The differential diagnosis included arteritic ischemic optic neuropathy (AION), non-arteritic ischemic optic neuropathy (NAION), papillitis and intraorbital mass lesion. Laboratory evaluation demonstrated normal platelets, ESR and CRP. Spectral domain optical coherence tomography showed right optic nerve edema most prominent inferiorly and nasally. OCT of the left eye was normal. The macular OCT was normal.
|
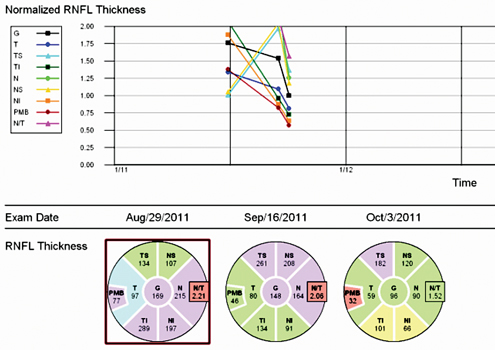
Two weeks after presentation, the patient noted worsening of his symptoms. Visual acuity was 20/40 and color plates 2/8 in his right eye. Two weeks later, the patient’s symptoms were unchanged and his visual acuity was 20/50 and color plates stable at 2/9 in the affected eye. Repeat OCT showed resolving edema of the right optic nerve and later testing revealed thinning in the affected area demonstrated on serial retinal nerve fiber layer thickness maps (See Figure 2).
Repeat Humphrey visual fields continued to show a dense right superior altitudinal defect with somewhat poor testing parameters. The patient also reported that his sleep study demonstrated obstructive sleep apnea and that he was being fit for a CPAP (continuous positive airway pressure) mask for home use. The patient was diagnosed with NAION and advised to discontinue his use of erectile dysfunction medications and to follow-up for his sleep apnea treatment.
Discussion
Multiple risk factors for developing NAION have been described in the literature. Some of these risk factors overlap with other vasculopathic disease processes, such as diabetes, hypertension, atherosclerosis and hyperlipidemia. Other associated causes include collagen vascular disease, antiphospholipid disease, anemia and cataract surgery. Medications that have been associated with NAION include amiodarone and, more controversially, erectile dysfunction medications. Classically, the patient has a “disc at risk,” which can often be appreciated by a small cup-to-disk ratio in the unaffected eye. It is believed that this “crowding” of the optic disc makes the optic nerve more vulnerable to ischemic events in high-risk individuals. In the case described above, the patient did not have the classic disc at risk in his fellow eye, so this finding should not be considered an absolute for the diagnosis of NAION. The majority of NAION is classified as non-progressive; however, two studies, one by Lanning B. Kline, MD, and another by Mark Borchert, MD, and Simmons Lessell, MD, demonstrated that 25 percent of patients develop progressive NAION with worsening vision for three to four weeks after the insult, as observed in this patient.
Howard Pomeranz, MD, PhD, and colleagues described one of the first case series, consisting of five patients that developed NAION subsequent to their use of sildenafil, a phosphodiesterase inhibitor. Four of the five patients had no vascular risk factors and developed loss of vision within 24 hours of ingestion. Since then, other reports of vision loss following ingestion of these medications have prompted the Food and Drug Administration to issue a warning of the possible association of NAION with erectile dysfunction medications.
More recently, obstructive sleep apnea (OSA) has been strongly associated with the development of NAION. In a study by Karine Palombi, MD, et al., sleep apnea was found to be 1.5 to twofold more frequent than the rate of the other identified risk factors typically associated with NAION, such as hypertension and diabetes. In this study, OSA was found to be the most frequent disorder associated with NAION and routine screening was recommended for all patients with NAION. Jian Li, MD, PhD, and colleagues evaluated the utility of sleep apnea screening questions, such as the Sleep Apnea Scale of the Sleep Disorders Questionnaire (SA-DQS). This study was inconclusive, and the authors suggested that further research needed to be done in larger populations to validate the use of such questionnaires in patients with NAION.
The purpose of screening for sleep apnea in patients with NAION extends well beyond ophthalmic complications and vision loss. Obstructive sleep apnea has been independently linked to a host of systemic disorders including: hypertension; myocardial ischemia; stroke; arrhythmias; and fatal and nonfatal cerebrovascular disease, each of which may cause significant morbidity and mortality. In a more recent study, Louis P. Voigt, MD, and colleagues showed that patients with OSA had a longer QT dispersion as measured on a standard surface electrocardiogram, which may serve as a marker for increased risk of sudden cardiac death. REVIEW
The author would like to thank Robert Sergott, MD, Wills Eye Institute Neuro-ophthalmology Department, for his time and assistance.
1. Borchert M, Lessell S. Progressive and recurrent nonarteritis anterior ischemic optic neuropathy. Am J Ophthlamol 1988;106:443-9.
2. Kline LB. Progression of visual defects in ischemic optic neuropathy. Am J Ophthalmol 1988;106:199-203.
3. Li J, McGwin G Jr, Vaphiades MS, Owsley C. Non-arteritic anterior ischaemic optic neuropathy and presumed sleep apnoea syndrome screened by the Sleep Apnea scale of the Sleep Disorders Questionnaire (SA-SDQ). Br J Ophthalmol 2007;91:1524-1527.
4. Palombi K, Renard E, Levy P, Chicquet C, Deschaux Ch, Romanet JP, Pepin JL. Non-arteritic anterior ischaemic optic neuropathy is nearly systemically associated with obstructive sleep apnoea. Br J Ophthalmol 2006;90:879-882.
5. Pomeranz HD, Smith KH, Hart WM, Egan RA. Sildenafil-associated Nonarteritic Anterior Ischemic Optic Neuropathy. Ophthalmology 2002;109:584–587.
6. Voigt L, Haq SA, Mitre CA, Lombardo G, Kassotis J. Effect of obstructive sleep apnea on QT dispersion: A potential mechanism of sudden cardiac death. Cardiology 2011;118(1):68-73.