The choice a cataract surgeon makes when confronted with an eye that has little to no capsular support is the source of one of ophthalmology’s most heated debates. Should an anterior chamber lens be inserted, or would one of the many posterior chamber lens fixation techniques work better? These days, most surgeons would probably opt for the latter option, leaving the humble ACIOL fighting to maintain relevance in a fixation-friendly world.
We asked cataract surgeons to discuss the risks associated with AC-IOLs, the instances when they may actually be preferred over a posteriorly fixated lens and why all anterior segment surgeons—including residents—should continue to keep this technique in their toolkit. Read on for what they had to say.
The Risks vs. Reality
There are a few reasons ACIOLs carry some inherent risks, according to surgeons.
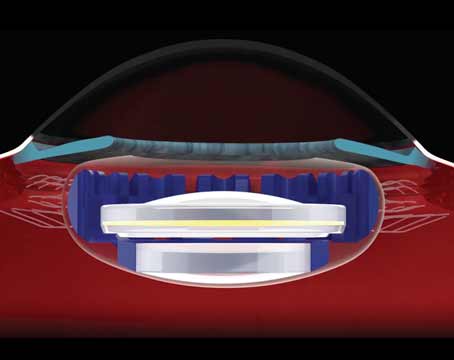
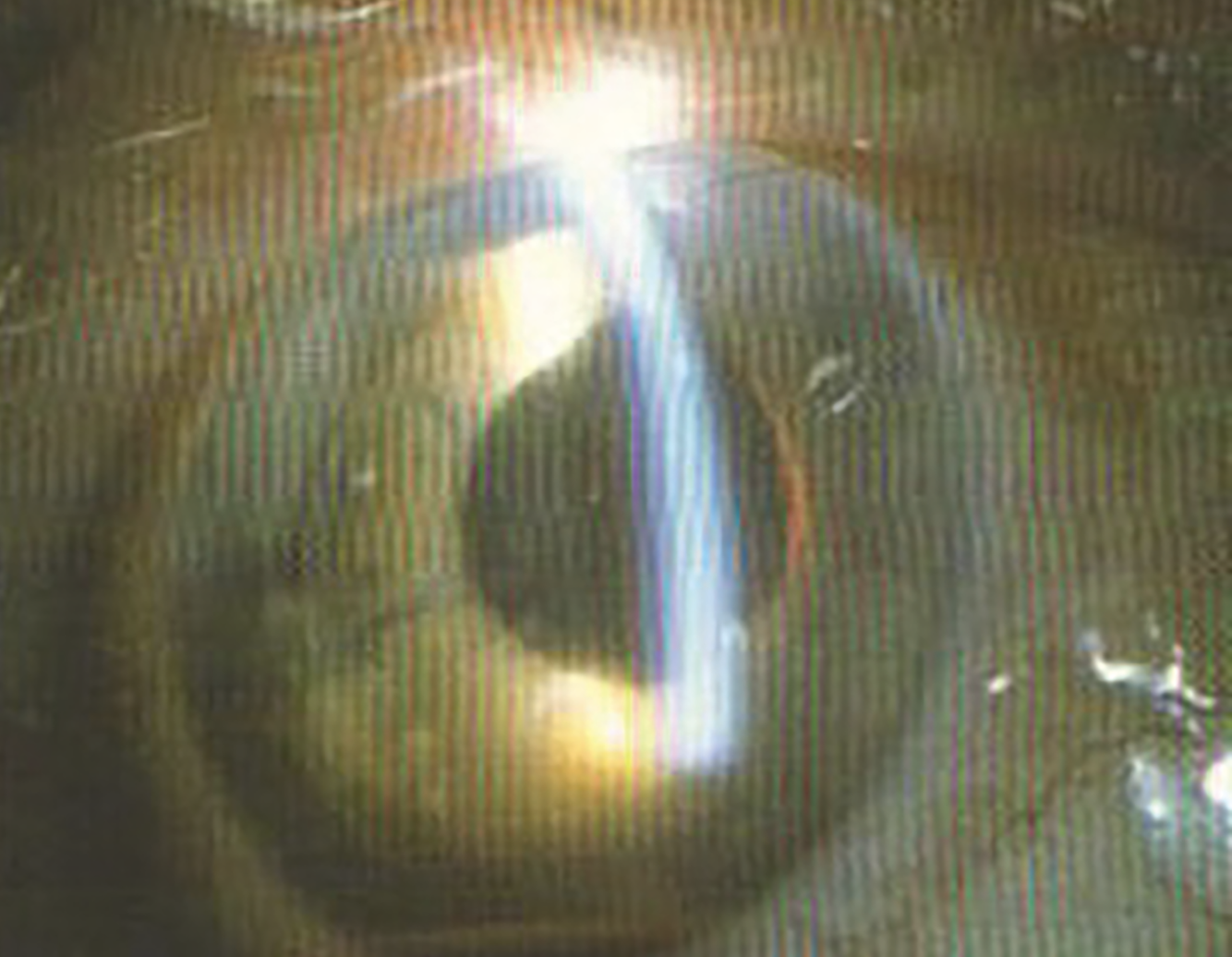 |
| Uveitis-glaucoma-hyphema syndrome was a common complication caused by ACIOLs and is often cited as a reason to avoid implanting them. Photo: Richard Packard, MD, FRCOphth. |
Physiologic location is one. “Some of the issues that surround the use of ACIOLs are related to the placement of the lens in the anterior chamber in front of the iris that puts it in closer proximity to the cornea,” says Mark Kontos, MD, a cataract and refractive surgeon in Washington state. “In patients who may have initial weaknesses to the cornea, such as Fuchs’ dystrophy, having an anterior chamber lens close can sometimes precipitate problems with the cornea to where they develop cloudiness that’s unable to resolve. There’s also a risk of developing a persistent corneal edema or other issues that could be problematic for the vision. In patients who are younger, having an anterior chamber lens could be a problem for them as far as the health of their cornea as they grow older.”
Others highlight the design of the lens as its biggest fault. Early ACIOL designs featured rough edges on the haptics, which caused damage to the cornea and gave rise to the flexible-loop ACIOL. Uveitis-glaucoma-hyphema syndrome was one of the most common complications associated with ACIOLs due to its contact against the iris, although the condition has become more rare as phaco techniques have evolved.1
“With the evolution of PCIOLs and extracap, ACIOLs were reserved for use in the event of complications—broken capsule, displaced nucleus, vitrectomy,” says Douglas K. Grayson, MD, who is a cataract and glaucoma specialist practicing in New Jersey, as well as an attending surgeon at New York Eye and Ear Infirmary. “Surgeons would implant an ACIOL as a last resort. The cornea was already obscured, the patient was uncomfortable and it was more about getting a lens in and finishing the case. In those scenarios, AC-IOLs were suboptimal—they caused synechiae, UGH syndrome, CME and secondary glaucomas. Those were situations where a lens probably shouldn’t have been placed at all. The patient should have been left aphakic and brought back another day under control to have a lens implanted.”
Dr. Kontos says incision size also contributes to complications. “In order to place this lens, you have to make a pretty large incision—5.5 to 6 mm,” he explains. “That can create irregular astigmatism to the cornea or create difficulties with the wound, such as wound leaks. Because the lens rests on the iris, it can sometimes cause abnormalities in the shape of the pupil that aren’t necessarily a functional problem, but cosmetically they could be an issue for the patient. Sometimes you can get persistent inflammation because of the haptics touching on the iris in such a way that creates an inflammatory response.”
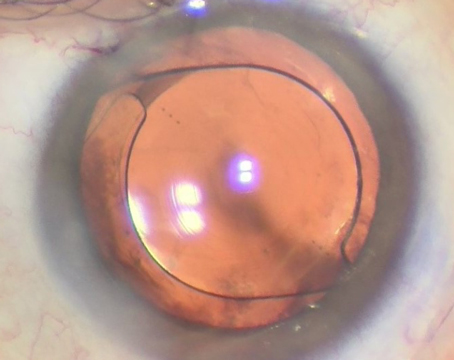
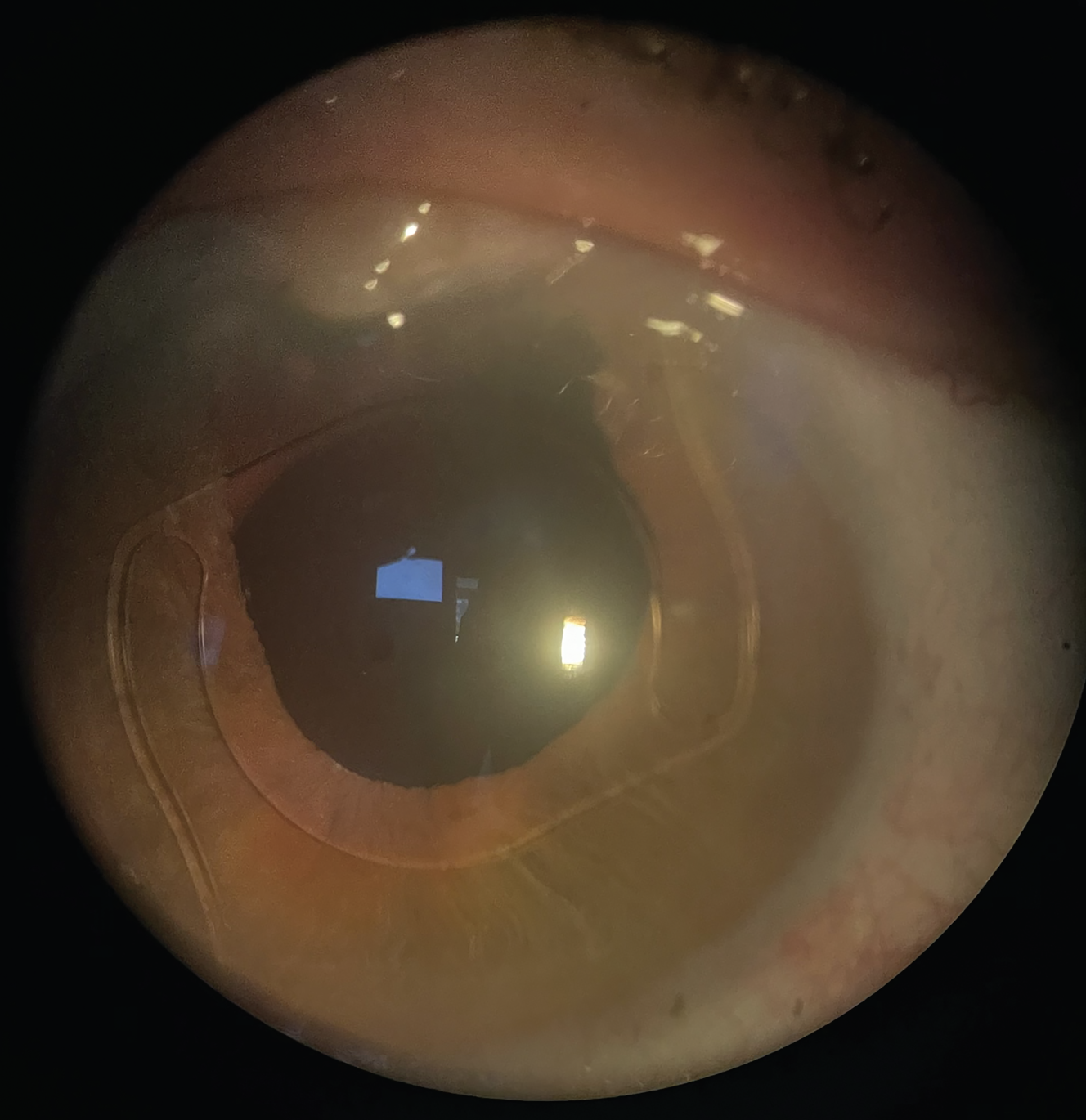 |
| A well-positioned ACIOL with superior iridectomy and filtering bleb. Photo: Douglas K. Grayson, MD. |
ACIOL sizing is another concern of Richard Packard, MD, FRCS, FRCOphth, who now consults for Arnott Eye Associates in London. “If it’s too small the lens can propeller inside the eye and damage the endothelium ,” he says. If your peripheral iridectomy doesn’t work well, the iris can bulge around the IOL. The iris could also fixate around the haptics so it decenters the pupil. All manner of things could happen.
“However, if you compare the results in outcomes, there isn’t that much of a difference,” he continues. “It’s a moot point.”
Several studies support this. In 2005, researchers at Bascom Palmer Eye Institute compared the clinical outcomes and complications of patients who received an ACIOL vs. a sutured PCIOL after cataract surgery resulting in poor capsular support. They concluded that there were no significant differences in outcomes and went as far as to say that “a reconsideration of ACIOL condemnation is warranted” and “placement of an ACIOL may be considered a comparable, or even favorable, alternative [to transsclerally sutured PCIOLs] depending on the surgeon’s training and patient characteristics.”2
Approximately 15 years after that was published, an updated study reinforced the continued safety profile of ACIOLs. Published in 2020, a retrospective case study of 45 peer-reviewed pieces of literature evaluated eight different types of IOL fixation techniques:
• ACIOL;
• iris-claw IOL;
• retropupillary iris-claw IOL;
• 10-0 polypropylene iris-sutured posterior chamber IOL;
• 10-0 polypropylene scleral- sutured PCIOL;
• 8-0 polypropylene scleral-sutured PCIOL;
• CV-8 polytetrafluoroethylene; and
• intrascleral haptic fixation.
Evidence showed no superiority of any single technique, and researchers determined each one had equivalent visual acuity outcomes, safety profiles and its own risks of postoperative complications.3
Joanne Shen, MD, an ophthalmologist at the Mayo Clinic in Scottsdale, Arizona, and a coauthor of that study, says the current ACIOL design available is the least traumatic in its evolution. “Our study did show that there may be some higher association of cystoid macular edema and anterior chamber inflammation with an ACIOL,” she notes. “This is obviously because of where the IOL sits, and this research wasn’t a clinical trial so we’ll never have definitive data to say ACIOLs are unsafe or safe. You can’t say it across the spectrum.”
Appropriate Times to Use an ACIOL
Despite the increasing popularity of PCIOL fixation techniques, the cataract surgeons we spoke with say there are plenty of reasons to keep ACIOLs in the realm of options for patients lacking capsular support.
“I’ve always maintained that in a controlled circumstance, anterior chamber lenses of modern design are excellent if you measure for the correct size,” says Dr. Grayson. “They’re put in as a secondary procedure where the person’s already aphakic, and they’re very well-tolerated. If they’re placed in the angle correctly, they don’t cause corneal decompensation. Any problem that may be related, such as CME, which can’t be resolved with medications or injections, you have a very clear-cut source you can look with and say, ‘Aha, see this one haptic may be a little bit off and that may be causing it.’ So you could do a secondary procedure to rotate the anterior chamber lens and relieve that source of irritation. So, the AC lens is a very useful tool.”
For Dr. Kontos, any decision depends on the situation, and often age is a large part of it. “Every case is going to be a unique scenario, and in certain scenarios, I think using an anterior chamber lens is perfectly fine,” he says. “As long as the patient has a relatively healthy cornea, has a large or deep anterior chamber, and there aren’t any other issues going on, such as vitreous in the anterior chamber, you can probably use an ACIOL and do fine with it, especially in older patients. In a patient who’s in their late 70s or 80s, doing a simple surgery with an ACIOL can sometimes be a lot easier than going through the more complex surgery when you have to suture a posterior chamber lens. There can be situations where, during cataract surgery, the case can become complicated and perhaps you have no capsular support and have lost the lens into the back of the eye or something, you could place an anterior chamber lens if everything else is okay. This way you at least get a lens in the patient so that they could be functional. It’s important to have ACIOLs available in the operating room area, just in case of that emergency situation.”
Dr. Grayson poses an example of a scenario when an ACIOL could be the best option. “If a patient had a displaced PCIOL that had been in place for 15 years,” he says, “and, say, due to pseudoexfoliation, the one-piece lens had to explanted. So, the lens is explanted, you wait about a month until the cornea is clear and everything’s calm. Now you can put in an ACIOL, after measuring carefully and picking the right size. That’s one clinical scenario where it was an uncomplicated removal of a displaced one-piece lens, and they just have a nice AC lens and they can move on.”
Dr. Shen says she also considers the patient’s proximity to the clinic. “If you practice in a rural area, you may never see that patient again,” she says. “It’s likely they’re going to go back and see their local optometrist or other non-surgeon. This is important because the downside of some of these newer fixation techniques is they have erosions of the sutures or the haptic. This requires monitoring.
“On the other hand, with an ACIOL, you don’t have to monitor them as closely to make sure nothing’s peeking out of the surface that might allow bacteria to enter into the eye and cause endotheliitis and blindness,” she continues. “I personally have some patients who live about three to four hours away. I’m probably not going to be able to see them every six months, realistically. I also think about if they’re in a nursing home; if they have dementia. These are things that we as surgeons have to factor in.”
ACIOLs also require very few instruments to insert, Dr. Shen notes. “We have to factor in what our operating room has,” she says. “Do we have all the instruments and the technology to do some of these newer techniques of suturing, such as the Yamane technique and scleral fixation? You can’t just perform those with the bare bones like the ACIOL, which doesn’t require much technical equipment. It’s pretty straightforward.”
“There’s much more that has to take place for choosing a PCIOL,” says Dr. Kontos. “It requires more skill on the part of the surgeon and there’s a lot of variability that can occur. There can be problems with erosion of the haptics, or other issues that can create problems and the need to go back and do revision surgery. If you can avoid all of those things by doing a simpler surgery that the patient can tolerate, then I think it’s a perfectly appropriate course of action.”
PCIOLs and the various fixation techniques have their own drawbacks. “We’re seeing a lot of these fixation techniques creating some of the same problems as the first generation of PCIOLs did, including tilt, CME, erosions, UGH syndrome,” says Dr. Grayson. “There are a fair number of Yamane revision cases that have been sent to me.”
Dr. Shen says the scleral-fixated techniques don’t work well if a patient has had trauma, leaving the wall of their eye damaged and thinned. “If the sclera has been damaged, you may not have anything to sew to,” she says. “Imagine you’re trying to hang a picture on a wall, but every stud has been eaten by termites, so you don’t know where to hang it on the wall.”
She’s also concerned about the amount of torque these PCIOLs are undergoing. “These lenses aren’t designed to be torqued in this manner with the haptics that are typically supposed to be in one plane being bent forward,” says Dr. Shen. “What are we going to see in 10 years? Time will tell. Ultimately, none of these IOLs have been FDA labeled for these insertion techniques, including the sutured IOLs. If you look at the FDA labeling, there isn’t anything that says, ‘This is how you sew it on, this is what you use to sew it on.’ That was never discussed in the labeling.”
Surgeon Skills and Access
Even though surgeons can make the case for ACIOLs, they acknowledge the gap in training and access to the product.
“When I was training in the ’90s, ACIOLs were the standard,” says Dr. Shen. “If you couldn’t put a lens in the bag or in the sulcus, you did an ACIOL. I’m in my 50s now, so for me and others in this generation and above, we’re still comfortable with this procedure. But the newer generations, they’re also learning eight different types of IOL fixation techniques, with different types of sutures and lenses.”
It’s also not incredibly common to run into this type of complication during residency.
“It’s probably difficult to learn in residency because the opportunities to place an anterior chamber lens are limited, and in a lot of residencies, you may not see one because of just how advanced cataract surgery has gotten over the years,” Dr. Kontos says. “The need to place an ACIOL is so much more rare than it used to be. When I was a resident, it was just something you were definitely going to see and do at some point. But now it’s really not quite that way. It’s very conceivable to imagine an ophthalmology resident going through their entire residency without seeing an ACIOL placed. If that’s the case, it behooves you to learn and have some sense of it because I think it’s a skill that’s important to have. Just like anything, there’s going to be a time or two where that makes the most sense for the patient, and it’s a good idea to be able to have the ability to do it.”
“Younger ophthalmologists in training who have a complication where parts of the nucleus are going posteriorly, the previous generation would have maybe converted to an extracap procedure and tried to remove that nucleus in total to prevent posterior displacement, and possibly have them put in an ACIOL if things were calm enough, or we’d come back and do the AC lens two or three weeks later,” says Dr. Grayson.
“But what happens now is, when a complication occurs with the nucleus going posteriorly, they’ll close and defer to retina,” he continues. “In the previous days, retina would remove the nucleus and then send it back to the anterior segment surgeon to do some form of a lens. Now, retina specialists are trained in doing these sutured secondary lenses. I try to get my residents at New York Eye and Ear to at least become familiar with it so they know how to use it. But I think the anterior segment surgeons are losing their secondary lens skills.”
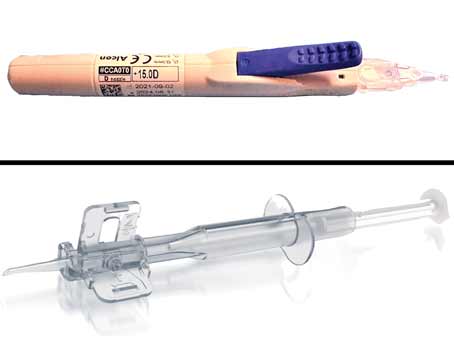
There’s also the matter of keeping ACIOLs on hand for surgeries. Currently, only Alcon and Bausch + Lomb manufacture these lenses. Dr. Packard says surgeons should have a bank of them ready, with at least three sizes for each IOL power.
“It’s never going to be commonplace, but I think there’s always going to be a place where an anterior chamber lens is an appropriate option for a patient, as opposed to the sutured IOL,” says Dr. Kontos. “When you’re doing cataract surgery and you’re not really anticipating the need for one, it’s a good idea to just use them as part of your planning process to say, ‘Okay, if something catastrophic were to occur here and I can’t get a lens into the posterior chamber or posterior capsule area or sulcus fixed, can I put an anterior chamber lens in this patient? Do we have them available in the surgery center if I need it?’ ”
“Pre-planning for an AC lens will lead to successful use of the lens,” seconds Dr. Grayson. “In a complicated cataract procedure that’s gone on for an hour, don’t try to just jam in a lens. Leave the patient aphakic, let everything clear, let the cornea clear, let the eye heal, and then another day you can do an AC lens with a vitrectomy if you need to, or you could do a pre-planned sutured lens.
“But the point of it is, and I teach residents this, if things have gone badly and it’s an extended period of time, never be afraid to just hold off on the lens, wait until things cool down, and then go on and do your lens later,” he continues.
Surgical Pearls
Technique is important for ACIOL success, so we asked these surgeons to share their top tips:
• Sizing and lens power. Dr. Packard says correct lens sizing is critical. “If it’s too small it could be more dangerous because it will propeller inside the eye and damage the endothelium,” he says. “You could use standard calipers to measure white to white and wound size, Stahl caliper, Kelman dip stick or OCT. You also need to remember to recalculate your A-constant.”
• Wound construction. Dr. Kontos says it’s best to make a temporal wound for these lenses. “It’s important to be able to have good wound construction,” he says. “You want to make sure that you don’t have a shallow wound that can allow the haptic of the anterior chamber lens to get caught into the wound. You want to make sure that you’ve gone into the cornea a little ways so you have a posterior lip when you insert the lens, that it’s going to be wedged back into the proper place in the angle, and it doesn’t have an easy way to slip right up into the wound. Make sure that the wound is well-sealed at the completion of the surgery.”
“I use a 6-mm, peripheral clear corneal incision for the AC lens, rather than doing a scleral tunnel,” says Dr. Grayson. “It gives you better visibility, placement and angulation to put the lens in. Close the wound with three sutures, and on a peripheral corneal wound, you don’t induce astigmatism, and patients do very well.”
• Constrict the pupil. “Another pearl involves constricting the pupil so that the iris is somewhat taut when you insert the lens,” says Dr. Kontos. “It’s a good idea to use Miochol for these cases to try and constrict the pupil as much as you can. It makes it a much easier process, and it’s less likely to get the iris hung up on the haptics as you’re sliding the lens in.”

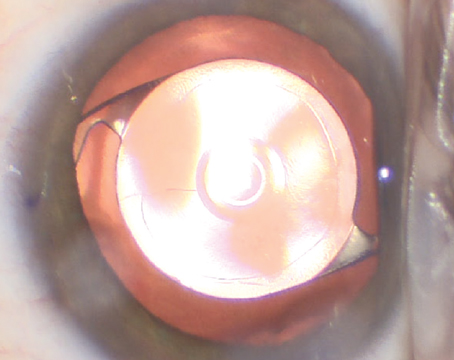
|
| Surgeons say a Sheets glide is a handy tool for ACIOL insertion as it helps create a scaffold to slide the lens into place. Photo: Richard Packard, MD, FRCOphth. |
• Visualization. Dr. Kontos says to make sure the placement of the haptics are in the angle above the iris and not rubbing up against the cornea or caught up and entangled into the iris itself. “The haptics should be resting on the surface of the iris and not embedded in the iris in any way,” he says. “It’s helpful to use a Sheets glide, which acts as a scaffold by which you can slide the lens into place, and then you can remove that fairly easily. That’s a good technique and a good piece of equipment to have handy if you’re going to be using an anterior chamber lens.”
• Peripheral iridectomy/iridotomy. Dr. Grayson says, “In any secondary lens procedure, a peripheral iridectomy is important, whether it’s done by laser or surgically.”
“It’s something that can be simply done at the temporal wound area,” adds Dr. Kontos. “You can just grab a piece of proximal iris that’s close to the angle and make a small little cut with Van Ness scissors, and that gives you a peripheral iridectomy to eliminate any possibility of angle closure.”
“You can do your peripheral iridectomy quite easily with a vitreous cutter,” suggests Dr. Packard. “You just turn the cut rate down to as low as you possibly can, use a bit of suction on the iris for a split second on the foot pedal, and you’ve got your iridectomy.”
• Lens orientation. If placing the lens temporally, rotating it with the haptics oriented vertically is a good idea, suggests Dr. Kontos. “That also helps to make sure that the lens haptics are seated properly, making sure that you’re placing the lens in the right configuration,” he says. “It does have a right-side up. The lens is vaulted slightly anteriorly. So it’s important that when the lens is being inserted, that you’re inserting it in such a way that the anterior vault is facing outward towards the surface of the cornea. If you place it inverted in the other way, then it’s going to be pressing down into the iris, and that’s going to create some problems over the long term.”
• Check for vitreous. Before completing the case, use triamcinolone to ensure no vitreous is left in the anterior chamber, recommends Dr. Packard.
In conclusion, Dr. Packard says, “Whoever you are as a surgeon, you should have your ‘Get Out of Jail Free’ technique for when things have gone significantly pear-shaped, and you don’t have anything to support a lens by way of the capsule. You should feel competent and comfortable with this technique so when things go bad, you know you can still end up giving the patient a satisfactory outcome."
Dr. Grayson consults for Alcon, Glaukos and Johnson & Johnson Vision. Dr. Kontos is a consultant for Alcon. Dr. Packard has no relevant disclosures. Dr. Shen has no financial disclosures.
1. Sen S, Zeppieri M, Tripathy K. Uveitis Glaucoma Hyphema Syndrome. [Updated 2024 Feb 29]. In: StatPearls [online publication]. Treasure Island, FL. StatPearls Publishing 2024.
2. Donaldson KE, Gorscak JJ, Budenz DL, Feuer WJ, Benz MS, Forster RK. Anterior chamber and sutured posterior chamber intraocular lenses in eyes with poor capsular support. J Cataract Refract Surg 2005;31:5:903-9.
3. Shen JF, Deng S, Hammersmith KM, Kuo AN, Li JY, Weikert MP, Shtein RM. Intraocular lens implantation in the absence of zonular support: An outcomes and safety update: A report by the American Academy of Ophthalmology. Ophthalmology 2020;127:9:1234-1258.