Fuchs’ endothelial corneal dystrophy is the most common indication for corneal transplantation in the United States, and surgical management of this disease has undergone a revolution during the past 20 years.1 Though endothelial keratoplasty is a highly effective treatment, investigators are searching for alternative treatment options because of the worldwide shortage of donor corneas and the risks associated with donor transplantation.
“Standard of care is partial-thickness corneal transplantation, typically the endothelium only,” says Kathryn Colby, MD, PhD, chair of ophthalmology at the University of Chicago. “We still do way more Descemet’s stripping endothelial keratoplasty (DSEK) in the United States than Descemet’s membrane endothelial keratoplasty (DMEK). In 2014, I performed my first case of Descemet’s stripping only (DSO), and we published our initial case series in 2016. Since then, it has really taken off. This is a simple technique, which involves removing the dysfunctional central corneal endothelial cells to allow healthier peripheral cells to migrate in. There is no long-term steroid use, no glaucoma and no chance of rejection. It’s a really wonderful technique.”
Descemet’s Stripping Only
Although early case series on Descemet’s stripping have yielded variable results, many more positive than negative outcomes have now been published, suggesting that this is indeed a promising technique for the treatment of Fuchs’ endothelial corneal dystrophy, which would reduce the rate of surgical complications, eliminate the risk of rejection and lessen the demand for donor tissue.2
Dr. Colby’s initial case series found that repopulation of the central corneal endothelium with corneal deturgescence can occur after deliberate central Descemet’s stripping in patients with Fuchs’ endothelial dystrophy who underwent cataract removal.3
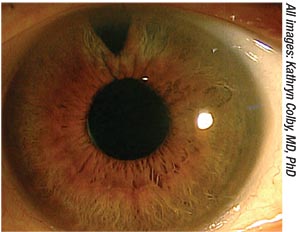 |
| Figure 1. Slit lamp photo of a Descemet’s stripping patient more than four years after surgery. |
In this retrospective case series, patients with Fuchs’ endothelial dystrophy and visually significant cataract underwent phacoemulsification. After intraocular lens insertion, 4 mm of the central Descemet’s membrane was stripped and removed. Vision assessment, corneal pachymetry and confocal imaging of the endothelial anatomy were performed preoperatively and 1, 3, 6 and 12 months postoperatively. Patients were classified as fast responders, responders, slow responders or nonresponders on the basis of postoperative time to resolution of corneal edema with demonstration of a visible central endothelial mosaic.
The study included 13 eyes of 11 patients, who ranged in age from 51 to 91 years. Preoperatively, no eyes had countable central endothelial cells by confocal imaging, and visual acuity ranged from 20/25 to 20/400. At days one and seven postoperatively, all corneas showed stromal and microcystic edema in the area of Descemet’s stripping. Four eyes demonstrated resolution of corneal edema with a visible central endothelial cell mosaic (range: 410 to 864 cells/mm2) by postoperative month one, with visual acuity ranging between 20/25 and 20/40. Four additional eyes demonstrated a similar response by postoperative month three, and an additional two eyes had resolution of corneal edema with an intact central endothelial mosaic at postoperative month six or later. Cell counts (range: 428 to 864 cells/mm2) were maintained in all 10 responders at the last follow-up visit, which occurred between postoperative months six and 24. Final vision ranged from 20/15 to 20/20 in these 10 eyes, with the exception of two eyes with retinal pathology. Three eyes required endothelial keratoplasty. Dr. Colby’s first Descemet’s stripping patient will reach the five-year mark in January 2019 and is still doing well with no signs or symptoms of endothelial dysfunction.
According to Christopher J. Rapuano, MD, chief of the cornea service at Wills Eye Hospital in Philadelphia, surgeons are still trying to determine the best instrumentation and candidates for this technique. “It works great, but it may not work forever. After a few years, the cells may die off, and patients may need an endothelial keratoplasty. However, there is a benefit to delaying it even a few years, and you can always do DSEK or DMEK later on,” he says.
Adjunctive Use of ROCK Inhibitors
Rho kinase (ROCK) inhibitors have been used in combination with Descemet’s stripping. A recent study comparing Descemet’s stripping and DMEK included three patients who elected to apply a topical ROCK inhibitor (ripasudil 0.4%), which could potentially improve healing.2
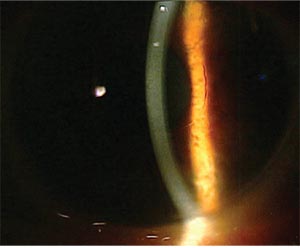 |
| Figure 2. An image of the same patient from Fig. 1, showing the edge of Descemet’s stripping and clear cornea. |
The study found that Descemet’s stripping effectively treats select patients with mild to moderate Fuchs’ dystrophy, with visual outcomes equivalent to DMEK. While the recovery time with Descemet’s stripping may be longer, these patients had fewer adverse events and less need for additional procedures. Additionally, they didn’t need long-term immunosuppression or donor corneal tissue.
This retrospective comparative cohort study included 27 eyes with mild to moderate Fuchs’ dystrophy (with corneal guttae/edema limited to the central cornea with relatively clear periphery). All procedures were performed at the University of Pittsburgh Medical Center between 2015 and 2017. Fifteen patients underwent DMEK, and 12 patients underwent Descemet’s stripping.
At the end of phaco, 4 mm of diseased Descemet’s membrane was removed. Visual acuity was measured using the Snellen chart and then converted to logMAR for analysis.
The average postoperative pinhole visual acuity was 20/25-1 (logMAR 0.16 ±0.09) for DMEK eyes and 20/30+1 (logMAR 0.13 ±0.10) for Descemet’s -stripping eyes. The average time to 20/40 vision was 2.2 ±2.8 weeks for DMEK eyes and 7.1 ±2.7 weeks for Descemet’s-stripping eyes. In the DMEK group, adverse events included: seven had increased intraocular pressure, one had anterior chamber inflammation, and one had graft nonadherence, with one patient (6.7 percent) requiring anterior chamber paracentesis and another (6.7 percent) requiring a rebubbling procedure. Patients in the Descemet’s-stripping group experienced no adverse events.
Another Descemet’s-stripping study included two cases that had been rescued by topical ripasudil.4 This Australian study found that descemetorhexis without grafting is a viable procedure for patients with Fuchs’ dystrophy with visual degradation due to central guttae. While careful patient selection is required, the researchers note that the advent of topical ripasudil as a salvage agent suggests that a broader application of the surgery may be possible.
This study included 12 eyes of 11 patients who underwent central descemetorhexis that didn’t exceed 4 mm. All patients had visual symptoms that were a result of Fuchs’ dystrophy. Corneal status and visual parameters were recorded monthly until corneal clearance was observed. After corneal clearance, they were recorded every six months. Cases that failed to clear by month two were considered for salvage treatment, which consisted of a ROCK-inhibitor eye drop. Endothelial keratoplasty was planned as the final salvage procedure in unsuccessful cases.
Of the 12 eyes, nine (75 percent) cleared spontaneously between two and six months. One eye failed to clear by month five, and the investigators administered topical Y-27632, a compounded ROCK inhibitor, without success. Endothelial keratoplasty was performed.
In two eyes, corneal healing stalled at two and three months. In both cases, complete corneal clearance was achieved by administering topical ripasudil six times a day for two weeks. In cases achieving corneal clearance, best-corrected visual acuity improved from a mean of 0.26 to 0.125 (logMAR) with subjective improvement in quality of vision.
Cultured Cells + ROCK Inhibitor
Another new procedure is the injection of cultured cells in combination with a ROCK inhibitor.5 This procedure has been investigated by Japanese surgeon Shigeru Kinoshita, MD, PhD, and colleagues.
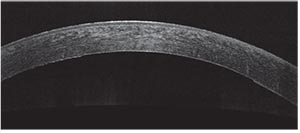 |
| Figure 3. Anterior segment OCT showing the edge of Descemet’s stripping. |
“It’s been performed in a variety of ways over the years, in animals and then in early human studies,” Dr. Rapuano explains. “Endothelial cells are taken from a donor or from the patient undergoing treatment, and brought into the lab. Then, a ROCK inhibitor is used to help multiply the cells. You can take a small number of cells and expand them many times. They can then be implanted in multiple patients. The cells are injected into the patient who then has to lie face down for a few hours. Theoretically, gravity forces those cells to stick onto the endothelium and then grow and repopulate to eliminate Fuchs’ dystrophy corneal edema.”
This same concept can be applied to cells from other parts of the body. “This can theoretically also be done with skin cells or lip cells. Additionally, to avoid rejection, the patient’s own cells can be harvested and expanded in the lab. Once you’ve expanded a few cells to hundreds or thousands of cells, you can put all of them back in the eye. There is no chance of rejection and no need for long-term steroids,” he adds.
Dr. Kinoshita recently published a study that found that the injection of human corneal endothelial cells supplemented with a ROCK inhibitor resulted in an increase in corneal endothelial cell density after 24 weeks in 11 people with bullous keratopathy.5 It’s well known that corneal endothelial cell disorders, such as Fuchs’ endothelial corneal dystrophy, induce abnormal corneal hydration that results in corneal haziness and vision loss, known as bullous keratopathy.
In Dr. Kinoshita’s study, the bullous keratopathy patients had no detectable corneal endothelial cells. Human corneal endothelial cells were cultured from a donor cornea. The researchers supplemented a total of 1 × 106 “subcultured” cells with a ROCK inhibitor and injected the cells into the anterior chamber of the eye that had been selected for treatment (subculture is used to prolong the life and/or expand the number of cells or microorganisms in the culture). Patients then remained in a prone position for three hours. The primary outcome was restoration of corneal transparency, with a corneal endothelial cell density of more than 500 cells per square millimeter at the central cornea at 24 weeks after cell injection. Secondary outcomes included corneal thickness of less than 630 μm and improvement in best-corrected visual acuity equivalent to two lines or more on a Landolt C eye chart at 24 weeks after cell injection.
At 24 weeks after cell injection, all of the treated eyes had a corneal endothelial cell density of more than 500 cells/mm2 (range: 947 to 2,833), and 10 eyes had a corneal endothelial cell density exceeding 1,000 cells/mm2. Ten of the 11 treated eyes achieved a corneal thickness of less than 630 μm (range: 489 to 640), and nine of the eyes achieved an improvement in BCVA of two lines or more.
The Future
According to Dr. Colby, even with these exciting new treatment options, endothelial keratoplasty is here to stay. “For other forms of endothelial dysfunction besides Fuchs’, either a tissue or a cell transplant will be required,” she says. “Additionally, patients who have advanced Fuchs’ will not be able to be successfully treated with Descemet’s stripping, because the disease is just too far gone. These patients don’t have enough healthy peripheral cells to repopulate.”
Another important area of research is the pathogenesis of Fuchs’ corneal endothelial dystrophy.1 A better understanding of the pathogenic mechanism of the disease will hopefully allow for the development of medical therapies to treat or prevent this condition in the future, experts say.
1. Sarnicola C, Farooq AV, Colby K. Fuchs endothelial corneal dystrophy: Update on pathogenesis and future directions. Eye & Contact Lens. July 12, 2018. E-pub ahead of print.
2. Huang MJ, Kane S, Dhaliwal DK. Descemetorhexis without endothelial keratoplasty versus DMEK for treatment of Fuchs endothelial corneal dystrophy. Cornea. September 14, 2018. E-pub ahead of print.
3. Borkar DS, Veldman P, Colby KA. Treatment of Fuchs endothelial dystrophy by Descemet stripping without endothelial keratoplasty. Cornea 2016;35:10:1267-1273.
4. Moloney G, Petsoglu C, Ball M. Descemetorhexis without grafting for Fuchs endothelial dystrophy—Supplementation with topical ripasudil. Cornea 2017;36:6:642-648.
5. Kinoshita S, Koizumi N, Ueno M, et al. Injection of cultured cells with a ROCK inhibitor for bullous keratopathy. New England Journal of Medicine 2018;378:11:995-1003.



