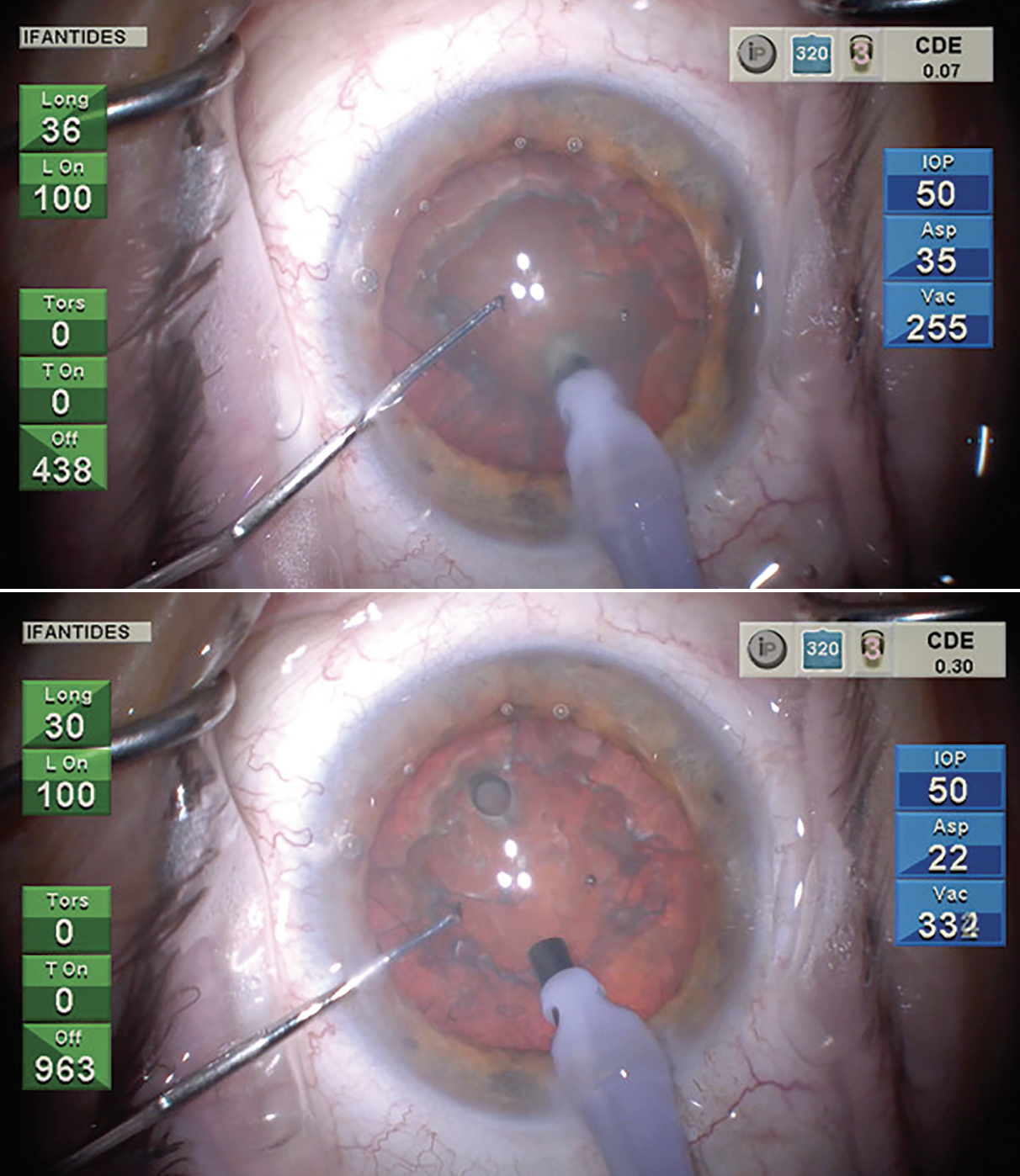
 |
| Chop techniques weren’t always included in residency programs and there’s a learning curve to the variations, say surgeons. Some favor the vertical chop (shown here) for its speed and reduced use of phaco energy. (Courtesy Uday Devgan, MD) |
When to Consider Other Techniques
One technique doesn’t necessarily fit all, so it’s important to stay up to date on other methods for breaking the nucleus.
• Soft nucleus. Dr. Ifantides says vertical chop isn’t ideal if the cataract is soft and young. “In this case I’ll either prolapse the lens into the anterior chamber, or I’ll do a partial divide and conquer where I’ll make a three-quarters length groove rather than a full groove and crack the distal portion of the cataract in half, leaving it attached sub-incisionally, and then switch to quadrant removal and aspirate the left distal side,” he says. “Because it’s still connected, as you vacuum it and eat up that hemi-nucleus the other hemi-nucleus rotates around and comes with it. It’s a pretty quick way to do that. I personally don’t vertical chop soft cataracts with high aspiration/vacuum.”
In soft cataracts, Dr. Mamalis says he uses a pre-chopping instrument. “In a softer nucleus you go in with the pre-chopper and you bury it into the nucleus and then spread the blades of the pre-chopper and that will actually divide the nucleus in half and then you can rotate it 90 degrees and again, bury the pre-chopper into the nucleus and then spread it apart and do the cracks with the pre-chopper,” he says. “So in a softer nucleus where it’s very difficult to do a chopping technique itself, I use the pre-chopper to divide it into four quadrants and then just do a four-quadrant technique.”
• Hard/dense cataracts. For very hard nuclei, that’s a different matter, says Dr. Mamalis. “If you have an extremely hard nucleus, it’s sometimes very difficult to break that into smaller pieces that you can then emulsify and so those are the patients where we can sometimes use the miLoop, which can actually help to break a very hard nucleus in either semi-halves or quadrants,” he says.
Another technique is the small-incision extracapsular extraction, which is commonly used in the developing world or in places without access to phaco. “The advantage of this technique is you do a scleral corneal tunnel with a frown shape to it—think of it as an upside down U—then you use a blade to go half thickness through the sclera until you enter the cornea and then enter the anterior chamber. You then can make a wider internal opening than there is an external opening and that allows you to remove the very hard nucleus whole without having to disassemble it,” continues Dr. Mamalis.
Dr. Ifantides described a technique called the rotary chop for dense cataracts.3 In this technique, the surgeon makes a hole in the cataract, spins it around and puts the chopper in that hole, then makes a second hole with their phaco needle again, like in a regular vertical chop. “That helps get deep into the posterior plate and propagate a crack,” he says. “We published that a couple of years ago. After publishing it, I found another surgeon who has also been doing that technique, James Katz, MD. He presented that about 10 years ago at a meeting I didn’t happen to attend, so I always want to give credit where credit’s due. That’s another way for dense cataracts to be segmented.”
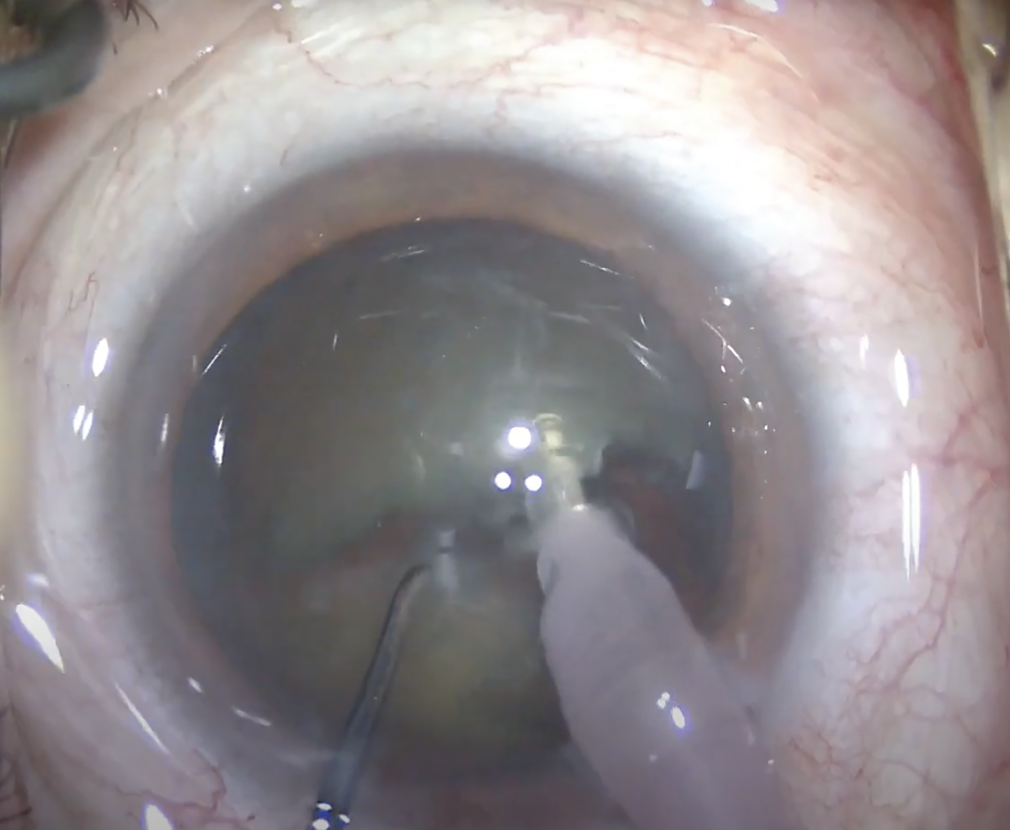
He will also occasionally do a horizontal chop. “I’m actually part of a clinical trial where I have a chopper with a light at the end of it and you can use that for horizontal chopping,” Dr. Ifantides says. “It’s called the iChopper (Oculight). It’s helpful for horizontal chop and all types of nucleo-fractis if the visibility isn’t that great.”
• Loose zonules. Dr. Mamalis says vertical chop is applicable in patients with pseudoexfoliation. “In cases where there might be some issues with the capsular fragility or with zonule adherence, for example, patients with exfoliation syndrome, I do find that stop and chop with a vertical chopper is actually a very zonular-friendly technique,” he says. “We’ll often use that even in patients with exfoliation syndrome or with some questions about the integrity of the zonules all the way around.”
• Phaco flip/tilt. This technique has fallen out of favor somewhat, but comes down to personal preference. “It could be useful for a brunescent cataract,” says Dr. Devgan.
There are a few too many risks with this technique, says Dr. Ifantides. “Some people still use it for soft cataracts and for loose zonules, but others will do it every single time where they’ll prolapse the lens on purpose, at least partially out of the bag, trying to keep it away from the posterior capsule,” he says. “I don’t love this technique because you end up putting strain on the anterior capsule, and in refractive-cataract surgery, we prefer to have an anterior capsule that overlaps the optic of the premium IOL. In order to do that you need a 5.5-mm or less capsulotomy. It’s hard to prolapse a more mature cataract from that and to be working with the lens partially prolapsed can put a lot of strain on the anterior capsule and cause an anterior capsular rent. I think people who make bigger capsulotomies like this technique a bit more unless they prolapse it all the way out, basically putting the cataract in the anterior chamber and eating it there. The con being you’re closer to their cornea and the lens can hit the cornea.”
Continuing Education
Dr. Devgan says it’s important for all surgeons, even those in mid-career, to keep learning and that includes phaco chop if they haven’t mastered it already. “It’s not that difficult and it will be far more effective,” he says.
Dr. Ifantides says not to get discouraged when attempting new techniques. “Surgeons will give up on something before they may have adequate performance on it,” he says. “We fail to compare certain techniques. To graduate residency you need 80-plus cataract surgeries that are pretty much all done with phaco. If you gave somebody a phaco machine and asked them to try it for the first time and give you feedback, I think most people would say it’s not an ideal device. It takes training and persistence to master. We should have the same mentality of saying, ‘If it takes 80-plus times to get safe with phaco, and way more to get really good with phaco, maybe we should be giving other devices and techniques a chance beyond just one or five or 10 tries.’ ”
It’s important not to become complacent, either, Dr. Ifantides continues. “If you’re doing the same style, type, steps of surgery as you were five years ago, you’re not reading enough or trying things out enough because things continue to improve,” he says. “Being plastic, I think, is really important, and having that desire to see how other people operate is important. Any chance that people get to spend time in other surgeons’ ORs is very valuable. No matter how good you think you are, there’s always something to learn from another surgeon and it’s really eye opening when you do that. You’ll always pick up skills if you’re paying attention.”
Dr. Chayet is considered a pioneer in refractive and cataract surgery, and is the medical director of the Codet Vision Institute in Tijuana, Mexico. He is a clinical investigator for RxSight, LensGen and ForSight Vision6.
Dr. Devgan is the owner of CataractCoach.com. Dr. Ifantides discloses relationships with Alcon, Bausch + Lomb, Johnson & Johnson Vision and Centricity. Dr. Mamalis has no related disclosures.
1. Gimbel HV. Divide and conquer nucleofractis phacoemulsification: Development and variations. J Cataract Refract Surg 1991;17:3:281-91.
2. Koch PS, Katzen LE. Stop and chop phacoemulsification. J Cataract Refract Surg 1994;20:5:566-70.
3. Ifantides C, Sieck EG, Christopher KL. Rotary chop: A new technique for teaching chop and tackling mature cataracts. Ophthalmol Ther 2020;9:2:321-327.