Although there is a tendency to think of dry eye as more of a nuisance than a disease, this is clearly not the case. Dry eye is a cellular disease on the cornea and conjunctiva, and it can have a major impact on patients' quality of life and the optical quality of the eye. Recent studies have helped ophthalmologists gain an understanding of how dry eye develops and have examined some promising new treatment options.
Ocular Irritation, Irregular Surface
A study conducted at the Ocular Surface Center at Baylor College of Medicine in Houston found that patients with ocular irritation have an irregular corneal surface that may contribute to their irritation and visual symptoms.1
The study was conducted to determine the correlation between the regularity indices of the Tomey TMS-2N computerized videokeratoscopy (CVK) instrument (Tomey, Waltham, Mass.) with conventional measures of dry-eye symptoms and disease.
 |
| Total corneal fluorescein staining scores are among the key measures of dry eye. |
Researchers evaluated the corneal surface irregularity and potential visual acuity indices on the Tomey TMS-2N CVK instrument in all study participants.
The study found that dry-eye patients had greater mean symptom severity scores, lower Schirmer 1 test scores, greater biomicroscopic meibomian gland evaluation with a composite severity score, more rapid tear breakup time, and greater total corneal fluorescein staining scores. Additionally, dry-eye patients had significantly greater surface regularity index (SRI), surface asymmetry index (SAI), and irregular astigmatism index (IAI) scores than normal subjects.
• SRI scores were 0.46 ±0.36 for normal eyes compared with 1.09 ±0.76 for dry eyes.
• SAI scores were 0.30 ±0.15 for normal eyes compared with 0.90 ±1.09 for dry eyes.
• IAI scores were 0.42 ±0.28 for normal eyes and 0.56 ±0.24 for dry eyes.
• The potential visual acuity index predicted significantly lower visual acuities in the dry-eye patients (0.89 ±0.13) compared to normal patients (0.68 ±0.23).
The SRI, SAI and IAI scores were positively correlated with total and central corneal fluorescein staining scores. An SRI of 0.80 or more, an SAI of 0.50 or more, and an IAI of 0.50 or more had sensitivities in predicting total corneal fluorescein staining of 89 percent, 69 percent, and 82 percent, respectively.
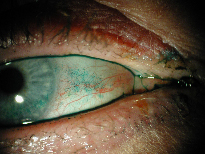 |
| Conjunctival lissamine green staining. A dry-eye-related irregular corneal surface may contribute to patients' irritation and visual symptoms. |
The study found that because of their high sensitivity and specificity, the regularity indices of the Tomey TMS-2N have the potential to be used as objective diagnostic indices for dry eye, as well as a means to evaluate the severity of this disease.
This study illustrates how dry eye causes degradation of the optical quality of the eye. Study participants with more dry spots on their eyes had more irregular corneal surfaces, demonstrating the importance of the tear film to visual function.
Hypersensitivity to Stress
Another study conducted at Baylor College of Medicine in Houston found that patients with dry eye were hypersensitive to an air jet stimulus.2
In this retrospective, clinic-based, case-control study, 20 normal subjects, 20 dry-eye patients, 20 post-LASIK patients without dry eye, and six post-LASIK patients with dry eye were evaluated. Corneal sensation was measured with the modified Belmonte gas esthesiometer that uses two different stimuli to assess mechanical and polymodal receptors on the corneal surface.
Mechanical receptors were assessed by two-second pulsed air jets of variable intensity, and polymodal receptors were measured by stimulating the cornea with two-second pulsed air jets of varying concentrations of CO2, a gas that is converted to carbonic acid when it comes in contact with the corneal surface.
According to the study results, the mean mechanical threshold was 61.50 ±20.07 ml/minute in the normal group, 34.60 ±21.09 ml/min in the dry-eye group, 99.50 ±47.40 ml/min in the post-LASIK group without dry eye, and 50.00 ±15.49 ml/min in the post-LASIK patients with dry eye. The percentage of CO2 that was needed to elicit discomfort was similar in all groups, and no gender-related differences were noted. A significant inverse correlation between the threshold of mechanical stimulation and the severity of corneal fluorescein staining was noted.
This hypersensitivity in patients with dry eye appears to be due to altered corneal epithelial barrier function. Profound hypoesthesia was observed after LASIK, and, similar to dry eye, post-LASIK patients with dry eye were sensitized. These findings provide new insight into dry-eye patients' hypersensitivity to environmental stresses, particularly air drafts.
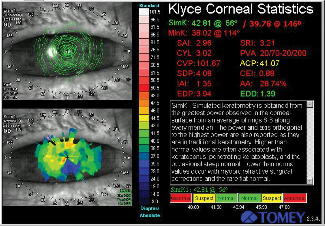 |
| Topograph of keratoconjunctivitis sicca. Apoptosis may play a role in the pathogenesis of KCS and may be a therapeutic target for the condition. |
Dry Eye Causes Apoptosis of Cells
Another study performed at the Ocular Surface Center at Baylor evaluated the effect of experimental dry eye on ocular surface apoptosis. We found that experimentally induced dry eye in mice causes apoptosis of cells in ocular surface tissues, including the central and peripheral corneal epithelium, bulbar and tarsal conjunctival epithelia, tarsal conjunctival stroma, and lid margin.3 Apoptosis may play a key role in the pathogenesis of keratoconjunctivitis sicca and may be a therapeutic target for this condition.
In this study, aqueous tear production and clearance were inhibited by systemic administration of scopolamine and exposure to an air draft for 12 days in four- to six-week-old 129SvEv/CD-1 mixed white mice. Eyes and ocular adnexa were excised, cryosectioned and evaluated for apoptosis by terminal deoxynucleotidyl transferase-mediated dUTP-digoxigenin nick end labeling (TUNEL) assay, immunohistochemical assay for caspase-3 and poly(ADP-ribose) phosphate (PARP), and examination of nuclear morphologic changes by Hoechst DNA nuclear staining and transmission electron microscopy.
We found that the number of TUNEL-positive cells in the mice with induced dry eye was significantly higher than the control mice in the following ocular regions: central corneal epithelium, peripheral corneal epithelium, bulbar conjunctival epithelium and tarsal conjunctival epithelium, tarsal conjunctival stroma, and lid margin. No significant differences were observed between mice with dry eye and controls in the central corneal stroma, peripheral corneal stroma, or bulbar conjunctival stroma; meibomian glands; skin; retina-choroid; or episcleral regions. Immunohistochemistry for caspase-3 and poly(ADP-ribose) polymerase p85 fragments revealed increased immunoreactivity in regions of increased TUNEL positivity, particularly in the corneal and conjunctival epithelial cells. Ultrastructural morphologic changes consistent with apoptosis were observed in the conjunctival epithelial cells.
As the eye becomes dry, there is rapid cell death of the superficial epithelial cells on the eye. This is probably due to inflammation or activation of this cell death pathway. Normally, there is a very slow turnover of epithelial cells on the cornea. So that the layer of epithelial cells doesn't get too thick, there is a gradual loss of dead cells from the surface, which are replaced with new cells from the bottom layer. When cells get to the top layer, some will die in a process called apoptosis, or programmed cell death.
In patients with dry eye, the cells die much more rapidly, which increases epithelial cell turnover. In an attempt to keep up with the accelerated loss of the superficial epithelial cells, many immature cells without a mucous coating are found on the surface of the eye.
The Role of T-Cell Activation
A study conducted by Allergan and the National Eye Institute has found that clinical symptoms of KCS may be more dependent on T-cell activation and resulting inflammation than previously believed.4
The study was conducted to examine the conjunctiva of patients with Sjögren's syndrome keratoconjunctivitis sicca (SS-KCS) and non-Sjögren's keratoconjunctivitis sicca (NS-KCS) for evidence of immune-based inflammation.
Researchers obtained conjunctival biopsy specimens from 15 patients with SS-KCS and 15 patients with NS-KCS. Immunohistochemistry was performed on frozen sections to characterize and quantify T-cell subtypes (CD3, CD4, and CD8) and markers of immune activation (major histocompatibility complex [MHC] class II: HLA-DR, HLA-DQ) and inflammation (intercellular adhesion molecule [ICAM]-1). Two masked investigators counted and averaged the numbers of cells positive for each marker.
In both types of dry eye, conjunctival biopsy specimens revealed that there was a significant increase in T lymphocytes in the conjunctiva, both in the epithelium and the stroma. The extent of cellular immunoreactivity did not differ significantly between SS-KCS and NS-KCS tissue samples.
This study concludes that patients with SS-KCS and NS-KCS have conjunctival inflammation manifested by inflammatory cell infiltrates and increased expression of immune activation markers. The investigators recommend that, in addition to tear substitutes, anti-inflammatory therapeutics should be investigated for the treatment of KCS.
Autologous Serum Drops for Dry Eye
A study conducted in the United Kingdom found that autologous serum has beneficial effects in treating severe ocular surface disorders.5
In this prospective, randomized, crossover trial, 31 eyes in 16 patients were randomized to either 3 months of 50 percent autologous serum drops followed by three months of conventional treatment, or three months of conventional treatment followed by three months of 50 percent autologous serum drops. Six patients had Sjögren's syndrome, and five patients had keratoconjunctivitis sicca.
Patients underwent the following clinical assessments at study entry and then on a monthly basis: Schirmer's test and rose bengal and fluorescein staining. Additionally, impression cytology was performed at entry and at three and six months. Grading was carried out on degrees of squamous metaplasia and goblet cell density, and subjective comfort was recorded daily using the "faces" scale.
Impression cytology was available in 25 of 31 eyes and showed significant improvement on serum treatment. Additionally, Rasch weighted faces scores were statistically significantly better with serum than with conventional treatment.
Unlike artificial tears, serum contains proteins and growth factors that make it ideal for treating dry eye. As the eye becomes dry, especially if the patient has an aqueous tear deficiency as is seen in Sjögren's syndrome, many of the important growth factors that come from the lacrimal gland are low in concentration or are absent. These can be replaced by using serum.
Corticosteroids for Dry Eye
A study conducted at Louisiana State University has found that topical corticosteroids have a beneficial effect on both the subjective and objective clinical parameters of moderate to severe dry eye.6 These effects were associated with the reduction of inflammation markers of conjunctival epithelial cells.
This single-masked, randomized, prospective clinical trial included 32 keratoconjunctivitis patients with or without Sjögren's syndrome. Patients were randomized to one of three groups: group 1 patients received a topical artificial tear substitute (ATS); group 2 received ATS plus a nonsteroidal anti-inflammatory drug (NSAID); and group 3 received ATS plus topical corticosteroid drops. At baseline and at 15 and 30 days after the start of treatment, eye symptom severity scores, Schirmer's test values, and rose bengal and fluorescein staining scores were evaluated. Impression cytology specimens were stained using immunohistochemical methods to detect the percentages of human leukocyte antigen II (HLA-DR) positive, Apo 2.7 positive, and periodic acid-Schiff positive cells.
The researchers found that patients in group 3 (those who received ATS plus topical corticosteroid drops) had significantly lower symptom severity scores, fluorescein and rose bengal staining, and HLA-DR positive cells on days 15 and 30 compared with patients in other groups. They also had a significantly higher number of periodic acid-Schiff positive (goblet) cells in their impression cytology specimens on days 15 and 30 compared with the other patients. On day 30, patients in this group had significant differences compared with their baseline measurements. The investigators did not, however, detect a significant effect of any treatment schedule on the Schirmer's test value and the numbers of Apo 2.7 cells in impression cytology specimens.
This study highlights the importance of inflammation in dry eye. Inflammation is the main reason that epithelial cells start sloughing off. As the eye becomes dry, the cells produce inflammatory mediators. This can happen in several ways.
First, the eye can become dry because the patient doesn't blink and air dries out the eye. Second, changes in the composition of the tear film can cause pathologic changes in the surface epithelium. If the salt concentration in the tears goes up, it stimulates the cells on the surface of the eye to produce inflammatory mediators. Third, when the lacrimal gland doesn't function well, as in patients with Sjögren's syndrome, it can secrete inflammatory mediators into the tears. Regardless of the cause, treating dry eye with an anti-inflammatory agent will improve the condition.
Future Research
Although recent studies have revealed some of the mechanisms of dry eye and have evaluated new treatment modalities, there is still much to be learned.
We believe that hormones play a role in dry eye, but we have not yet determined their exact function and balance. Dry eye is well known to increase with age, especially in women after menopause. Normally, hormones suppress inflammation and proteolytic enzymes. Hormone imbalances can cause these proteases to be more active, which promotes dry-eye disease.
Paradoxically, hormone replacement therapy can worsen dry-eye symptoms in some cases, and estrogen-only hormone replacement therapy seems to be worse than estrogen and progesterone combined therapy. There have been few recent studies examining the effect of hormone replacement therapy on dry eye because of the bad publicity surrounding hormone replacement therapy in the past couple of years.
We do know that many different hormones come into play, however. For example, David Sullivan, PhD, has found that androgen hormones seem to be protective for dry eye.7 Once the exact role of hormones is determined, we may be able to use them to treat dry eye.
Another future direction of treatment is to use more targeted therapy to inhibit specific mediators in dry eye. For example, if we knew that a certain factor was causative, we could give an inhibitor of that factor. We know that inflammation is important, but we don't know the relative importance of each of the mediators. Once we know that, it will be easy to devise therapies to inhibit the specific mediator.
Dr. Pflugfelder is a professor of ophthalmology at Baylor College of Medicine. Contact him at (713) 798-4732 or stevenp@bcm.tmc.edu.
1. de Paiva CS, Lindsey JL, Pflugfelder SC. Assessing the severity of keratitis sicca with videokeratoscopic indices. Ophthalmology 2003;110:1102-1109.
2. de Paiva CS, Pflugfelder SC. Corneal epitheliopathy of dry eye induces hyperesthesia to mechanical air jet stimulation. Am J Ophthalmol 2004;137:109-115.
3. Yeh S, Song XJ, Farley W, Li D, Stern ME, Pflugfelder SC. Apoptosis of ocular surface cells in experimentally induced dry eye. Invest Ophthalmol and Vis Sci 2003;44:124-129.
4. Stern ME, Gao J, Schwalb TA, et al. Conjunctival T-cell subpopulations in Sjogren's and non-Sjögren's patients with dry eye. Invest Ophthalmol and Vis Sci 2002;43:2609-2614.
5. Noble BA, Loh RSK, MacLennan S, et al. Comparison of autologous serum eye drops with conventional therapy in a randomized controlled crossover trial for ocular surface disease. Brit J Ophthalmol 2004;88:647-652.
6. Avunduk AM, Avunduk MC, Varnell ED, Kaufman HE. The comparison of efficacies of topical corticosteroids and nonsteroidal anti-inflammatory drops on dry-eye patients: a clinical and immunocytochemical study. Am J Ophthalmol 2003;136:593-602.
7. Sullivan DA, Sullivan BD, Evans JE, et al. Androgen deficiency, Meibomian gland dysfunction, and evaporative dry eye. Ann N Y Acad Sci 2002;966:211-222.



