In what felt like an almost complete return to normalcy, in the first week of May, the Association for Research in Vision and Ophthalmology held its first live meeting in three years. Though virtual meetings were serviceable, there’s nothing like being present in the poster hall and circulating amid the presenters, or catching a podium presentation live and in-person. If you weren’t able to make it to this year’s meeting in Denver, here’s a look at some interesting presentations from the gathering.
• Online AREDS vitamins. Researchers say it’s “buyer beware” when your patients shop online for AREDS-formula ocular supplements.
Researchers searched “AREDS” and “AREDS2” on Amazon and Google Shopping. They checked each product in the top 30 results (besides promoted ones) for compliance with the AREDS2 formula, allowing for both low (25 mg) and high (80 mg) zinc formulations. They also found the price per daily serving for each product and compared the prices of “compliant” vs. “non-compliant” formulas.
They found that 30.8 percent (37/120) of the products didn’t adhere to the AREDS2 formula, and 5.8 percent (7/120) followed the AREDS1 formula, which the researchers note is no longer recommended since it results in an increased risk of lung cancer for smokers. Products that deviated in any way from the AREDS2 formulation were 26 percent more expensive than those that didn’t. Also, products that were missing at least one of the ingredients in the AREDS2 formula were 26.9 percent more expensive than those that had the ingredients. The researchers say that “clinicians may wish to be specific in their recommendation of AREDS2 formulations to avoid inaccurate dosing.” (Yu J. ARVO Abstract F0189, 2022)
• Novel visual acuity measurement. A group of investigators say it may be possible to measure a patient’s visual acuity without actual VA testing. They found that a person’s answers to a series of yes/no questions about their vision can be used to estimate their VA, which might have implications for tele-ophthalmology exams in the future.
In the study, 333 patients with a mean age of 57 from four different testing sites responded to a set of 100 yes/no questions designed to assess acuity in recognizing familiar objects, such as silverware on a table, at typical viewing distances with normal to ultra-low vision.
Measured VA values were available from all participants and converted to logMAR units, and it turned out that the percentage of “yes” responses answered by each participant was significantly correlated with his or her VA. A strong relationship, was also found between participants visual ability estimate from the two-parameter model and their VA. The average prediction error, calculated by the absolute difference between the predicted VA and the actual VA, was 0.23 logMAR.
| Review’s on Instagram! Stop by Review of Ophthalmology’s new Instagram account @revophth and see what’s new! |
The researchers say that the results show that a questionnaire can be useful in estimating VA worse than 20/40. (Wu Y-H. ARVO Abstract [Paper] Estimating visual acuity without a visual acuity chart, 2022)
• New approach to complex IOL calculations. Researchers from the University of Ghent say cataract surgeons might be able to accurately predict IOL powers in post-LASIK patients using an experimental ray-tracing technology.
The study looked at 75 patients with previous myopic or hyperopic LASIK who underwent cataract surgery. The surgeons entered the patients’ anterior and posterior corneal Zernike coefficients, corneal thickness, postoperative effective lens position and vitreous chamber depth, and IOL geometry into an optical design software program called Zemax (Radiant Zemax; Focus software), which is usually used for imaging and illumination systems. Using this software, the researchers built patient-specific eye models and calculated the resulting optical quality.
The surgeons found agreement between the predicted refraction of the proposed optimized methodology for IOL power calculation and the postoperative subjective refraction. Average spherical equivalent was -0.36 ±0.80 D (subjective) and -0.35 ±0.73 D (predicted). The percentage of eyes within ±0.5 D was 82.6 percent (M), 84.1 percent (J0) and 82.6 percent (J45), while the agreement within ±1 D was 93.3 (M), 98.6 (J0) and 97.3 percent (J45). (Perez-Merino P. ARVO Abstract F0417, 2022)
• Long-term Luxturna. The revolutionary ophthalmic gene therapy Luxturna (voretigene neparvovec; Spark) has been available for several years now for patients with RPE65-mediated inherited retinal dystrophy, and a group of researchers in the PERCEIVE study are starting to report its long-term effects.
In the study, 103 treated patients were followed for five years. At the most recent follow-up, 35 patients (34 percent) reported ≥1 ocular AEs including 17 with ocular “adverse events of special interest” (16.5 percent). Chorioretinal atrophic change events (at the injection site and/or elsewhere [13]) were most common. Ocular AESIs included foveal degeneration (4), vitritis (4), inflammation (3), retinal tear (2) and increased intraocular pressure (5).
Two patients had serious ocular AEs (one patient with inflammation, and one with increased IOP). Non-ocular AEs occurred in 80 patients, with the most frequent being headache (4). One patient, with no previous history, reported three psychiatric events. Visual function improved in terms of full-field light sensitivity threshold, and best-corrected visual acuity improved at Year 2, with a mean change from baseline of -13.67 ±22.62 decibels.
The researchers say chorioretinal atrophy has been identified as a new adverse reaction, but so far hasn’t been associated with vision loss. (Fischer MD. ARVO Abstract [Paper] PERCEIVE Study Report, 2022)
• Artificial intelligence in glaucoma management. Researchers from Johns Hopkins trained an AI system to catch visual field worsening, and compared the machine’s results to those of clinicians using area under the receiver operating characteristic curve analysis.
Out of 8,705 eyes, 869 (10 percent) were found to have worsening fields over time. The Deep Learning Module had an AUROC of 0.94 (1.00 is perfect) for detecting worsening of visual fields on the test set, compared to just 0.63 for the clinician decisions. The researchers say that DLM may allow for earlier detection of progression, and that existing VF progression-analysis software might benefit from the additon of a DLM. (Hau K. ARVO Abstract A0455, 2022)
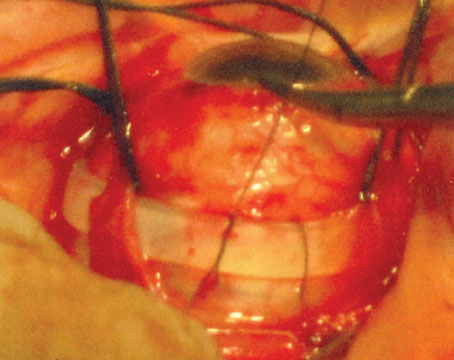
• Predicting the outcome of retinal detachment repair. Investigators from Toronto say that you may be able to use early postop imaging to determine who’ll get the most visual benefit from the detachment repair.
The researchers retrospectively analyzed 614 eyes of 614 patients who underwent primary rhegmatogenous retinal detachment repair, and tested their vision, metamorphopsia and anisekonia at three months postop. They also imaged them with spectral-domain OCT and fundus autofluorescence imaging.
Regression analysis found that significant early postop imaging predictors of visual acuity were discontinuity of the external limiting membrane (p=0.01) and presence of retinal vessel printings on FAF (p=0.033). Discontinuity of the interdigitation zone was a significant predictor of metamorphopsia (average of MH+MV (p=0.008) and presence of RVPs was a significant predictor of aniseikonia (p=0.04). In the study, the researchers say, “Modifications of surgical techniques aimed to reduce postoperative discontinuity of the outer retinal bands and retinal displacement may improve functional outcomes after retinal detachment repair.” (Lee WW. ARVO Abstract [Paper] Imaging Predictors of Functional Outcomes Following Rhegmatogenous Retinal Detachment Repair, 2022)
• Macular atrophy progression in different forms of AMD. Researchers looked into the progression of macular atrophy in patients with AMD. They analyzed two groups: 91 patients without MA at baseline (in order to study time to first MA development in treated and fellow eyes); and 47 patients with a total of four years of follow-up, in order to study the time course and growth rate of MA in treated and fellow eyes.
They found a significant difference in MA incidence and progression in eyes with nAMD treated with anti-VEGF agents compared to fellow eyes exhibiting dry AMD. They say that treated nAMD eyes tended to develop MA more often, and the MA progressed at a faster rate in these eyes compared to fellow dry AMD eyes. (Tsilimbaris M. ARVO Abstract A0455, 2022)