A number of new procedures and devices for treating glaucoma are currently in use or under investigation. One of the most promising, and one that I have used extensively, is the Trabectome. The Trabectome is a handheld instrument (approved by the Food and Drug Administration) that treats glaucoma by using microelectrocautery to ablate a strip of tissue from the trabecular meshwork and Schlemm's canal, allowing the aqueous direct access to the eye's drainage system. Manufactured by NeoMedix in
Using the Instrument
The Trabectome is inserted into the eye through a clear corneal incision; it is positioned across the anterior chamber, and the tip is inserted through the trabecular meshwork into Schlemm's canal. (See second illustration below.) The bent tip, which contains the electrodes, is coated on the back with a smooth insulating material. This creates a protective footplate that prevents the heat generated during electrocautery from damaging nontargeted tissues. It also guides the tip smoothly through Schlemm's canal, while ablating the targeted trabecular and juxtacanalicular tissues. Simultaneous irrigation and aspiration remove the debris and maintain a stable anterior chamber.
Technically, the Trabectome procedure is a trabeculectomy ab interno. It's one of the newer trabecular surgeries, or internal filtering procedures, as I call them (to help differentiate them from external filtering procedures such as trabeculectomies and tube shunts). The Trabectome procedure is in the same class as trabecular stenting procedures, canaloplasty, viscocanalostomy and excimer laser trabeculostomy.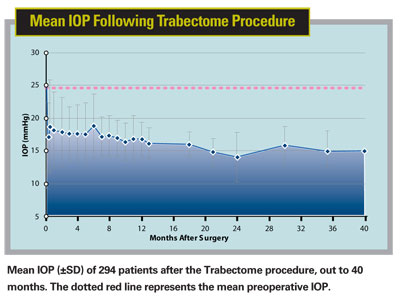
The main issue for surgeons interested in using the Trabectome is that it's a different type of surgery, performed using a gonioscopic approach. In this procedure you place a gonio lens on the eye, with the eye and head tilted away from you. The microscope is also tilted to provide a direct view of the anterior chamber angle while you're doing the procedure.
This approach is similar to other glaucoma procedures done in children, such as goniotomy; it's quite different from standard surgery for glaucoma or cataract in which the surgeon is accustomed to looking directly down through the microscope into the eye. However, once you're used to it it's no more difficult than other intraocular procedures.
Multiple Advantages
Use of the Trabectome offers several benefits compared to other surgical approaches commonly used to treat glaucoma:
• It removes the source of greatest outflow resistance. The inner wall of Schlemm's canal and the adjunct trabecular meshwork are thought to be the area of greatest resistance in the outflow pathway. The ablation caused by the Trabectome exposes the aqueous in the anterior chamber directly to the outflow collector channel, increasing the flow of aqueous.
• It doesn't cause scarring. Because the Trabectome uses electrocautery to ablate a strip of tissue instead of simply making a slit-type incision, the two flaps are widely separated. As histological studies have confirmed, this helps to prevent healing and scarring.
• It preserves the conjunctiva. Unlike other procedures that access Schlemm's canal using an external approach, the Trabectome doesn't sacrifice any of the conjunctiva. The conjunctiva remains untouched, an advantage if the patient should someday require filtering surgery.
• It's faster and less risky than trabeculectomy. In addition to requiring less time to complete, the follow-up is less rigorous. The Trabectome procedure avoids most complications associated with trabeculectomy, such as hypotony, choroidal effusion, flat anterior chambers, leaking blebs and the risk of infection due to bleb leakage in the late postop period.
When to Use It
In my experience, the Trabectome is a good option as an initial surgical intervention for glaucoma. Its effectiveness and safety profile make it a better choice than many existing alternatives. In fact, it could be a viable surgical option earlier in the disease than most other surgical interventions would even be considered.
For example, if a patient is on multiple medications and you're looking for a way to lower the number of meds and still maintain effective IOP control, the Trabectome should be considered as a stand-alone procedure—even in a patient who is relatively well-controlled. This is especially true if the patient is having side effects from the medications, has cost issues or isn't compliant. (In contrast, I would hesitate to perform trabeculectomy on a glaucoma patient in this situation because of the risks involved.)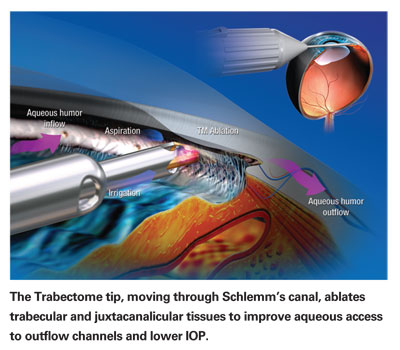
The Trabectome is also a good option to combine with phacoemulsification and cataract removal in order to control glaucoma. Combining the Trabectome with cataract removal adds minimal risk to the procedure; in contrast, combining cataract with trabeculectomy adds significant risk. We're currently doing an analysis of the effectiveness of combining the Trabectome procedure with phacoemulsification surgery in 58 patients. Mean preop IOP was 19.7 ±6 mmHg; at six months, mean IOP is 15.0 ±3 mmHg.
We recommend this procedure for any of the open-angle glaucomas, including primary open-angle glaucoma, pseudoexfoliation glaucoma and pigmentary dispersion glaucoma. The procedure also works well in patients with chronic angle-closure glaucoma with goniosynechiae. In fact, I've used the procedure in combination with goniosynechialysis. The gonio lens lets you do the goniosynechialysis under direct visualization to open up the angle; then you perform the Trabectome procedure.
In terms of contraindications, there are a few situations in which I might not choose to use the Trabectome:
• When the angle view is obscured. You have to have a reliable, clear view of the angle in order to perform this procedure, so you couldn't do this in a patient who has corneal opacity, significant scarring or a very abnormal angle.
• When a large pressure drop is needed. If a patient has advanced glaucoma and you want the pressure lowered into the 10- to 12-mmHg range, the Trabectome is probably not the best option to use. Because the Trabectome procedure is not an external filtering surgery and is limited by episcleral venous pressure, it usually doesn't lower pressure quite as far as a successful trabeculectomy. So in this situation, trabeculectomy may be more advantageous.
• If the patient has had prior filtering surgery. If a patient has had a prior failed trabeculectomy or tube shunt procedure, it's unclear how the eye will respond to the Trabectome.
What's Next?
In the long run, the Trabectome should be a valuable option for general ophthalmologists, as a way to surgically treat glaucoma at an earlier stage. But right now, efforts are focused on working toward a large, multicenter trial, and training a large nucleus of glaucoma specialists in the use of the device.
Eventually, we plan to conduct a randomized trial comparing the Trabectome with a gold standard such as laser trabeculoplasty or trabeculectomy (probably the latter). We also plan to explore which medications work best in conjunction with the Trabectome. Finally, we'll be investigating the efficacy that can be achieved if the surgeon makes more than one incision. (We're able to remove 90 to 100 degrees of the trabecular meshwork with one incision; we don't know how the pressure drop will be affected if we make multiple incisions and remove more tissue.)
If you'd like to learn more about the Trabectome, training sessions including a didactic and wet lab will soon be offered in several locations around the country, as well as at the upcoming
Dr. Francis is associate professor of ophthalmology on the glaucoma service at the Doheny Eye Institute, Keck School of Medicine,



