Although trabeculectomy is still the gold standard for glaucoma surgical treatment, it's far from perfect. Despite our best surgical efforts, we sometimes see bleb leaks or blebitis, especially when Mitomycin-C is used. Problems that arise in the late postop period can be especially vexing, possibly even leading to vision loss.
Recently, Peter J. Maris Jr., MD, Kyoko Ishida, MD, and I completed a clinical study aimed at shedding light on a new surgical technique: We compared the effectiveness and complications of trabeculectomy to those associated with implanting Optonol's Ex-PRESS miniature glaucoma device under a scleral flap. (The study report was published last month in the January issue of Journal of Glaucoma.1) None of the study authors—including myself—have any proprietary interest in Optonol or the Ex-PRESS implant.
The Ex-PRESS device is a stainless steel shunt that, to date, has shown excellent biocompatibility with human tissue. (It's also safe for magnetic resonance imaging scanning.) Originally, the device was simply placed underneath the conjunctiva rather than a scleral flap, but this produced some variability in outcomes, and occasionally the device would erode through the conjunctiva. Today, most surgeons using the Ex-PRESS shunt place it under a scleral flap instead.
For our study, we compared 50 eyes in 49 patients implanted with the Ex-PRESS miniature glaucoma shunt (under a scleral flap) with 50 matched control eyes in 47 patients who received a trabeculectomy. Our technique was similar to trabeculectomy; we made a conjunctival flap, either fornix or limbus-based, followed by a triangular, partial-thickness scleral flap. We inserted the device under the scleral flap into the anterior chamber through a 27-ga. needle track for the R-50 shunt (or a 25-ga. needle track for the X-50 or T-50). We then closed the flap with interrupted nylon sutures, allowing us to perform laser suture lysis postoperatively, if necessary. Finally, we closed the conjunctival incision in the standard manner. (Note that there was no need to perform a sclerostomy or iridectomy.) Mitomycin-C was used in all surgeries in the study.
We compared intraocular pressure and complications over a period of 15 months, defining success as an IOP of ≥5 mmHg and ≤21 mmHg, with or without glaucoma medications, but with no further surgery. We defined early postoperative hypotony as an IOP less than 5 mmHg during the first postoperative week.
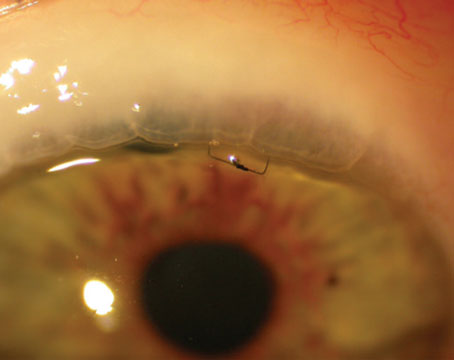
The Ex-PRESS shunt under a scleral flap, postop day one. The bleb is elevated but fairly diffuse, the chamber is deep, and there is little inflammation.
Results
Our data suggest that the Ex-PRESS shunt, used in this way, may provide long-term results equal to those produced by trabeculectomy, while reducing some of the short-term risks associated with trabeculectomy. Specifically, we found:
• Less risk of hypotony. The data showed a significantly higher mean IOP during the early postoperative period with the implant than in the eyes treated with trabeculectomy. In fact, we found a statistically significant difference in the rate of postop hypotony—the primary cause of complications in the early postop period—favoring the Ex-PRESS shunt.
• Fewer complications. We found a reduced overall rate of complications compared with trabeculectomy as well, including fewer choroidal effusions after the implant.
• Less inflammation. Postop inflammation was difficult to quantify, but subjectively, patients experienced minimal inflammation. We observed this difference as well. The fact that implanting the Ex-PRESS shunt does not involve performing a sclerostomy or an iridectomy may account for this. Typically, eyes looked very quiet during the early postop period.
• Same benefits over the long term. At the end of 15 months we found no significant difference between the Ex-PRESS implant and trabeculectomy in terms of mean IOP [see chart, below], number of medications used or survival curves. Both options performed well. (It's worth noting that a similar prospective, randomized study by De Jong and coworkers, reported at ARVO this year but not yet published, found that the Ex-PRESS device implanted under a scleral flap was more effective than trabeculectomy in terms of IOP reduction and medication reduction.)
In a comparison of mean IOP following implantation of the Ex-PRESS shunt under a scleral flap and trabeculectomy, the two groups were statistically significantly different at multiple time points during the early postoperative period. (Data from: Maris PJG Jr, Ishida K, Netland PA.)
In addition to these statistical results, we observed that the Ex-PRESS procedure requires less time to perform, because there's no need for sclerostomy and iridectomy. We also felt that it reduced our postop time because we were managing fewer complications. In terms of ease for the surgeon, a number of ophthalmologists working with trainees have noted that beginners pick up the technique very quickly, and the anterior chamber usually remains well-formed throughout the procedure.
In terms of downsides, the Ex-PRESS shunt is a more costly treatment. However, the device and the procedure are covered by insurance, and it hasn't been a burden for our patients. Also, biocompatibility problems could crop up at some point in the future, although we're not aware of any at this time. And we can't assume that our results will apply to other devices being developed; glaucoma drainage implants such as the Baerveldt or Ahmed valves are generally used for different indications.
A Good Beginning
Overall, our clinical impressions are that this procedure is a useful alternative to trabeculectomy; it does seem to reduce tissue trauma and inflammation; it provides more predictable results; and it appears to cause fewer complications. We also found this to be true in cases of combined cataract and glaucoma surgery. We are currently assembling data on a non-comparative series of 300 eyes which we hope will shed more light on how the Ex-PRESS device performs clinically under a scleral flap.
Given this data, should surgeons consider switching from trabeculectomy to implanting the Ex-PRESS shunt under a scleral flap? As with all surgical alternatives, it's an individual choice. I think some surgeons will find this approach to be advantageous, but it's still early to make general recommendations. However, we hope that this data, along with other data now being gathered, will help to make such decisions easier.
Dr. Netland is the Siegal Professor, director of glaucoma and vice chair for academic affairs in the Department of Ophthalmology at the Hamilton Eye Institute, University of Tennessee Health Science Center, Memphis, Tenn.
1. Maris JG Jr, Ishida K, Netland PA. Comparison of Trabeculectomy With Ex-PRESS Miniature Glaucoma Device Implanted Under Scleral Flap. J Glaucoma, Jan. 2006.