SUTURES REPRESENT THE TRADITIONAL MEANS OF CLOSING ophthalmic wounds, but they have some significant disadvantages. Suturing a corneal laceration inflicts trauma to the cornea just from the multiple needle passes. Sutured wounds typically result in astigmatism and uneven healing. Additionally, sutures are a potential nidus for infection, and they can incite inflammation and neovascularization in the cornea, which can ultimately result in corneal scarring. Suturing also requires additional operating time and technical skill. Finally, prompt removal of sutures is necessary, particularly those made of monofilament nylon material, to avoid the risks of suture abscess and neovascularization.
In this article, my coauthors and I will review the inherent challenges and the progress in the efforts to develop an adhesive that may represent a better alternative to sutures, whether in long-standing products such as cyanoacrylate, or more recent options, some new to the market and others still under investigation.
Disadvantages of Adhesives
Some of the adhesives that are currently used in ophthalmology are also not ideal. Cyanoacrylate has been used on the eye for the past 40 years off-label, but it is difficult to apply. When cyanoacrylate contacts any moist surface, it immediately polymerizes, and after it does, it becomes stiff, abrasive and opaque. For these reasons, cyanoacrylate adhesive is poorly tolerated, and patients often require placement of a bandage contact lens to blink comfortably and to retain the adhesive on the eye. Additionally, the by-products of cyanoacrylate glue, notably formaldehyde and cyanide, have been shown to be toxic to the lens and retina.
While Tisseel (Baxter Corp. Mississauga, Ontario) may be suitable for conjunctival autografts and for LASIK flap complications, it is also not ideal. The preparation process for Tisseel is time-consuming, and there is the theoretical risk of transmitting viral infection because of its human and bovine constituents. It is also expensive to use.
New Direction
We have recently attempted to find a sealant that is more ideally suited for ophthalmic use. The optimal ophthalmic sealant would have the following characteristics:
• Secure tissue in place
• Persist long enough to allow the incision to heal
• Promote the natural healing mechanism
• Degrade as tissue is regenerated
• Act locally and safely
• Induce minimal astigmatism
• Provide microbial barrier to infection
• Be transparent
• Have elastic mechanical properties
• Have optimal rheological properties for delivery
• Have favorable solute diffusion properties
My colleagues and I have been synthesizing and studying a new class of adhesives called biodendrimers for use on the eye. We are currently conducting experimental studies in human cadaver and animal eyes; no human applications have been performed yet.
The molecular structure of biodendrimers is much different from that of cyanoacrylate. Biodendrimers have a tree-like structure that branches out at various points. All of its components are natural metabolites that are synthetically made in the laboratory and are biocompatible and biodegradable.
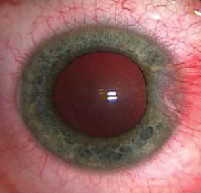
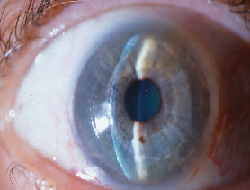
 |
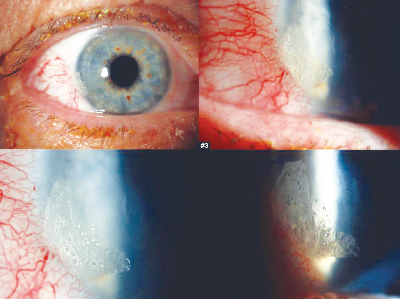
| Clockwise from upper left, these images show a loose flap, application of the biodendrimer sealant, activation and adherence. |
We have now moved to a self-gelling system, in which two chemical components are simply mixed together to form the gel. The self-gelling system is preferred because it will not require argon laser or other light for polymerization.
Recent studies have shown that both the laser-activated system and the self-gelling system have higher leaking pressures than sutures in both linear wounds and stellate corneal wounds.1
Additionally, we have used optical coherence tomography technology with real-time imaging to analyze the adhesive on a full-thickness clear corneal wound during fluctuation of intraocular pressure. We found that the corneal wound gaped and opened when the IOP was lowered and occasionally when it was raised. However, the adhesive was able to stay intact on the eye during these conditions. These observations demonstrated the strong adhesion and flexibility of the biodendrimer adhesive in an ex vivo setting and provided evidence that an adhesive may be an ideal alternative for sealing corneal wounds.
LASIK Application
We have also used both the self-gelling glue and the laser-activated glue to seal LASIK flaps. We created LASIK flaps in 10 human eye-bank eyes. In one group, we used the laser-activated glue, and in the other group, we used the self-gelling glue. We tested the adherence of the flap both before and after the application of adhesive. This study confirmed that the adhesive was effective in sealing the flaps and supported the role that adhesives could play in treating various LASIK flap complications, such as epithelial ingrowth and flap dislocations.2
Other practical advantages of a biodendrimer adhesive include its easy application process, quick polymerization time (within 30 seconds), smooth texture and transparency.
Dr. Kim is an associate professor of ophthalmology and the associate director of the Cornea and Refractive Surgery Service at Duke University Eye Center, Durham, N.C. Contact him at (919) 681-3568 or kim00006@mc.duke.edu. His studies on biodendrimers are funded by a grant from the NIH/NEI, the Pew Foundation, and Johnson & Johnson Focused Giving Program. He is a consultant for Hyperbranch Medical Technology Inc.
2. Kang PC, Carnahan MA, Grinstaff MW, Kim T. Novel tissue adhesives to secure laser in situ keratomileusis flaps. J Cataract Refract Surg 2005;31(6):1208-1212.
LASIK Flap Complications
David R. Hardten, MD, Minneapolis
EPITHELIAL INGROWTH IS A COMPLICATION OF LASIK SURGERY that occurs in 0.5 to 15 percent of cases, and it is usually observed in the first few weeks after surgery. It may be nonprogressive or progressive, and in its most advanced stage, it may result in flap melt.
Signs of epithelial ingrowth include isolated nests or sheets of cells, decreased uncorrected and/or best corrected visual acuity, induced astigmatism on refraction, and irregular astigmatism on topography.
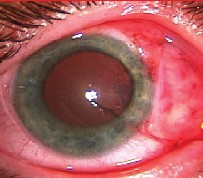
 |
| Isolated nests or sheets of cells are one common sign of epithelial ingrowth. |
Treatment of Epithelial Ingrowth
In some cases, the epithelium grows so much that the flap must be lifted and the epithelial ingrowth removed. Epithelial ingrowth can be removed using a blunt spatula and a Merocel sponge. However, it is often a recurrent problem, and the treatment success rate decreases with multiple manipulations.
To prevent recurrence of epithelial ingrowth, flap adherence must be ensured. This can be accomplished by suturing the flap edges, but sutures can induce striae and irregular astigmatism, and suture removal is required.
Using Tisseel may be a better alternative for some patients. Tisseel fibrin glue is a mixture of fibrinogen and thrombin. It also has a bovine fibrinolysis inhibitor, and it is mixed at the tip of a duplojet syringe. The surgeon typically has 30 to 60 seconds to manipulate the adhesive before it completely sets, but the thrombin can be diluted with saline (without calcium) to further slow the setting time. Tisseel takes eight to 10 minutes to completely dry, and I prefer to wait for it to be relatively dry before placing a bandage soft contact lens. The Tisseel dissolves in one to three weeks.
 |
 |
| Epithelial ingrowth following LASIK can be a recurrent problem. | Tisseel glue, postop day one, following radial keratotomy and LASIK. |
Epithelial Ingrowth Removal
With my current technique, I use topical proparacaine and a closed bladed speculum to isolate the lashes. The epithelium is removed from the top of the flap and along the gutter (the border between the flap and the peripheral bed) for 2 mm on either side of the gutter. I then lift the flap and remove the epithelium from the stromal bed and from the back of the flap, taking care to remove all epithelium, especially from the edge of the flap and the gutter where it is especially adherent.
I apply 70% alcohol to soften up the epithelium in the stromal bed and on the back of the flap because these are the most difficult areas from which to remove epithelium. It is important to take care that a small amount of the alcohol is placed on the cornea to prevent spilling on the conjunctival stem cells. The alcohol is also not left in place for a long period of time to reduce the possibility of endothelial damage. Then, the gutter and edge of the flap are scraped again with a blunt PRK spatula. Sharp dissection is avoided.
Then, I lay the flap back down and let it dry into place, making sure that it adheres securely. I then apply the Tisseel glue to the gutter. Preparation of the glue can be difficult, and the manufacturer's instructions should be followed carefully. The thrombin portion can be diluted by 50 percent with balanced salt solution without calcium to enable a slower setting time to allow manipulation of the glue, if desired. With practice, this may not be necessary. It is also important when using the duplojet syringe to make certain that there are no air bubbles in the syringe that might prevent proper mixing of the solutions. Air bubbles tend to prevent the fibrin portion from being expressed from the syringe. Alternatively, the glue can be mixed in a contact lens case and then painted on the eye, or the glue components can be applied to and mixed on the cornea.
The Tisseel glue is used to fill the space in the gutter, blocking epithelium from growing in the gutter until the flap has scarred into place. This allows 360-degree adherence without the use of sutures or the skip areas between sutures.
Results
Of the 21 eyes in which I have used this technique, 13 eyes had no evidence of recurrent epithelial ingrowth, six eyes had small nests of epithelial cells at the flap edge that to date have not required removal, and two eyes had significant recurrence. One was due to inadequate application of the fibrin portion of the glue. There were no recurrences after a second surgery in either of these eyes. This procedure has a better success rate in my experience than lifting the flap and removing the epithelial ingrowth alone.
The only disadvantages to using Tisseel are that it is more time consuming and expensive than simply removing the epithelial ingrowth, and it is somewhat difficult to learn the mixing technique. The surgeon must make sure that the two components are mixed on the surface of the eye to allow proper setting of the adhesive.
Another downside is that vision recovery is fairly slow because the glue has a hazy appearance until it dissolves, which takes a few weeks. Postoperatively, I use frequent lubrication, a bandage soft contact lens for two to three weeks, steroid four times daily for four weeks, then twice daily for four weeks, a fourth-generation fluoroquinolone four times daily for two to three weeks, and frequent lubrication. Nonsteroidal drops are helpful for discomfort for the first few days. The patients are given an oral narcotic for three to four days. This technique is a useful rescue for patients with recurrent epithelial ingrowth.
Dr. Hardten is in private practice in Minneapolis, Minn., and is an associate professor of ophthalmology at the University of Minnesota, Department of Ophthalmology. Contact him at (612) 813-3631 or drhardten@mneye.com. He has no financial interest in any of the products or companies mentioned in this article.
Liquid Bandage Suceesfully Seals Clear Corneal Incisions
David C. Ritterband, MD, New York City
Recent studies in the literature have suggested that sutureless clear corneal cataract incisions may be associated with an increased risk of acute postoperative endophthalmitis, and researchers have expressed concern that the instability of sutureless clear corneal wounds may allow an early postoperative influx of extraocular fluid contaminated with ocular surface bacteria.1-4
These studies demonstrate the need for and the potential benefits of a safe, flexible, easy to use, and reliable barrier device to seal a corneal cataract wound. This device would serve as an adjunct to prevent the efflux of intraocular fluid out of the eye and to prevent the influx of potentially contaminated external ocular surface fluid.
The 2-octyl cyanoacrylate compound marketed commercially as Dermabond (Ethicon, Somerville, N.J.) has been used safely and successfully since 1998 in various medical treatments including blepharoplasty, facial skin closure, cleft lip repair, laparoscopic surgery, and in the treatment of gastric fundal varices.5-8 The 2-octyl cyanoacrylate compound is also marketed for consumer wound care as Liquid Bandage (Johnson & Johnson, Skillman, N.J.). The newer cyanoacrylate compounds, such as 2-octyl cyanoacrylate, are inexpensive, can be easily applied, and can create a "watertight" seal that is much more pliable and tissue compatible than its predecessors. Cyanoacrylate-based compounds have been used safely and effectively in ophthalmology since 1968, mostly to seal corneal perforations, despite never being approved by the Food and Drug Administration for this purpose. Prior to its use in the eye, my colleagues and I performed a laboratory study model demonstrating the efficacy of Liquid Bandage in preventing influx of extraocular fluid through a clear corneal wound despite fluctuations in intraocular pressure and manual manipulation of the wound.
Liquid Bandage in the Eye
Our study, presented at ASCRS this year, included 51 eyes of 51 patients undergoing temporal, clear corneal cataract surgery. In each eye, a 2.75-mm standard clear corneal tri-planar wound was made, which was followed by standard phacoemulsification and cortical removal. An acrylic IOL was injected without enlarging the wound. After implantation of the lens, the wound was dried, and the commercial Liquid Bandage product was applied to create a sealed barrier across the wound.
At the first postoperative visit, we evaluated wound integrity, presence of tissue adhesive and patient symptoms. Forty-five of the 51 eyes had adhesive present, two had partial adhesive present, and four had no adhesive present on the first postoperative day. Additionally, 31 patients complained of foreign-body sensation, two complained of tearing, and one complained of photophobia. While many patients complained of foreign-body sensation, most felt it was minor. The reported incidence of foreign-body sensation was no greater than is generally reported after standard cataract surgery without the use of an adhesive.
In addition, 25 patients experienced diffuse mild conjunctival injection, and five experienced focal temporal conjunctival injection.
By the second postoperative visit, the majority of patients were symptom-free. Six of 51 patients still complained of mild, transient foreign body sensation. Two of the six patients had remnants of the barrier device present, two had fully epithelialized wounds, and two had punctate epithelial staining along the wound. The physical presence of the barrier device appears to be one of several causes of foreign-body sensation after cataract surgery.
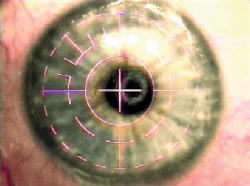
 |
| Focal conjunctival injection on postop day one in a minority of cases receiving the Liquid Bandage after cataract surgery. By the second visit, most patients were symptom-free. |
There appeared to be no problems with wound healing. There were no wound leaks at any visit. Thirty-six of 51 eyes had complete epithelialization by their second postoperative visit (five to seven days). Of the remaining 15 patients, nine still had remnants of glue on their wound edge, blocking fluorescein uptake, and the other six had either a small linear area of fluorescein staining or punctate staining along the wound edge.
Liquid Bandage worked well. It adhered quickly and easily, and it generally dissolved in five to seven days. Additionally, it is inexpensive. One bottle of Liquid Bandage contains approximately 48 drops, and it costs $8.99 at our local pharmacy. Each eye only requires two to three drops, so the price averages between $0.40 and $0.50 per eye.
A future additional benefit may be that the glue can be chemically modified. For example, one advance would be to bond antibiotics to it. The antibiotics would be covalently bonded to the adhesive and painted on with the adhesive and would then leach into the eye.
Our study demonstrated the ease, applicability, and low side-effect profile of Liquid Bandage as a temporary wound barrier and sealant in clear corneal cataract surgery. Its use may help to reverse the recent trend of increased postoperative endophthalmitis associated with clear corneal wounds, and improvements and experience with application techniques will likely improve the mild side effects. Continued study will elucidate the full utility of Liquid Bandage or other related adhesives as an ophthalmic surgical tool.
Dr. Ritterband is a clinical associate professor of ophthalmology and assistant director of Cornea and External Disease at the New York Eye and Ear Infirmary in New York City. Contact him at (212) 505-6550 or ritterband@msn.com. He has no financial interest in any of the products or companies mentioned in this article.
1. Lertsumitikul S, Myers PC, O'Rourke MT, et al. Endophthalmitis in the western Sydney region: a case-control study. Clin Exp Ophthalmol 2001; 29:4000-4005.
2. Cooper BA, Holekamp NM, Bohigan G, et al. Case-control study of endophthalmitis after cataract surgery comparing scleral tunnel and clear corneal wounds. Am J Ophthalmol 2003;136:300-305.
3. Nagaki Y, Hayasaka S, Kadoi C, et al. Bacterial endophthalmitis after small-incision cataract surgery. Effect of incision placement and intraocular lens type. J Cataract Refract Surg 2003:29:20-26.
4. McDonnell P, Taban M, Sarayba M, et al. Dynamic morphology of clear corneal cataract incisions. Ophthalmol 2003;110:2342-2348.
5. Ritterband DC, Meskin SW, Shapiro DE, et al. Liquid Bandage tissue adhesive (2-octylcyanoacrylate) in sealing clear corneal wounds: A laboratory model. In press.
6. Taravella MJ, Chang CD. 2-octylcyanoacrylate medical adhesive in treatment of a corneal perforation. Cornea 2001;20(2):220-221.
7. Webster RG, Slansky HH, Refojo MF, et al. The use of adhesive for the closure of corneal perforations. Arch Ophthalmol 1968;80:705-709.
8. Singer AJ, Thode JC Jr. A review of the literature on octylcyanoacrylate tissue adhesive. Am J Surg 2004;187(2):238-248.
Suterless Conjunctival Autograft
Sadeer B. Hannush, MD, Philadelphia
PTERYGIUM SURGERY HAS BEEN AROUND FOR MILLENNIA, AND there are more than 100 published techniques for removing pterygia. Whenever there are this many techniques, it usually means that no single one is decidedly superior to all others.
One shortcoming of many of the techniques is that they do not prevent recurrence of the pterygium. Cornea specialists currently prefer two techniques to prevent recurrence: using intraoperative mitomycin or performing a conjunctival or amniotic membrane graft. On the Cornea Service at Wills Eye Hospital, we prefer conjunctival transplantation, whenever possible, over intraoperative mitomycin at least for primary pterygia.
Sutures Not Ideal
Historically, we have sutured these conjunctival autografts in place with 10-0 nylon or 9-0 or 10-0 Vicryl. Suture use is not ideal, however, and both nylon and Vicryl have downsides. Vicryl sutures may be inflammatory, but they dissolve, making suture removal unnecessary. Nylon sutures must be removed by the surgeon.
The biggest problem with sutures is patient discomfort. Suture ends rub on the tarsal conjunctiva. I have tried burying the knots and placing a large bandage contact lens over the sutures, but nothing has worked well.
A study conducted by Gabor Koranyi, MD, found that using tissue fibrin sealant (an organic glue) instead of sutures for securing a conjunctival transplant during pterygium surgery shortens surgical time significantly and is associated with less postoperative discomfort.1
Tisseel VH
In his study, Dr. Koranyi used Tisseel VH. It is a fibrin tissue adhesive, and its components include a sealer protein (human fibrinogen from pooled plasma), fibrinolysis inhibitor solution (bovine), thrombin (human), and calcium chloride.
Tisseel VH mimics the body's own response to injury by creating a coagulum, or clot, that makes the tissues adhere to each other. It forms this solid coagulum within three to five minutes of delivery, and 70 percent of its ultimate strength is attained in the first 10 minutes. Full strength is reached in about two hours.
Tisseel is approved in the United States, but its use in ophthalmology is off-label. I began using Tisseel VH in January 2003, and I have now used it in approximately 60 cases with good results.
The advantages of Tisseel VH over sutures include: less inflammation; faster surface rehabilitation; and patient comfort.
The main disadvantage is the hypothetical risk of viral or prion disease transmission. Prion disease transmission is hypothetically possible because of the bovine component in Tisseel VH. In more than 12 million uses worldwide, there has never been a report of transmission of bovine spongiform encephalopathy (mad cow disease). This is principally attributed to the source of bovine fibrinolysis inhibitor solution being countries in which no case of mad cow disease has ever been reported.
It is also possible to transmit hepatitis B, hepatitis C, and HIV, but there have been no reports of this either. The only reports of viral transmission were of human parvovirus before 1999, when PCR was added to the battery of tests for the evaluation of the donor pool.
The other disadvantage is cost. While one pack of sutures costs between $20 and $35, 1 mL of Tisseel VH costs $80. However, while Tisseel VH costs more, it also reduces OR time significantly (and time is money). In fact, Tisseel VH has cut in half the amount of time we allow for this procedure. Moreover, each vial of product may be used for more than one procedure on the same day.
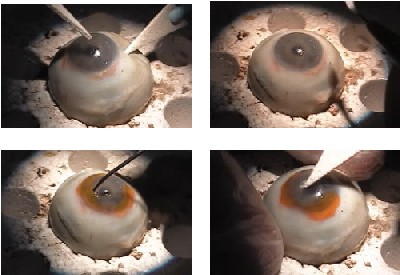
|
|
 |
 |
| Sutureless conjunctival autograft from preop (top) to immediate and late postop. |
Dr. Hannush is an attending surgeon at the Cornea Service at Wills Eye Hospital and assistant professor of ophthalmology at Jefferson Medical College in Philadelphia. Contact him (215) 752-8564 or sbhannush@comcast.net. He has no financial interest in any of the products or companies mentioned in this article.
Traditional Cyanoacrylate
Christopher J. Rapuano, MD, Philadelphia
TRADITIONALLY, CYANOACRYLATE HAS BEEN USED FOR STERILE corneal melts and perforations. Theoretically, the glue is applied, the cornea heals under the glue, and the healed cornea pushes the glue out. Then, the cornea is completely intact with some scarring. The best candidates are eyes with divots or craters as opposed to eyes with protruding areas of ulceration, as the glue adheres much better in indentations and tends to fall off too quickly when protrusions are treated.
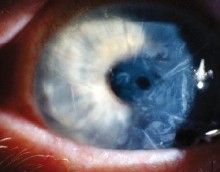
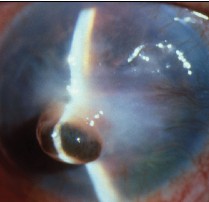 |
| Sutureless conjunctival autograft from preop (top) to immediate and late postop. |
Application Techniques
There are several techniques for applying it. It is important to put on enough glue to seal the hole, but not so much glue that it forms a large mound. If too much glue is applied, it must be removed. However, removing the glue is difficult, and other tissue can be removed in the process, causing significant
My preferred technique is to use a tiny plastic pipette applicator. A small amount is sucked up into the pipette, and small drops are applied into the hole. Once the cyanoacrylate polymerizes, a contact lens is placed on top of it. Then, I usually have the patient wait for 30 minutes in the office to make sure that the cyanoacrylate is staying on and that the anterior chamber is forming.
One problem with cyanoacrylate is that it occasionally does not come off by itself. In these cases, the surgeon can try to pull it off at the slit lamp, but this is not ideal because the hole can be re-created. Another option is to leave the glue on and hope that it will come off on its own. However, if it is in the center of the cornea, leaving it on can prolong patients' visual impairment.
Uses
Although some people believe that cyanoacrylate has an antibiotic effect, I think it can impede the delivery of antibiotics to an infection, so I don't think it's a great choice for use with active infections.
With a corneal laceration that cannot be closed with sutures alone, some ophthalmologists will put glue on top of the sutures to seal the laceration. The problem is that it is then difficult to remove the glue after it adheres to the stitches. A glue that dissolves on its own in a few weeks would be a much better choice for application over sutures.
Not Ideal
While cyanoacrylate has been a standard of care for certain types of ulcers and perforations for many years, it certainly is not perfect. For lacerations, it would be better to have a glue that could be applied in the absence of stitches. This might improve scarring.
 |
| One problem with cyanoacrylate is that it occasionally does not come off by itself. |
Dr. Rapuano is in practice at Wills Eye Hospital in Philadelphia. Contact him at (215) 928-3180 or cjrapuano@willseye.org. He has no financial interest in any of the products or companies mentioned in this article.
Anterior Lamellar Transplants
Herbert E. Kaufman, MD, New Orleans
CYANOACRYLATES ARE STRONG AND HAVE BEEN PROVEN effective. These types of glue have terrific tensile strength. However, in the eye, they act like a piece of plastic. Cyanoacrylates do not allow fluid or nutrients to pass back and forth. Additionally, they do not allow the tissue underneath them to heal. As more tissue is made and sloughs off, the glue's bond is broken.
Cyanoacrylates work well on the surface of the eye. They can be used to seal perforations and to close corneal wounds, but they do not work well inside the tissue. The cornea receives its nutrition from the aqueous, and the aqueous has to percolate through the cornea. If that cannot occur because of a barrier, such as cyanoacrylate, the tissue farthest away from the aqueous will become necrotic.
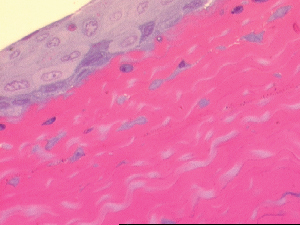 |
| Cornea with tissue glue 10 days postop. |
Flap Adherence
After LASIK, the flap adheres to the stromal bed because the endothelium is pumping fluid to pull everything together. Equally important, the epithelium is impermeable to fluid, so nothing can come in.
With lamellar transplants, however, the epithelium is often damaged. In these cases, the surgeon cuts a free flap that is approximately half the thickness of the cornea. After removing this damaged part of the cornea, a matching free flap is removed from a donor and transplanted onto the patient's eye.
The flap must then be held in place until the surface layer grows over and the endothelial pump suctions them together. A small amount of fibrin glue is placed on the base. The donor cap is applied and pressed on with a Paton spatula, and a bandage contact lens is placed for a week. As the tissue heals, the body dissolves the glue.
 |
| Superficial scar 200-µm free cap with ACS Tisseel adhesive and soft contact lenses. |
Tisseel is also effective in other types of ophthalmic surgery, such as LASIK, especially when flap lifts are necessary or epithelial ingrowth occurs. In cataract surgery, it can be used in any uncertain wounds, and it works well in pterygium removal to fixate a conjunctival or amnion graft without sutures. It also can be used during glaucoma surgery for conjunctival flaps, and it works well on skin flaps.
Dr. Kaufman is the Boyd Professor of Ophthalmology and Pharmacology and Experimental Therapeutics at Louisiana State University. He can be reached at (504) 412-1200 or hkaufm@lsuhsc.edu. He has no financial interest in any of the products or companies mentioned in this article.