Q: One of my Medicare claims was denied and now I need to appeal. How does the Medicare Appeals process work?
A: Not every claim you file with Medicare will go through smoothly the first time, but in many cases it’s obvious to your billing staff what went awry. In that situation, fixing the issue and resubmitting or re-opening the claim may result in correct processing and proper payment without a formal appeal. Sometimes, however, a paid or submitted claim is reviewed by a payer and formally denied. Denials after a review by your Medicare contractor can happen for a number of reasons:
- Diagnosis not on payer list for coverage. If a doctor has chart documentation that says a patient has a certain disease, and that disease isn’t on the payer list for coverage, then the service you delivered (e.g. surgery, diagnostic test or exam) is considered non-covered.
- Medical necessity considerations—even with a proper diagnosis. Most often, these occur when the payer’s published guidance isn’t followed, or proper documentation isn’t used (even if there isn’t published guidance).
Check the chart when the payer says you have an incorrect diagnosis; some services are published as only covered for certain specific diagnoses. If your patient has noncovered diagnosis “X,” and the payer allows only “A, B or C” for payment, then this isn’t an appeal you’re likely to win—although you can write to the Medicare Contractor requesting this be a covered diagnosis in the future.
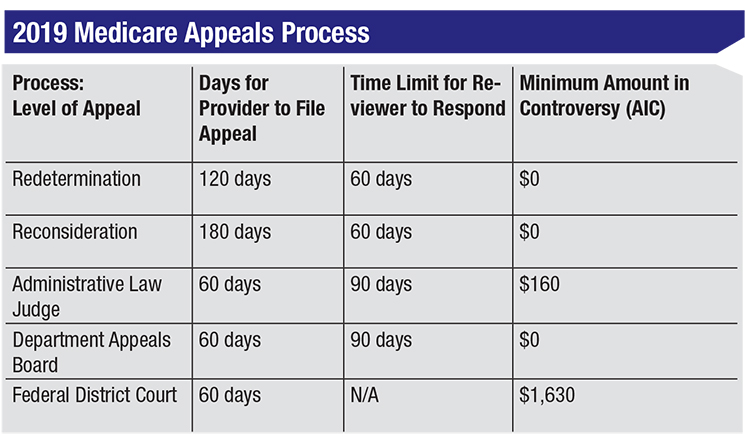
Formal denials for medical necessity or lack of documentation require more work. Medicare has an official process with various levels of appeal.
 |
Q: I found out I have to appeal something formally. What’s the first level of the appeal process?
A: The first level of appeal is known as Redetermination. You can access the CMS-20027 form on your local Medicare Administrative Contractor’s website or get it directly from CMS. (You can do it without the form but it isn’t advised since you might leave something out.) CMS notes, “A redetermination is a review of the claim by Medicare Administrative Contractor (MAC) personnel not involved in the initial claim determination.”
Once you receive the Remittance Advice, you have 120 days to file according to the RA’s date of receipt. CMS notes that it’s assumed you received the RA five days after the date listed on the notice. Your MAC will also inform you, “If you wish to avoid recoupment from occurring you need to file your request for redetermination within 30 days from the date of this letter as described above.” Note that the date on the letter is not the date you are assumed to have received it—an important distinction.
Recoupment means that if you don’t pay the demand in full, the owed money will be subtracted from other payments you’ll get. Importantly, interest begins accruing on any balance, even if you elect to stop recoupment, and it’ll continue to accrue until you finally win (in which case it would go away in full), or lose (in which case you would owe it all plus the interest). The interest rate in effect is 10.75 percent (simple, not compound).
CMS adds that you should include “any and all documentation that supports the argument against the previous decision.” Leave out anything that doesn’t help your argument. This information (chart, op note, test result, anything you write, etc.) is sent with the form to the MAC that made the original determination. The sending address can be found on the MAC website, in the Redetermination process section. Keep a complete copy of what you send. There isn’t a minimum dollar amount regarding the amount in controversy that’s needed to file. You can mail or send your packet electronically, but regardless of how it’s sent, be sure to get a return receipt so you know it was delivered.
Q: I lost a first-level appeal. What can I do next if I want to pursue it further?
A: Your MAC will have notified you via a Redetermination Notice as to whether or not the decision was in your favor. If the decision was unfavorable, you can forgo the appeal process and have it recouped gradually, pay it in full, or go to a second-level appeal known as Reconsideration. Again, CMS assumes you’ve received the notice five days after the date listed. Be sure to see if the denial is for the same reason, and if not, address it carefully. There’s a different form for second-level appeals—CMS-20033. Your MAC can provide instructions and forms, or you can download the documents from CMS.
You have 180 days to file a Reconsideration based on the date listed on the notice received, but recoupment will begin no earlier than 60 days from the date on the letter, unless you notify them. This appeal doesn’t go to your MAC; instead it goes to a Qualified Independent Contractor (QIC). Again, there’s no minimum amount in controversy required to file an appeal, but this is likely your last chance to send any new information that could help your case. CMS notes, “Any documentation not submitted at the reconsideration level may be excluded from consideration at subsequent levels of appeal …” They add, “The reconsideration decision will contain detailed information on further appeals rights, where applicable.”
Q: I lost part of the second-level appeal. What’s next?
A: If your Reconsideration goes unfavorably, in full or part, you can proceed to a third level of appeal—an Administrative Law Judge (ALJ) hearing—but recoupment begins immediately. A third form is needed, the OHMA-100, and you have 60 days from the receipt of the QIC notice to file. There must be at least $160 in controversy and it’s unlikely that additional information can be submitted.
There are fourth and fifth levels of appeal, but they are rarely required. At the fifth level, you must file within 60 days and have at least $1,630 in controversy. The appeal is filed with the Federal District Court, and it’s a good idea to have a lawyer represent you.
Q: Can you summarize how to be successful when formally appealing?
A: Successful appeals require paying close attention to payer guidance, if it exists, and meeting medical necessity requirements. Reasons for any denials are important to address, as subsequent rounds of appeal might not be denied or questioned for the same reason(s).
The required timelines to return your information and (separately) avoid recoupment require monitoring, as these change based on the level of appeal. REVIEW
Mr. Larson is a senior consultant at the Corcoran Consulting Group. Contact him at plarson@corcoranccg.com.



