The Aspheric Advantage
 |
| The AcrySof IQ lens by Alcon. |
| Optic/Haptic Material ACRYSOF with UV and blue light-filtering chromophores |
The main advantage of aspheric IOLs compared with traditional spherical IOLs is improved contrast sensitivity and functional vision. In young patients who have optimal vision, the cornea's positive spherical aberration is balanced by the negative spherical aberration in the crystalline lens. "As we get older, our lens gets thicker and rounder and becomes more positively aberrated. The result is image quality deterioration," explains Robert M. Kershner, MD, director of Eye Laser Consulting, Boston, and clinical professor of ophthalmology, John A. Moran Eye Center, University of Utah School of Medicine, Salt Lake City.
While the purpose of IOLs is to replace the crystalline lens, spherical IOLs have positive spherical aberration, so rather than balancing the positive spherical aberration of the cornea, they add to it. Like the youthful human crystalline lens, aspheric IOLs can induce negative spherical aberration, which balances the cornea's spherical aberration and improves visual performance.
To determine whether aspheric IOLs would provide better retinal image contrast and functional visual performance than conventional silicone and acrylic IOLs, Dr. Kershner prospectively studied 221 eyes of 156 patients.1 These eyes were randomly assigned to receive one of three IOLs: the Tecnis Z9000 (Advanced Medical Optics), the AA4207VF (Staar Surgical Co.), and the AcrySof SA60AT (Alcon).
Visual acuity was measured preoperatively and at one day, one and three weeks, and one, three and six months postoperatively. Additionally, fundus photography and photopic and mesopic functional acuity contrast testing were performed preoperatively and three months postoperatively.
"What we found was nothing short of amazing. This study showed that the Tecnis lens improved contrast perception by 38.5 percent during the day and by 100 percent at night. This means that seniors were seeing at night with the same image quality and contrast perception as an 18-year-old during the day. I immediately stopped using every other lens and switched to the Tecnis lens. To date, approximately 30 studies have corroborated these results," he says.
Additionally, an aspheric lens has been shown to provide patients with increased functional vision in night driving conditions compared with a traditional spherical IOL.2
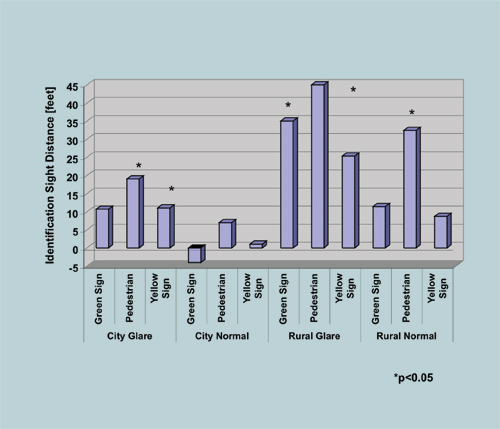
In a randomized, double-masked study, 29 patients were implanted with the Tecnis IOL in one eye and the AcrySof SA60AT spherical IOL in the fellow eye. All testing was conducted with best-corrected visual acuity using one eye at a time in each testing condition. Both city and rural night driving conditions, with and without glare, were tested, and patients were asked to identify a directional sign, a warning sign, and a pedestrian. "The eye implanted with the aspheric lens outperformed the eye implanted with the spherical lens in 21 of 24 testing conditions, and the difference was statistically significant in 10 conditions," says Mark Packer, MD, who served as coordinating investigator of the study. Dr. Packer is assistant clinical professor, Oregon Health and Sciences University, and in private practice at Drs. Fine, Hoffman, and Packer in Eugene, Ore.
 |
| The Tecnis Z9000 by AMO. |
Three Aspheric IOL Choices
Three aspheric IOLs are currently FDA approved: the SofPort LI61AO (Bausch & Lomb), the AcrySof IQ (Alcon Laboratories, Inc.), and the Tecnis Z9000 (Advanced Medical Optics, Inc.). All three lenses have different strategies for compensating for spherical aberration.
The SofPort lens is a multi-piece lens made of third-generation silicone. It has a refractive index of 1.43, and it introduces no spherical aberration to the eye.
The AcrySof IQ is a single-piece lens made of hydrophobic acrylic, and it has a refractive index of 1.55. It adds 0.20 µm of negative spherical aberration to the eye.
The Tecnis Z9000 is a multi-piece lens. It is available in both second-generation silicone and acrylic. The silicone IOL has a refractive index of 1.46, and the acrylic lens has a refractive index of 1.47. It introduces 0.27 µm of negative spherical aberration to the eye.
Choosing a Lens
Surgeons also have different strategies for compensating for spherical aberration. Some surgeons correct all patients using the average spherical aberration of the cornea, which is +0.27 µm. The theory is that counteracting this amount of spherical aberration will provide the vast majority of people with good functional vision.
Other surgeons are attempting to customize lens choice to each particular patient, because not all patients have an "average" spherical aberration. "If outcomes are measured in terms of an entire group of patients, then aspheric lenses produce much better outcomes. However, we need to determine what is best for each individual patient, rather than patients as a group," Dr. Packer says.
Skip Nichamin, MD, agrees, noting that while it is not yet standard practice, "the best way to choose an aspheric IOL for a particular patient is to measure the patient's preoperative corneal spherical aberration." Dr. Nichamin is the medical director of the Laurel Eye Clinic, Brookville, Pa.
For example, a patient with +0.27 µm of corneal spherical aberration may be a good candidate for the Tecnis lens, while patients with very little spherical aberration may do better with the SofPort AO lens. The AcrySof IQ lens could be considered for some patients who fall somewhere in between.
It may also be important to target a postoperative spherical aberration, and the ideal target may be +0.1 µm. A study of naval pilots found that, in addition to better-than-average visual acuity, they also have better-than-average contrast sensitivity when compared to non-aviation controls, and these pilots have a slightly positive spherical aberration.3
To determine whether patients targeted for a postoperative spherical aberration of +0.1 µm would have better outcomes than patients who were not targeted, George H. Beiko, BMBCh, conducted a prospective study. Twenty patients with a corneal spherical aberration of +0.37 µm were implanted with the Tecnis lens, targeting a postoperative spherical aberration of +0.10 µm.4 Another 20 patients were implanted with the Tecnis lens, but a postoperative spherical aberration was not targeted. Contrast sensitivity and visual acuity were compared between the groups. Patients' corneal-derived spherical aberration was measured using the Oculus Easygraph topographic system, and contrast sensitivity was measured with the Stereo Optical VT 1600X.
Dr. Beiko found that the group targeted for a postoperative spherical aberration of +0.10 µm outperformed the non-selected patients at almost every spatial frequency tested under photopic and mesopic conditions.
The AcrySof IQ lens is designed to bring the average population to a postoperative spherical aberration of +0.10 µm. "So, I implanted the AcrySof IQ lens into some nonselected patients. These patients outperformed the nonselected Tecnis patients. However, when I compared them to the Tecnis patients who were targeted for +0.10 µm, they performed equally well. Achieving good outcomes seems to be tied to this one value, not to one particular lens," says Dr. Beiko, in private practice in St. Catharine's, Ontario, Canada.
Dr. Packer notes that surgeons must also consider that the preoperative cornea is not always identical to the postoperative cornea. Higher-order aberrations in the cornea can be induced during surgery. Specifically, coma can be induced by the incision. "For some reason, in some surgeons' hands, the cornea changes in spherical aberration as well as coma, and the change is not always predictable. So, it is important for surgeons to know whether they are routinely inducing spherical aberration during surgery," he says.
While customization is not always straightforward, it may be the future of cataract surgery. "Customization is the direction in which we are headed, and practices that are providing this may have a marketing advantage," Dr. Packer says. Dr. Nichamin agrees. "This is the beginning of a whole new era for us. We are where LASIK surgeons were a few years ago when custom ablation was introduced. Everyone is starting to think very carefully about quality of vision," he says.

Aspherics: Not for Everyone
While these lenses have many advantages over spherical IOLs, they are not the best lens choice for all patients. Additionally, some practices are using aspheric IOLs in most patients, while others are reserving them for the patients who will benefit most.
"The only role for a traditional IOL over an aspheric IOL is in patients who have undergone a hyperopic ablation. Other than these patients, I have gone 100 percent aspheric," Dr. Nichamin says.
Dr. Kershner agrees. "Anyone who has had his or her cornea modified from the average standard corneal spherical aberration will not derive benefit from these lenses. Spherical IOLs should also be used in patients who do not have corneas with positive spherical aberration," he says.
Dr. Kershner notes that these lenses require capsular bag fixation, so they should not be used in patients whose capsular bag is compromised. In these cases, the lens could decenter or tilt.
If there is a concern about lens decentration or tilt, surgeons may want to consider the SofPort lens, which is the least sensitive. Dr. Nichamin says that in theoretical bench testing, based upon the amount of its inherent spherical aberration, the Tecnis lens is the most sensitive to mild decentration and tilt. He notes that clinical studies must confirm these suppositions, and these studies are underway in multiple centers.
 |
Patients who have the most to gain from aspheric lenses are those who have undergone myopic refractive surgery, according to Asim Piracha, MD, who is in private practice at the John Kenyon Eye Center with offices in Jefferson, Ind., and Louisville, Ky. "The patients who would do the worst with these lenses are those who have very steep corneas, such as keratoconus patients, or those who have had previous hyperopic refractive surgery. These patients already have negative spherical aberration in their corneas, and an aspheric IOL would create excessive negative spherical aberrations in their visual system," he says.
Another consideration for surgeons is the increased cost of aspheric IOLs over spherical IOLs, and this may be one reason why some surgeons are reluctant to use them. "In some elderly cataract patients who do not have visually demanding lifestyles and concomitant ocular pathology, I don't use aspheric lenses as I am unsure that these patients will perceive any benefit," Dr. Piracha says.
According to Dr. Kershner, because Medicare reimbursement is the same, regardless of the cost of the lens, there is a significant financial motivation for surgeons to use the least expensive lens they can get. "Surgeons' first motivation is for their patients, but if they feel they can get the same vision with the least expensive lens or if they don't believe that the new technology is much of an advantage, they may choose a different lens. I use aspheric lenses, and I believe that the more happy patients I have, the more new patients I'll see, but to say that financial factors don't enter into the equation at all would be unfair," he says.
Drs. Packer and Kershner note that the Tecnis lens is currently being considered for "new technology" status that would allow surgeons to charge an additional $50 to Medicare.
1. Kershner RM. Retinal image contrast and functional visual performance with aspheric, silicone, and acrylic intraocular lenses: Prospective evaluation. J Cataract Refract Surg 2003;29:1684-1694.
2. Packer M. Improvements in functional vision with a modified prolate IOL compared to a standard spherical IOL. Presented at the ASCRS meeting, Washington, DC, April 15-20, 2005.
3. Grimson JM, Schallhorn SC, Kaupp SE. Contrast sensitivity: establishing normative data for use in screening prospective naval pilots. Aviat Space Environ Med 2002;73:28-35.
4. Beiko G. Personalized correction of spherical aberration in cataract surgery. Presented at the AAO Meeting, Chicago, October 15-18, 2005.



