When patients present with ocular conditions that have no apparent cause, it is important to consider whether the condition could be caused by a systemic medication they are taking. Patients will often neglect to mention the maintenance drugs that they take every day, over-the-counter medications and herbal supplements, so ophthalmologists may need to ask specifically about these types of medications.
“Ophthalmologists may not ask about these very commonly used drugs, and a lot of patients will just assume that they aren’t real medicines because they are kind of maintenance medicines. They think it’s like taking a vitamin,” according to Jonathan D. Trobe, MD, a professor in the Departments of Ophthalmology and Visual Sciences, and Neurology, at the University of Michigan’s Kellogg Eye Center.
While this article does not include an exhaustive list, common systemic medications that cause ocular side effects include: bisphosphonates; cyclosporine and tacrolimus; minocycline; hydroxychloroquine; ethambutol; topiramate; tamsulosin; amiodarone; anticholinergics; erectile dysfunction drugs; blood pressure medications; and some herbal medications.1
Bisphosphonates
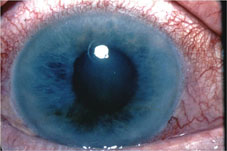
 |
| Episcleritis caused by osteoporosis medications. |
Cyclosporine and Tacrolimus
These drugs are commonly used in patients who have undergone organ or bone marrow transplants, and they can cause posterior reversible encephalopathy syndrome. These patients will present with bilateral vision loss. “Some of these patients will also have seizures and mental status alterations, so that they become a little confused,” Dr. Trobe says. “Others may just come in with vision loss, which is not from the eyes. It is from the back of the brain, so an MRI scan is required to make this diagnosis, and it’s pretty definitive.”
The condition will almost always resolve once the patient discontinues the medication. However, the sooner the condition is caught, the better. “These drugs interfere with circulation to the back of the brain, and patients can sometimes go on to develop stroke, which is irreversible,” he explains.
A recent case study described a patient who was prescribed tacrolimus after a cadaveric kidney transplant and experienced blurry vision that was a result of aqueous tear deficiency as a dose-dependent adverse effect of oral tacrolimus.2
Minocycline
Minocycline is a tetracycline derivative and is commonly used to treat acne. It is prescribed for many teenagers because of its effectiveness. However, it can cause increased intracranial pressure and papilledema, which can cause permanent vision loss if it’s not reversed. Patients may get a headache from the high pressure, but some do not. “They will eventually develop blurred vision from this. When they go to an eye doctor, the eye doctor will see the papilledema,” Dr. Trobe notes.
Hydroxychloroquine
Hydroxychloroquine (Plaquenil) is used to treat malaria, lupus and rheumatoid arthritis. It is a known retinal toxin, and the effects are irreversible. Fortunately, most patients taking this drug do not experience side effects at the dosages usually prescribed. “Most rheumatologists know about this complication, and patients are usually screened for it,” Dr. Trobe says. “The confusing and controversial question is, what should the screening be? In other words, how often should we screen, what should we do, and what’s the easiest way of recognizing the earliest form of retinal toxicity? Because it’s irreversible, you want to be able to see it very early on. There have been some new guidelines suggested, and, at the moment, things are in flux. [Optical coherence tomography] looks like a good way to screen for patients with this, but OCT is expensive, and it may be too expensive considering the low likelihood of having toxicity.”
According to a recent study, there is currently no gold standard for identifying ocular toxicity prior to its development, which has led to controversy regarding recommendations for screening patients taking hydroxychloroquine.3
Dr. Trobe notes that patients with normal kidney function who are taking 6.5 mg/kg/day or less have an extremely low chance of developing retinal toxicity, especially if they have not taken the drug for more than five years.
Ethambutol
This drug is widely used to treat mycobacterial disease, including tuberculosis. If it is not taken at safe doses, it is an optic nerve toxin.4 The damage typically occurs slowly and progressively in both eyes, and it is usually irreversible.
Patients are typically treated with doses up to 25 mg/kg/day, especially shortly after diagnosis. Safe doses are 15 mg/kg/day or less. “Very few people at that dose have ever gotten into trouble,” Dr. Trobe says. “The few who do usually have kidney disease, which causes the drug to not be properly eliminated. If you’re at the safe dose, it is possible that screening is not necessary.”
Topiramate
Topiramate (Topamax) is used to treat epilepsy and migraine headaches, and it is used off-label for weight loss, according to Rick W. Fraunfelder, MD, who is in practice at the Casey Eye Institute in Portland, Oregon. It can cause angle-closure glaucoma soon after starting treatment. “In these patients, the drug should be stopped, or patients can lose their vision,” he says.
A recent study conducted in Turkey found that topiramate induced changes in the eye.5 The study included 76 eyes of 38 patients who were taking topiramate for the treatment of migraine. Patients were examined at baseline and after 15, 30 and 90 days of topiramate treatment. After 90 days of treatment, the median refractive error value significantly increased from -0.25 D to -0.62 D. Mean central corneal thickness was 570.56 µm before treatment and increased to 573.69 µm at the 15-day follow-up, 575.31 µm at the 30-day follow-up, and 574.56 µm at the 90-day follow-up. These changes were not statistically significant.
Additionally, mean retinal thickness increased from 263.46 µm to 271.60 µm, which was not statistically significant. The mean retinal nerve fiber layer thickness was 100.56 ±15.36 µm before treatment and significantly increased to 110.2 ±8.41 µm at the 30-day follow-up and 111.03 ±14.59 µm at the 90-day follow-up.
Tamsulosin
Ophthalmologists need to ask about patients’ use of tamsulosin (Flomax), which is used to treat prostate enlargement and improve urinary flow in men. “Everyone seems to be on a drug to control their urine,” says Cindy M.L. Hutnik, MD, PhD, a professor at the Ivey Eye Institute in London, Ontario. “Men can’t pee, and ladies pee when they don’t want to. Almost every patient of a certain age seems to be on this drug, which can have definite effects in the eye. The well-known syndrome, intraoperative floppy iris syndrome, used to occur only in men who were on medicine to relax their prostate. Now, urologists are treating women with these drugs, and that can, at the time of cataract surgery, make surgical risk much higher.”
She notes that even if the drug is discontinued, the patient is at a lifetime risk of more complicated cataract surgery. So, ophthalmologists need to ask whether the patient is currently taking tamsulosin and whether he or she has ever taken it.
Amiodarone
Amiodarone (Cordarone) effectively treats cardiac arrhythmias. It causes the appearance of a whorl in the cornea, which does not usually cause symptoms, although some people can have a little bit of blurred vision, according to Dr. Trobe. “It is also said to cause ischemic optic neuropathy,” he adds. “In my opinion, the evidence is not robust, but it is out there and doctors are very much conscious of it. They are afraid to use it in patients who have developed ischemic optic neuropathy in one eye while taking amiodarone because of the threat of malpractice litigation should the patient develop ischemic optic neuropathy in the second eye.”
Anticholinergics
Dicyclomine (Bentyl), and other drugs with anticholinergic effects, are administered to patients who have stomach conditions that require stomach relaxers and to patients with Parkinson’s disease. Young patients taking these drugs will develop difficulty with accommodation.
Erectile Dysfunction Drugs
| "Patients who take [erectile dysfunction drugs] also have other reasons to get ischemic optic neuropathy. But patients who use these drugs—especially those who have vision in only one eye—are entitled to know that they may be at risk for this condition."
— Jonathan D. Trobe, MD |
According to Dr. Fraunfelder, in addition to vision having a blue hue, patients can also see shimmering around objects. “These drugs can also cause central serous retinopathy, which is a collection of fluid in the macula in the back of the eye, and they can cause subconjunctival hemorrhages,” he says. “Many doctors think erectile dysfunction drugs cause optic neuropathy, but we haven’t seen any proof of that in our literature reviews. It’s unlikely but possible. We just don’t know enough about it yet.”
In fact, a recent study found that there is “lack of conclusive evidence to indicate a direct cause-effect relationship between PDE5 inhibitor use and vision-threatening ocular events. Men who use PDE5 inhibitors appear to suffer vision-threatening complications at the same frequency as the general population.”6 The study found that minor visual adverse effects occur in 3 percent to 11 percent of users and that they are reversible.
Blood Pressure Medications
 |
| Aggressive management of blood pressure, especially with diuretics or calcium channel blockers, may contribute to open-angle glaucoma. |
Herbal Medications
Herbal medications are reportedly a $60 billion industry worldwide and a $20 billion industry in the United States. “Basically half of the population takes some sort of nutritional supplement or herbal medicine, and half of those people don’t tell their doctors about it because they don’t think it’s pertinent,” says Dr. Fraunfelder. “However, it can be pertinent, because sometimes herbal medications can interact with prescription medicines the patient is already taking. For instance, gingko biloba causes patients to have a longer bleeding time, so it can make people who take blood thinners more prone to bleeding.”
Dr. Fraunfelder adds that black bitter licorice has ocular side effects, causing migraine headaches with visual side effects, such as scintillating scotomas in patients’ vision. Additionally, canthaxanthin, which can be taken orally as a tanning agent and is used in some foods as a coloring, can deposit in the retina in little crystals that can change some electroretinogram readings.
1. Santaella RM, Fraunfelder FW. Ocular adverse effects associated with systemic medications: recognition and management. Drugs 2007;67(1):75-93.
2. Kapoor KG, Mirza SN, Gonzales JA, Gibran SK. Visual loss associated with tacrolimus: Case report and review of the literature. Cutan Ocul Toxicol 2010;29(2):137-139.
3. Tehrani R, Ostrowski RA, Hariman R, Jay WM. Ocular toxicity of hydroxychloroquine. Semin Ophthalmol 2008;23(3):201-209.
4. Talbert Estin KA, Sadun AA. Risk factors for ethambutol optic toxicity. Int Ophthalmol 2010;30:63-72.
5. Ozturk BT, Genc E, Tokgoz M, Kerimoglu H, Genc BO. Ocular changes associated with topiramate. Curr Eye Res 2011;36(1):47-52.
6. Azzouni F, Abu Samra K. Are phosphodiesterase type 5 inhibitors associated with vision-threatening adverse events? A critical analysis and review of the literature. J Sex Med 2011 Jul 19. [Epub ahead of print].



