This year saw the approval and introduction of the two new members of the fluoroquinolone family, a fourth generation of antibacterial agents: Vigamox (moxifloxacin HCl 0.5%, Alcon) and Zymar (gatifloxacin 0.3%, Allergan).
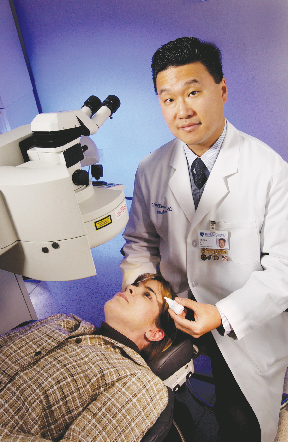
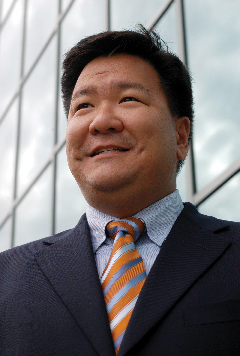
As with any new product, physicians are still evaluating the new drugs to determine their clinical preferences. We asked two leading ophthalmic clinician-researchers to assess the new drugs and the studies used to gain their regulatory approval, and which factors deserve special emphasis when considering the fourth-generation drugs. Terry Kim, MD, of Duke University, and Ralph Chu, MD, medical director of Chu Vision Institute and a surgeon practicing in Minnesota, joined with moderator, Francis Mah, MD, himself a researcher, clinician and educator at the University of Pittsburgh, to hash out the issues.
 |
| Francis Mah, MD |
Dr. Mah: Has either of you witnessed any clinical differences between Zymar and Vigamox, in terms of healing in your own patients?
Dr. Kim: At Duke we've been evaluating both Zymar and Vigamox for prophylaxis in cataract and refractive surgery, as well as for the treatment of corneal ulcers. I have not noticed any clinical differences in either setting, and I've been trying to pay more attention to this. For instance, after LASIK, checking the epithelial edge along the flap the next day, and after cataract surgery, inspecting the wounds carefully to see if re-epithelialization is occurring at a normal rate. I haven't done any controlled or prospective studies, but I have to say I've not had any adverse outcomes or delayed healing with either antibiotic.
Dr. Chu: Our experience is predominantly with Zymar and we have not seen any toxicity in our patients. However, I am aware of a study performed by Dr. Majid Moshirfar at the University of Utah comparing epithelial healing rates in humans undergoing penetrating keratoplasty. He found slower epithelialization, more red eyes, and more significant SPK in eyes treated with Vigamox.
 |
| Terry Kim, MD |
Dr. Kim: I've heard that story too, Ralph. We do a large number of corneal grafts here, and I've had an opportunity to use both antibiotics. Healing is something we're obviously very cognizant about after penetrating keratoplasty. Again, we haven't done any formal study, but I have not noticed delayed epithelial healing with one versus the other in this setting.
Dr. Chu: Dr. Moshirfar's hypothesis was that healing should be better and that there should be less toxicity with Vigamox since there is no BAK in the formulation. In this prospective, randomized, non-pharmaceutical company sponsored study, he found the opposite and to me that is compelling.
Dr. Kim: Over the past year, ophthalmologists have been bombarded with data regarding all of the issues of the fluoroquinolones: potency, spectrum of activity, penetration and toxicity. And there have been in vitro, ex vivo, and in vivo studies. I think it's important that we look at certain factors regarding these studies to try to come up with as fair an answer as possible. For example, we should look to make sure commercial preparations of medications are used. Obviously, look at study design. Are animal models appropriate? Are there sufficient "n's" to draw statistical significance; at least enough to prove the data? And I think all ophthalmologists would like to see human data. Obviously many of these studies cannot be easily done in humans, but we'd like to draw as much clinical relevance as possible.
Dr. Mah: Ralph, what do you think about the non-human studies? If they're well-done, show significance, use commercial product and the model looks good; what's the significance of this type of information?
Dr. Chu: I think that well-controlled human studies using commercially available preparations for the comparison probably provide the most clinically useful data. However, since it is not feasible in most cases to use humans to gather much of the data we need, I think there is a role for in vivo and in vitro studies. Using the right model to detect differences is essential. For example, Dr. [Stephen] Pflugfelder performed an epithelial toxicity comparison of Zymar vs. Vigamox in a dry-eye mouse model and found more disruption of tight junctions and loss of the epithelial barrier function in the Vigamox treated group. If a different non-stressed in vivo model were used, you may not have seen the difference. That does not mean there aren't differences, you just need the right model to look for them. As long as both drugs are treated equally during testing, then I think significant value can be gathered from the in vivo animal models.
Dr. Kim: It's interesting because if you say "stress," one question may be: Is the stress itself causing some abnormalities in wound healing? It's difficult for a lot of ophthalmologists to extract what is the direct cause and effect relationship there. Is it the antibiotic? Is it the stress? Is it a combination of these? All of us know as corneal specialists that it's not always one single variable there.
 |
| Y. Ralph Chu, MD |
Dr. Chu: As long as both drugs or groups in a study are subjected to the same conditions equally, stressed or non-stressed, then the questions you raise become irrelevant. This is the danger of comparing data across different study models. It causes confusion. Another point for the clinician to keep in mind is the number of studies reaching the same conclusion. When the in vivo data and the human data correlate in multiple studies comparing the drugs under equal conditions in each study that is powerful.
Dr. Kim: However, I believe ophthalmologists really want to know the validity and clinical relevance of these studies and how these studies will affect their patients in clinical practice, regardless of the number of studies performed. The issue of penetration, for example, is not something we can assess clinically. We can't see a patient and determine the concentration of an antibiotic in the cornea, aqueous humor, and vitreous. So we have studies, some with animal data (Robertson et al, ARVO 2004) and some with human data (Katz et al, ARVO 2004), that have helped prove the superior penetration of Vigamox. Older studies on topical ofloxacin penetration (Donnenfeld et al, Arch Ophthalmol 1997) helped acknowledge the importance of adequate antibiotic penetration in target tissues to protect against infection. On the other hand, I can, to some extent, make an assessment of positive vs. negative toxicity clinically. I can stain the ocular surface with fluorescein and see if the epithelium is experiencing delayed healing, in whatever wound or incision you're talking about. Precipitation is another good example. Because ophthalmologists were able to witness this phenomenon clinically with some of the older fluoroquinolones, they paid a lot more attention to it. But over the past year, in using both fourth-generation fluoroquinolones, I simply have not observed any toxicity or adverse effects in wound healing with cataract, corneal and refractive surgery.
Dr. Mah: What do you think about the clinical experience Terry is talking about, Ralph?
Dr. Chu: I think paying attention to the toxicity studies is important. Not every ophthalmologist is going to see precipitates in every patient on Ciloxan. Fluorescein staining and slit lamp evaluation can only detect gross wound healing abnormalities. Almost when it is too late. Avoiding toxicity through what we learn from animal studies is key. I am hearing anecdotal reports from around the country concerning toxicity, especially concerning epithelial closure rates.
Dr. Kim: I definitely agree with that, too. All of us know the importance of evaluating an in vitro study. In the beginning, that's all we have to go on in terms of predicting the clinical performance of an antibiotic.
Dr. Mah: What kinds of reports of toxicity are you hearing anecdotally?
Dr. Chu: I am hearing about delayed epithelialization after PRK and LASEK. There are also two prospective randomized human studies concerning epithelial toxicity, one by Dr. Eric Donnenfeld's group in Long Island evaluating post- PRK wound healing and the other by Dr. Moshirfar in Utah evaluating post-PK wound healing.
Dr. Kim: But you're also hearing about animal and human studies that are refuting this. For example, Dr. Richard Yee will also present a study at AAO that failed to show a difference between Vigamox and Zymar in epithelial healing rates following PRK in human patients. These findings seem to be more in line with my clinical experience with these products.
Dr. Mah: What types of studies need to be done to convince doubting clincians about issues of re-epithelialization regarding these antibiotics? Do other studies need to be done to convince people or to really show the differences or are the available studies enough?
Dr. Chu: I think the most powerful studies are the human, prospective randomized comparative studies. The first of these are coming to publication and I hope to see more.
Dr. Mah: Dr. Dan Durrie had an abstract [ASCRS 2004] on human contralateral LASIK cases; one eye Zymar, one eye Vigamox, same patient. There was no difference in any parameter that he studied. Does that add to the proof or mix things up?
Dr. Chu: I don't think that in a routine LASIK patient that I would expect much difference in toxicity, especially at the one-week time point when the patients were first evaluated. Unless the epithelium is damaged and has to recover from an injury as in PRK, LASEK, or post-PK, we may not see a difference. Other studies are now showing this.
Dr. Kim: I actually think a straightforward study without external stresses may be a better way to see if the antibiotic itself is actually contributing negatively to wound healing. Dr. Durrie's randomized, prospective, double-masked study was straightforward and clearly showed no difference in wound healing, pupil size, redness, etc. on LASIK patients using Vigamox or Zymar. To further counter the claims of potential fluoroquinolone toxicity, Mitch Friedlander did an independent, contralateral study (ARVO 2004) where normal volunteers were randomized to Vigamox in one eye and Zymar in the other eye. They also failed to show a difference between the two fluoroquinolones when measuring conjunctival injection, pupil size and corneal sensation. And this is a type of study any ophthalmologist can perform informally in the office to assess firsthand if any adverse effects are noted. We tried this at Duke and couldn't find a difference as well.
Dr. Mah: What is the impact of the toxicity studies right now? Have they raised some eyebrows?
Dr. Kim: I think they have sparked some speculation, but they have also been refuted by studies with contradictory findings, and, most importantly, by ophthalmologists' own experiences with these agents. The toxicity studies are out there, and people may be looking at them, but I don't think it's caused any major change in clinical practice. I myself have not heard any anecdotal accounts of delayed healing with Vigamox, and I've tried to look at why this would occur. With Vigamox's physiologic pH of 6.8 and its BAK-free formulation, we simply shouldn't see discomfort, toxicity or any adverse effect on wound healing. So further prospective, randomized, double-blinded studies in humans should elucidate whether or not this is really being seen on the clinical level.
Dr. Mah: What about you, Ralph? Do you think these studies have become an issue for clinicians?
Dr. Chu: I definitely think the toxicity studies have caused clinicians to think twice about which fluoroquinolones to choose for their patients. We are learning to think about another aspect of these antibiotics: wound healing. We are used to thinking about penetration, MICs, etc., but now we have to choose an antibiotic with favorable pharmacokinetics that causes the least amount of toxicity to the cornea. What these studies are teaching is that BAK is not the only source of toxicity in an ophthalmic formulation, and even a BAK-free solution can have significant toxicity.
Dr. Mah: Ralph's done a study showing excellent penetration with Zymar. Terry, what's the significance of penetration of antibiotics, especially these fluoroquinolones, therapeutically and for prophylaxis?
Dr. Kim: Penetration is key and is a crucial complement to potency when evaluating an antibiotic's clinical efficacy. The minimum inhibitory concentration of an antibiotic is meaningless if the antibiotic cannot reach the target tissue in sufficient concentrations. So factors like molecular structure, pH, and concentration are very clinically relevant since they largely affect the penetration of an antibiotic. That's why Vigamox's unique biphasic molecular structure, physiologic pH, and higher concentration contribute to its superior penetration. A number of head-to-head comparative human studies by Drs. Solomon and Donnenfeld (ARVO 2004) and McCulley (ASCRS 2004) have consistently shown that Vigamox penetrates into the aqueous humor better than Zymar. Although studies such as yours and Dr. Price's (ARVO 2004) did show good aqueous humor penetration in humans with Zymar, a key factor was that dosing of Zymar had to be increased to levels not routinely used perioperatively (i.e., more than q.i.d.) in order to achieve these concentrations. This makes sense when you consider that fluoroquinolones are concentration-dependent killers. The more frequent the dosing, the more antibiotic you're going to get inside the target tissue, and the higher the therapeutic index (peak concentration or Cmax/MIC90 ratio) With the concerns of increased endophthalmitis rates following clear corneal cataract surgery and the heightened awareness of LASIK-associated infections, I think every ophthalmologist is going to want an antibiotic with superior penetration and potency, since this will translate into better clinical performance. These criteria will apply for the therapeutic as well as the prophylactic use of these antibiotics.
Dr. Mah: Some say it doesn't matter how much antibiotic penetrates, as long as you get a therapeutic level into your tissue, the cornea or the anterior chamber.
Dr. Kim: That's why I mentioned the therapeutic index. The therapeutic index of an antibiotic (Cmax/MIC90 ratio) is becoming increasingly important, since this index takes into account an antibiotic's penetration or peak concentration in the target tissue relative to its MIC90. That's the reason why you hear the experts say that a Cmax/MIC90 ratio of 10:1 is predictive of a clinical cure for fluoroquinolone antibiotics. We should try to achieve tissue concentrations that are at least 10X above the MIC90 in order to kill the organism. So a higher concentration of an antibiotic will increase the chance of a clinical cure. And that therapeutic level is going to be dependent on dosing, as we discussed. So why not use an antibiotic like Vigamox that will achieve a very high therapeutic index with routine q.i.d. dosing in a prophylactic setting for cataract or refractive surgery? Another reason for desiring higher tissue concentrations is to lower the likelihood of developing resistance. Data from the Campbell Lab and other sources has demonstrated the emergence of resistant organisms, particularly gram-positive organisms, against our fluoroquinolones. So now we're talking about achieving antibiotic concentrations that will also prevent mutations in bacteria that confer resistance (or MPC). Typically, the mutation prevention concentration or MPC is three- to fourfold higher than the MIC. Therefore, having higher antibiotic concentrations in target tissues will benefit our patients not only from the standpoint of protecting against infection, but also for prolonging the usefulness of our current fourth-generation fluoroquinolones by preventing the development of resistance.
Dr. Mah: What do you think about that rationale regarding antibiotic penetration, Ralph?
Dr. Chu: I don't always think that if some is good, more is better. We've been really well-educated about penetration from all of the studies comparing Ocuflox and Ciloxan, and the message is, you need to get enough drug inside the eye at adequate concentrations. But now we are reminded that there is toxicity associated with any topical medicine. Penetration at what cost is what also needs to be thought about. The differences in penetration between Vigamox and Zymar can not be solely explained by differences in pharmacokinetics, such as concentration differences and pH. I think toxicity to the epithelium explains why more Vigamox is leaking into the eye compared to Zymar. Frank Bucci performed a study looking at sterilization rates in the anterior chamber of cataract patients who were dosed with either Vigamox or Zymar. He found no difference in bacterial contamination of his anterior chamber aspirates.
Dr. Kim: Ralph's right in that concentration and pH are pertinent factors for penetration for this class of antibiotic. However, molecular structure may be another reason for the superior penetration of Vigamox, but not because of epithelial barrier breakdown. Corneal penetration and permeability studies comparing Vigamox to Zymar have shown that Vigamox penetrates the cornea better without affecting epithelial integrity, presumably due to its inherent molecular structure possessing biphasic properties (Owen, ARVO 2004). But the arrival of IQuix (Santen) at a 1.5% concentration of levofloxacin will generate discussions of whether more is better. And here, the molecular structure is the key difference. No matter how high a concentration this drug will achieve, its clinical efficacy will be limited due to its molecule structure. Levofloxacin is essentially the L-isomer of ofloxacin and lacks the distinguishing structural characteristics of the fourth-generation fluoroquinolones Vigamox and Zymar, such as the C-8 methoxy group substitution. Therefore, its spectrum of coverage will be restricted and not affected by higher concentrations. But it will be formulated as a BAK-free solution, like Vigamox. BAK has been postulated to improve drug penetration by disrupting epithelial tight cell junctions, but since Vigamox does not contain BAK, this should not influence its penetration characteristics.
Dr. Mah: Another issue is antibiotic resistance. There's research showing that in fluoroquinolones at a higher concentration, you can actually prevent mutations such as a resistance mutation. So there's another reason to want more penetration, toxicity aside and assuming spectrum of activity is exactly the same.
Dr. Chu: I think you are able to achieve higher concentrations of either antibiotic by increasing the dosing frequency. An important corollary to this is to not dose at subtherapeutic levels for extended periods as this may increase the development of resistance. An example of this would be using erythromycin once a day for months to treat blepharitis. In this case, the antibiotic has become no more than a lubricant.
Dr. Kim: I agree!
Dr. Mah: I think in general everybody would agree that both drugs are much better than what we had previously in terms of covering gram-positive bacteria, resistant iso;ates and also covering atypical mycobacteria, compared to everything that we had commercially available before.
Dr. Chu: I agree. Given the rising resistance patterns to currently available third-generation fluoroquinolones as your lab and others have shown, clinicians should make the switch to fourth- generation fluoroquinolones. I think the spectrum of coverage is similar for the two drugs in gram positive isolates with Zymar having an advantage with gram negative and atypical organisms.
Dr. Kim: No question our fourth generations are more potent and have a broader spectrum of coverage, especially for atypical organisms and specifically atypical mycobacteria, which have caused an increasing proportion of devastating LASIK-associated infections. But a study from your lab, Francis, (Mather, Am J Ophthalmol 2002), that looked at the third- and fourth-generation fluoroquinolones against human endophthalmitis isolates, did show a statistically significant difference comparing both fourth-generation drugs. The gram positive isolates were more susceptible to Vigamox vs. Zymar in that setting. Everything else was equal.
Dr. Mah: If you review all the literature on Vigamox and Zymar, in general, I think Vigamox has slightly lower MICs against gram-positives in general. Zymar seems to have a slight advantage over Vigamox for gram-negatives. Both do much better than the previous fluoroquinolones in terms of spectrum of activity. The issue is going to be the clinical relevance of those small but definite differences in potency. My gut feeling is that it probably doesn't make much of a difference unless you're talking about endophthalmitis, where you've got lower concentrations getting into the anterior chamber. But on the surface of the eye, in the management of bacterial keratitis, for example, because of our ability to increase the frequency of dosing, I don't really think those small differences probably make a huge difference. This opinion is my gut feeling.
Dr. Mah: BAK is probably the final difference between the two medications. Ralph, talk about BAK and about the benefits or the reasons to have BAK in an antibiotic.
Dr. Chu: I think that BAK in an anti-infective is essential. Many of us have been taught that BAK=BAD, but the studies showing this toxicity were done with concentrations of BAK much higher than those used in most ophthalmic solutions today including Zymar. The concentration of BAK in Zymar is similar to that found in Ocuflox and Ciloxan. With anti-infectives being used with the idea of eradicating organisms and preventing infections, a deliberate decision was made to add BAK to the formulation to protect patients against the risk of bottle contamination especially with fungal organisms such as Candida and Aspergillus. In fact both Zymar and Ocuflox would have met the same USP criteria as Vigamox to be BAK-free or self-preserved.
Dr. Mah: Terry, what are the positives and negatives of BAK?
Dr. Kim: The general trend in ophthalmology over the years has been to move away from potentially toxic preservatives like BAK. Glaucoma medications are moving from BAK to preservatives like Purite. NSAIDs are now available with lower BAK concentrations to improve comfort and tolerability. And even with artificial tears, we are seeing "disappearing" preservatives. I think of Vigamox as being self-preserved, as opposed to "preservative-free" because it did have to pass stringent U.S. Pharmacopeia standards in order to gain that classification. In addition to exceeding USP requirements, further testing was even performed with additional challenge organisms, such as Acanthamoeba, Nocardia, and Fusarium, in order to alleviate the fears of contamination. The arrival of self-preserved antibiotics represents a new standard in antimicrobial therapy. And the reason why this is happening now is because of the enhanced potency of our newer generation fluoroquinolones. When used for surgical prophylaxis, surgeons should also keep in mind that we are also using povidone iodine as the standard of care for cataract and refractive surgery. And in the elective LASIK surgery setting where you really want to make the whole experience as comfortable as possible for the patient, I actually like the fact that there isn't a potentially toxic preservative on board. If it's not needed, why add it?
Dr. Chu: I appreciate Terry's argument but one thing that gets lost is that BAK isn't the only source of toxicity. I don't think BAK, at least at the concentration in these medications, is harmful. As for NSAIDs, reducing the concentration of the active molecule is what has contributed the most to patient comfort.
Dr. Kim: An important point is that, if you look at the USP data for Vigamox in terms of the reduction in colony-forming units, I think Vigamox demonstrated cidal levels, right?
Dr. Mah: You're right. The requirements are stasis, but the Vigamox data did show beyond three logs of kill or a bactericidal effect, for the tested bacteria and fungi.
Dr. Kim: So that's why Vigamox exceeded the USP requirements in the category of preservation. However, this data should not be used to view our fourth generations as anti-fungals or anti-parasitics.
Dr. Mah: Ralph, do you feel it is necessary to have the BAK for the contamination issue?
Dr. Chu: I think there is a risk of bottle contamination especially from fungal organisms with a potential risk for subsequent infection in patients. We have done some work in this area with in vivo models and have shown significant contamination and subsequent keratitis formation when using a BAK-free fourth- generation fluoroquinolone versus a fourth-generation fluoroquinolone with BAK. This data is being submitted for publication.
Dr. Kim: I feel comfortable looking at the USP studies and feel that the chance of fungal contamination is going to be really negligible. You have to determine what is more important to you. Potentially, we can see some toxicity from BAK no matter what the medication, and because we see a lot of our patients who are on multiple medications, BAK-free antibiotics offer an opportunity to avoid a potentially negative factor.
Dr. Mah: Regarding the marketing messages—toxicity or penetration— to differentiate these two obviously excellent antibiotics, which is more important to you clinically?
Dr. Chu: I think the toxicity studies are critical to our understanding of another important aspect of these medications. Inhibition of wound healing should not be forgotten. Multiple animal studies have shown significant toxicity at the epithelium and stromal wound healing levels when using Vigamox. These in vivo results corroborate two prospective randomized human trials. Penetration, although important, is an old message. Both antibiotics have been shown to achieve adequate concentrations to sterilize target issues. It's important to choose an antibiotic that is going to provide protection against a broad spectrum of bacteria and have a favorable pharmacokinetic profile, but also is tolerable and causes the least amount of toxicity.
Dr. Kim: Well, the toxicity message is not convincing to me, mainly because of the lack of proof in human clinical studies and, most importantly, clinical practice. In evaluating the crucial characteristics for our newer antibiotics, I look at the three P's for clinical efficacy: potency, penetration and preservation. Fortunately, we have two very potent fourth-generation fluoroquinolones, and all the in vitro data has supported this fact. I definitely think there's a significant difference between Vigamox and Zymar in terms of penetration, and I feel strongly that penetration remains a very, very important factor for superior performance in the treatment and prevention of infections, which are threatening our cataract and refractive procedures with resistant and atypical organisms. And finally, having an effective mode of preservation that is biocompatible without any potential toxicity is clinically relevant. These are the factors that convince me that Vigamox is an excellent option for having the best protection and insurance against infection.