As a surgeon who performs both refractive and cataract lens surgery, I see the full spectrum of presbyopic patients, from the refractive patient looking to improve his uncorrected vision to the cataract patient hoping to regain his sight. After working with the accommodative Crystalens for two years, I believe that this device is a good option for the management of both these groups of presbyopes. Here are my impressions and my advice if you're looking to get involved with this recently approved device.
The Crystalens Explained
Before embarking on a discussion of implanting the lens, it helps to understand the lens's design and how it works.
 |
| When you implant the inferior loops and haptic, don't let go of the lens. |
After implantation in the capsular bag, the lens vaults posteriorly, and remains that way as it is encapsulated by fibrosis of the bag. The proposed mechanism of the Crystalens is that accommodation is restored through the action of the ciliary muscle. Upon constriction, the muscle undergoes a redistribution of mass, which increases vitreous pressure. This is believed to force the lens forward, changing the refractive power of the eye. Movement of the lens has been demonstrated using pharmacological stimulation, but a validated technique for measuring the movement of pseudophakic accommodation under physiologic conditions does not yet exist. Researchers, such as Dr. Adrian Glasser, are currently working to devise an accurate, valid way of measuring pseudophakic accommodation. The proposed mechanism of the Crystalens simply cannot be confirmed until these methods of measurement are devised and validated.
The Ideal Patient
The U.S. Food and Drug Administration clinical trial of the Crystalens demonstrated that it's safe and effective for a wide range of cataract patients. It also seems to be very good as a refractive procedure especially for the aging hyperope, age 55 years old or older, who has some evidence of lenticular changes. The lens is able to give the older hyperope a more natural range of visual function than any of the currently available corneal refractive procedures.
As with any refractive procedure, it is important to establish realistic expectations. I like to tell presbyopic patients who are good candidates for the procedure that they should not expect the lens to give them the reading vision of a 29-year- old. I explain, however, that the lens does provide a more natural, fuller range of vision than other modalities available to us. People who hear this in my practice seem to understand it, and, with the benefit of excellent biometry and careful surgery, our patients have been uniformly happy with their results.
 |
 |
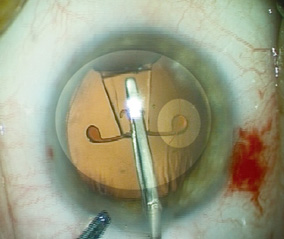
| Implanting the superior haptic. It's usually easier to get one loop "started" under the bag and then move the haptic sideways to implant the second loop. Don't release the trailing plate haptic until it and the loops are in the bag. | |
In my experience, the Crystalens is a better option than LASIK for the refractive management of the aging hyperope for three important reasons.
First, hyperopic LASIK in the older patient is often associated with tear-film problems, slow healing and slow visual stabilization. Crystalens patients do not experience an exacerbation of tear-film deficiencies and enjoy very rapid visual rehabilitation.
Second, hyperopic LASIK causes a decrease in contrast sensitivity in eyes with early cataract changes. The Crystalens tends to improve contrast sensitivity in these patients by eliminating the lens opacification.
Third, hyperopic LASIK simply does not solve the problem of presbyopia. Hyperopic LASIK in the aging presbyope can give better distance vision at the expense of good near vision or better near vision at the expense of good distance vision, but it can not give the presbyope what he or she really wants—good vision at distance and near without glasses. The Crystalens can deliver this.
Preoperative Evaluation
• Biometry and astigmatism management. Since Crystalens implantation is as much about crisp uncorrected postop vision as it is about removing a cataract, careful biometry is a critical ingredient for success (See "Immersion Rises to the Top" sidebar below). Patients can't appreciate the benefits of an accommodative IOL if they have a substantial postop error. It pays, therefore, to approach Crystalens surgery with the same appreciation for detail that we afford our keratorefractive surgery patients.
In keeping with this refractive surgery mindset, it's also important to perform preop corneal topography, something cataract surgeons may not be used to doing regularly. Keratometry is helpful for giving us the idea of the extent of the cylinder, but topography is important for quantifying and localizing it. You can then treat the cylinder during the surgery using limbal relaxing incisions
Topography also allows you to easily catch corneal pathology, such as pellucid marginal degeneration, that would contraindicate LRIs.
• Pupil measurement. Pupil size is also important. Patients with poorly dilating pupils aren't good candidates, because you need to see the margin of the capsulotomy very well during surgery in order to make sure you're placing the lens correctly in the capsular bag. Conversely, one should consider not using this lens in patients with widely dilating pupils. The Crystalens optic is 4.5 mm. This small optic might lead to problems with glare and halos at night in patients whose pupils dilate widely in low levels of illumination.
Tips for Surgery
When you've chosen a good candidate, here are tips to make sure his implantation goes well.
If there's some preop cylinder, always work on the steep axis of the cornea. If there is none, a temporal incision is better, as it is less likely to induce an astigmatic error. An ideal capsulotomy is between 4 and 5 mm. If you make the capsulotomy too small, it will be difficult to insert the proximal haptics. If the capsulotomy is very large, however, the lens may dislocate.
Also, I've implanted the lens with a wide range of viscoelastics, and I've come to the conclusion that it's more difficult to implant the Crystalens when using a highly retentive one. Since the lens is very flexible, a highly retentive viscoelastic tends to make the IOL curl up as you try to implant it.
If the patient has some astigmatism, you can use LRIs to treat it at the time of surgery. I use LRI nomograms, such as those of James Gills, MD, and Louis "Skip" Nichamin, MD.
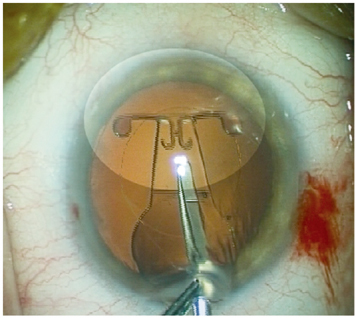
After a normal phaco, widen the incision to 3.5 mm. When removing the lens from its case, grasp it along its length with a smooth implantation forceps, making sure the hinge groove is facing up.
When you're implanting the lens, hold it as you place the distal haptics in the bag. Then, as you release the forceps you're using to place the lens in the eye, be sure to hold the lens with your left hand to make sure it doesn't come back out of the incision.
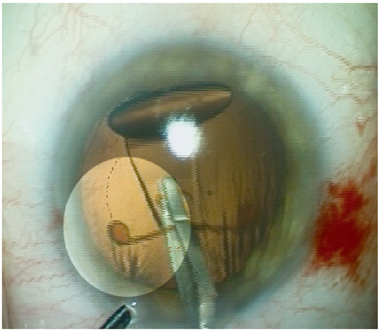
Once the trailing haptic and the loops are in the bag, you can release the lens and remove the implant forceps. As the haptics return to their normal shape, the lens will begin to center itself. You must be absolutely sure that you get both haptics in the capsular bag if you want the lens to work well. There is no data about implanting a Crystalens in the sulcus; if you can't get it in the bag, I would not implant it. Use an irrigation/aspiration tip to center the lens and remove excess viscoelastic from behind it. The haptics should be covered as much as possible by the anterior capsule, and the lens should vault posteriorly.
After you've filled the chamber, sealed the incision and instilled the postop drops, wait several minutes and administer a drop of Atropine 1%. The Atropine relaxes the ciliary body and lets the lens position itself more posteriorly, fitting snugly against the capsular bag. Make sure not to aggressively hyperinflate the anterior chamber, however, as this can cause the lens to move too far posteriorly and encapsulate there, resulting in postoperative hyperopia.
| The Synchrony Springs into the Spotlight |
 |
| The Visiogen company is developing its own accommodative intraocular lens, the Synchrony, which uses a novel concept: two optics instead of one. Stephen McLeod, MD, vice chair of ophthalmology at the University of California-San Francisco and a Visiogen consultant, explains the reasoning behind the lens. "It's a dual-optic system, with a plus-powered lens in the front and a minus powered lens in the back," he says. "The front and back lenses are joined by spring haptics. When the two lenses are close together, the eye should be set for distance. Then, as the ciliary body contracts, this takes tension off of the zonules, the capsular bag relaxes and the lenses are allowed to spring apart." This springing apart moves the front lens forward, changing the eye's focus to near. He says the natural tone of the capsular bag keeps the lenses together, storing energy in the spring that "wants to push the lenses apart." Currently, the front lenses in the Synchrony are in the 30-35 D range and the back ones are from -8 to -12 D. The front optic is 5.5 mm in diameter and the back is 6 mm. Los Angeles surgeon and Visiogen consultant Samuel Masket says, "The concept is very promising, but our experience is also very preliminary. There's been maybe 20 implants worldwide, though we gain experience with each passing series." Dr. Masket says that, for the Synchrony as well as the entire new industry of accommodative lenses, there are certain concerns that will have to be addressed. "For all the lenses that provide accommodation, either the optic has to move or it has to gain strength," he says. "All are dynamic, and depend upon the maintenance of a flexible capsular bag; we'll have to reduce the presence of equatorial lens epithelial cells, or limit their activity, so we'll have better optical performance. And, [with the Synchrony] you have two optical components in the bag, so if they're not in contact there is a concern about interlenticular opacification. But we haven't seen that yet. There's also the concern that the bag could become fibrotic from normal lens changes." Salt Lake City surgeon Nick Mamalis has implanted the lens in cadaver eyes, and says another challenge will be putting it in as small an incision as possible. "Forceps require a somewhat larger incision, so the company is working on an injector system to allow it to go through a reasonably sized incision," he says. "After having worked with both systems, I think the injector will eventually be the way to go." Dr. Masket sees other aspects that need ironing out, as well. "We've demonstrated the concept to be valid," he says. "Now it's a matter of working out the optical formulas in order to be more accurate with power calculations." |
• Day one postop. On the first postop day, make sure the lens is centered properly. If the lens is decentered, a haptic is out of the bag or there's a problem with the capsule, reposition it as soon as possible. If the lens is still decentered, remove it and place a monofocal IOL. If you need to exchange the Crystalens to implant one with a more accurate power, it's best to do so within three weeks.
Though the postop Atropine will impede accommodation, you can gauge the success of the procedure by testing the uncorrected distance acuity. If the patient can see clearly at distance uncorrected and the eye is nearly emmetropic, then the patient will be happy.
If, however, the patient has trouble seeing at distance, intermediate and near, careful evaluation is necessary. If there is a significant residual refractive error, you may need to exchange the Crystalens for a more appropriate power. The Crystalens becomes very well fixed to the capsular bag in a matter of weeks. If an IOL exchange seems indicated, it is better to proceed sooner rather than later.
If the patient is myopic postop, determine the degree of myopia and how the patient perceives his acuity. Some patients can tolerate monovision, but enhancements via lens exchange, LASIK or LASEK may be necessary.
Though I wouldn't recommend piggybacking maneuvers in addition to the Crystalens for the beginning surgeon, a surgeon in our trial placed a lens in a patient's sulcus over a Crystalens with an excellent result.
Routinely, before the patient leaves the first-day visit, we instill another drop of Atropine, and suggest over-the-counter reading glasses for use until the Atropine wears off. After the agent's effect is gone, it's important that the patient try to read as much as possible without glasses. The data suggest that near vision will continue to improve over time in patients who "work" at restoring their accommodation. Schedule a follow-up exam for two to four weeks.
• One month postop. At this visit, when testing the patient's vision, it's informative to measure accommodative amplitude through the patient's distance correction. I like to ask patients if they are wearing any glasses for distance or near. Most patients report that they don't wear, or rarely wear, glasses during the day. In some instances, patients state that they only wear reading glasses for very fine print or at night.
If your patient tells you that he wears glasses for distance or for reading some or most of the time, determine if they're truly necessary and if he's happy with the situation. If he is, you don't have to do anything other than to prescribe the appropriate correction. A number of patients like to wear magnifiers for very small print or night-driving glasses and are very happy with this.
If the patient is unhappy, determine when and why he wears his glasses. If uncorrected near vision is the problem and his spherical equivalent is over 0.5 D, perform a cyclopleged refraction and consider enhancement with LASIK or incisional astigmatic correction. If the spherical equivalent is within ± 0.5 D of plano, rule out other ocular pathology, such as cystoid macular edema. If there's no pathology evident, the patient may not be trying to read without glasses and hasn't developed his accommodative potential. You have to remember that, on average, these are patients who haven't accommodated in 20 years. Some patients may need to be weaned off glasses and encouraged to read.
Results
In a study of bilaterally implanted subjects with an average age of 69, at one year 98 percent saw 20/40 or better at distance, 100 percent saw 20/40 or better at intermediate ranges and 98 percent could read 6-point type without glasses. Ninety-four percent of these patients said they could perform most of their daily activities without glasses.
The effect appears to last over time, as well. At two to three years, patients are performing as well as they did initially. And, in Mexico, Arturo Chayet, MD, has 14 Crystalens patients who are four years postop. Seventy percent of Dr. Chayet's patients see 20/30 or better uncorrected at distance and J3 or better at near.
| Immersion Rises to the Top |
| According to Crystalens' maker Eyeonics, errors in biometry account for around half of all postop surprises after cataract surgery, and A-scan measurement is typically the one most prone to operator error. Because the Crystalens' accommodative powers rely on a crisp refraction postop, its maker recommends surgeons use immersion A-scan or the IOLMaster (Zeiss) rather than applanation, which can introduce operator error through the need for applanation of the cornea. Applanation can lead to errors from a variety of sources: the amount of pressure the A-scan operator uses on the eye, the level of patient cooperation, the cataract's density and axial alignment errors. The company says immersion biometry eliminates compression errors, minimizes axial alignment errors, and provides multiple and consistent readings. Though many fear that immersion A-scan takes much longer than applanation, experts say that, with experience, the time difference is negligible. The following companies offer immersion A-scan systems: Alcon: 1 (800) TO-ALCON Accutome: 1 (800) 979-2020 Innovative Imaging Incorporated: 1 (800) 765-7226 Quantel Medical: 1 (888) 660-6726 |
Though the lens uses a 4.5-mm optic, my patients have not complained of visual aberrations. We performed a sub-study comparing Crystalens patients to standard monofocal IOL patients and found no difference in contrast sensitivity under mesopic conditions with or without glare. Subjectively, through questionnaires, Crystalens patients were no more likely to complain of glare and halos or aberrations at night than standard monofocal patients. Younger patients than those in our series, however, or patients whose pupils dilate widely, might do less well, especially in low light.
The lens has had a very solid safety profile. Out of 450 patients in each phase of the study, there were two cases of repositionings. One was due to a non-intact capsulorhexis and the other occurred in a patient with a small pupil in whom one of the haptics was positioned outside of the bag. There were no lens-related complications, and YAG capsulotomy doesn't appear to negatively affect lens function.
There is an understandable amount of skepticism about the Crystalens. This seems appropriate, since this is an entirely new technology. Many of my colleagues ask me if it really works. I can say simply that, in my experience, it works very well. The Crystalens does not give a 69-year-old the accommodative function of a 29-year-old, but I believe that it is the best option we have today for the surgical correction of presbyopia. If you select good surgical candidates, take care to give patients realistic expectations, and approach this procedure with the same level of care and attention to detail that you afford to your keratorefractive patients, you should be pleased.
Dr. Colvard is an assistant clinical professor at the University of Southern California School of Medicine, and serves as a consultant to Eyeonics.



