ƒImprovements in the currently available multifocal and accommodative lenses are leading to better visual outcomes and greater patient satisfaction. At the same time, those improvements are changing which options are likely to work best in different situations. Here, four experienced surgeons share their latest thinking on the currently available presbyopic lenses and the factors—physical, medical and lifestyle-related—that cause them to favor one lens option over another.
Managing the New Multifocals
Scott MacRae, MD, in practice at the Strong Vision Refractive Center in Rochester, N.Y., and professor of ophthalmology and visual science at the Flaum Eye Institute, University of Rochester, says that 50 to 60 percent of his patients end up with a presbyopic lens. Although he favors the Crystalens, he acknowledges that multifocals may be the better option in some situations, and sees advantages to each of the multifocal options.
“We’ve studied the presbyopic lenses in our optics lab,” he says. “In our studies the ReSTOR +4.0 and the Tecnis [+4.0] multifocal have similar optimal near points that are a little bit closer than the ReSTOR +3.0. But the Tecnis multifocal also has a modest intermediate peak, giving the patient a little bit of intermediate focus as well.” (See chart, facing page.)
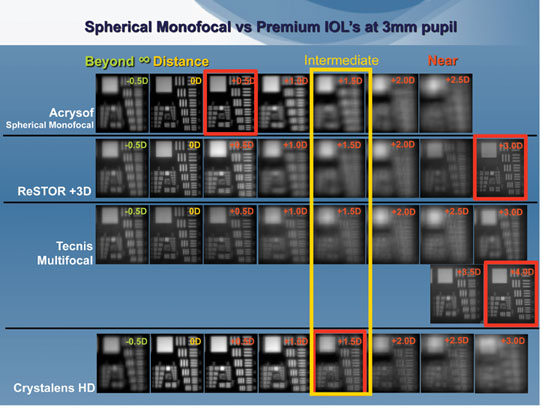 |
| Optical bench testing of IOLs in a wet cell IOL mount indicates that the Crystalens HD has the best intermediate-distance contrast with a 3-mm pupil. The near peak for the ReSTOR +3.0 is at +3 D, while the Tecnis Multifocal near peak is at +4 D. Note the mild intermediate peak at +1 D for the Tecnis multifocal. (Testing conducted at the Flaum Eye Institute, University of Rochester.) (Image courtesy Scott MacRae, MD.) |
R. Bruce Wallace III, MD, FACS, founder and medical director of Wallace Eye Surgery in Alexandria, La., and clinical professor of ophthalmology at the Louisiana State University School of Medicine in New Orleans, agrees. (According to Dr. Wallace, because his practice is located in a less-affluent part of the country, only about 10 percent of his patients choose a presbyopic lens.) “We were an investigative site for both lenses and we learned early on that the intermediate vision is better [with the Tecnis],” he says. “Also, the Tecnis is now in a single-piece platform, which appeals to many surgeons.”
Jason E. Stahl, MD, practices at DurrieVision in Overland Park, Kan., and is assistant clinical professor of ophthalmology at the University of Kansas; his practice specializes in eliminating the need for spectacles and doesn’t accept Medicare, so he almost exclusively implants either toric or presbyopic lenses. Dr. Stahl says that when choosing between the ReSTOR +3.0 and the Tecnis +4.0, the decision is based on the patient’s needs. “If the patient wants a little bit closer working distance, we’ll go with the Tecnis multifocal,” he explains.
Carlos Buznego, MD, in practice at the Center for Excellence in Eye Care in Miami and a volunteer assistant professor of ophthalmology at the Bascom Palmer Eye Institute, says his practice currently implants about 20 percent of cataract patients with presbyopic lenses; about 15 percent of this group receive a Crystalens, while the other 85 percent get the ReSTOR. Dr. Buznego believes multifocal lenses have gotten a bad reputation because of past problems with visual quality that are mitigated in the latest versions. “My lens of choice is the ReSTOR aspheric +3.0 lens, or SN6AD1,” he says. “I prefer the +3.0 because it has a smaller add than the +4.0 of both the previous ReSTOR and the current Tecnis multifocal. This allows patients to have a slightly longer working distance, thereby providing excellent near vision in addition to strong intermediate vision.”
Crystalens Pros and Cons
Dr. MacRae favors the Crystalens. “My premise is optimizing visual quality for the rest of the patient’s life,” he explains. “Some of these patients are going to get diabetes, macular degeneration, glaucoma or dry eye. Any of those things will degrade retinal image quality. If you’ve already degraded it a little bit with a multifocal, that will be challenging for their visual system.”
Dr. Buznego says that multifocal lenses are his first choice, but when he’s worried about contrast sensitivity or other multifocal issues, the Crystalens is his backup. “The Crystalens gives excellent distance and intermediate vision with workable near vision and a long working distance,” he notes. “However, a significant number of Crystalens patients will need low-add reading spectacles for small print.” Dr. Buznego has tried all of the versions of the Crystalens and now uses the aspheric model.
Dr. Wallace also prefers the AO. “With the AO Crystalens, we’re seeing better consistency of near vision and better consistency of IOL power calculation,” he says. “We now consider using it more often.”
Dr. Stahl uses all of the presbyopic IOLs. “There isn’t a one-size-fits-all lens,” he points out. “They’re all very good, although each of them has strengths and weaknesses. When choosing which lens to use in a good candidate, I think it comes down to spending time talking to the patient and finding out his visual needs.”
Lifestyle and Lens Choice
Patients who are good candidates for presbyopic lenses may present under many different circumstances. Those circumstances often influence which lens surgeons recommend.
• Patients with strong near needs.
“Worldwide, patients are expressing much greater interest in good intermediate and near vision than in years past,” notes Dr. Wallace. “Everyone uses devices like cell phones and iPads, both for work and leisure.”
Dr. Stahl says that if reading and doing near work without correction is very important to the patient, he’ll discuss multifocals—if the patient understands that there will be some loss of contrast sensitivity and halo issues at night. “On occasion we’ll do a combination of a multifocal in one eye and a Crystalens in the other eye,” he says.
Dr. Buznego agrees. “With multifocal IOLs, I routinely have patients who are J1 or J2 uncorrected within days of surgery.”
“We tell our patients that 80 to 90 percent will see well at intermediate with the Crystalens, but only about 30 to 40 percent will be able to see up close for sustained periods without using reading glasses,” says Dr. MacRae. “Actually, 50 to 70 percent of these patients can read without glasses, but the percentage drops when you’re talking about sustained reading for an hour or two. The multifocals will increase this number to 90 percent, but there is a loss of distance contrast.”
• Patients used to reading without glasses. “We ask low myopes whether they take off their glasses to read in bed at night,” says Dr. Wallace. “If the answer is yes, they’re going to want the same quality of near vision they’ve been enjoying without glasses. (By way of comparison, almost any technology will make most low hyperopes happy.) We’re careful to counsel them that this will be different from what they’ve had most of their life. We tell them they’ll probably have better distance vision than they’ve had for years, but the new near vision may have to be learned over time.”
Dr. Stahl agrees. “These patients are less impressed with what presbyopic lenses can do, and they may be disappointed at how their near vision changes,” he says. “You have to stress the distance vision and overall functionality they’re gaining. They should be able to do 90 percent or more of their activities without glasses.”
• Patients who work in dim light. “If the patient needs better near or reading vision in a dimmer environment, we’ll consider the Tecnis multifocal,” says Dr. Stahl. “The Tecnis works better in dim light because it’s not pupil-dependent. In the ReSTOR, the diffractive optic is only in the central 3.6 mm, so if you have a big resting pupil or work in a dimmer environment where your pupil is larger, the ReSTOR will be more distance-dominant, less near-dominant. In the Tecnis multifocal, the multifocality is spread across the entire lens.”
Dr. Wallace agrees that the Tecnis multifocal gives better near vision in dimly lit areas than the ReSTOR, but notes that the Crystalens also has low-light advantages because near vision won’t be affected much by the light level. Dr. Buznego says he also recommends a pseudoaccommodative lens
if a patient has a working situation with poor light.
• Night drivers and pilots. Surgeons agree that these patients are poor candidates for multifocals. “For those patients, if I’m going to use a presbyopic IOL, I’ll go with a Crystalens,” Dr. Buznego says.
Dr. Wallace concurs. “The halo effect of the Tecnis and ReSTOR multifocal is not as bad as we saw with other products, but it’s still there.” Dr. Stahl also wouldn’t recommend a multifocal for a truck driver or commercial pilot, though he says his practice has sometimes implanted a multifocal lens in someone who is a recreational pilot.
Dr. Wallace notes that some patients will do a lot of night driving and still want great reading vision. “In that situation, we can either do micro-monovision—give them a little myopia with a Crystalens in the second eye—or put something like a Tecnis multifocal or a ReSTOR in the other eye, which should give them more dependable near vision,” he says. “We might start with a Crystalens and see how they do.”
• Patients who didn’t like bifocal glasses. “A patient who had significant problems getting used to bifocals, whether progressive or standard, has already demonstrated an inability to adapt to a different visual system,” observes Dr. Wallace. “We’d be careful with those patients and maybe not recommend a presbyopic lens.”
• Previous monofocal contact lens wearers. “Some patients who have had problems wearing contact lenses are halo-phobic or glare-phobic,” notes Dr. Buznego. “I recommend the Crystalens for those patients, which has resulted in a good level of success.”
• Previous multifocal contact lens wearers. “Individuals who were successful multifocal contact lens wearers are very good candidates for presbyopic lenses,” says Dr. Wallace.
Dr. MacRae agrees, but feels this is somewhat unpredictable. “These patients are obviously highly motivated and they’ve already proven that they have reasonable plasticity,”he says, “so they’d probably do well with either a multifocal or mini-monovision using the Crystalens. My preference would be for the latter.”
Any correlation is less clear when a patient’s trial of multifocal contact lenses didn’t work out. Dr. Stahl notes that he’s never found any positive or negative correlation with how well they adapt to a multifocal IOL. Dr. Wallace agrees. “Multifocal implants don’t have the same characteristics as multifocal contact lenses—they don’t depend on hydration as much, and they don’t move on the eye,” he says. “So, some patients who didn’t like multifocal contact lenses will be successful with a multifocal IO. Nevertheless, we proceed with caution.”
• Patients accustomed to monovision. “We typically won’t recommend multifocal lenses for patients who have been successful with monovision contact lenses,” says Dr. Wallace. “Instead, we try to duplicate their contact lens monovision with monofocal lenses. We’ve had a few patients like this who wanted the multifocal lenses because they’d heard about them; but they weren’t as happy with multifocals.”
Dr. Buznego agrees. “Don’t argue with success if you have a patient who is happy with monovision,” he says.
At the same time, some surgeons prefer to recreate the monovision effect using the Crystalens. “These patients are well-suited for mini monovision with the Crystalens, and they do really well,” says Dr. MacRae. “One of the advantages of the Crystalens is that you can use a smaller amount of monovision. Because of the optics of the lens, you can use 0.75 D of monovision and the patient gets the same effect as if you had done 1.5 D with a monofocal lens. That allows him to get better distance vision in the eye with the Crystalens HD, with its greater depth of focus, compared to a monofocal; he’s not so nearsighted in that second eye.”
Optical Factors and Lens Choice
Medical and optical conditions also affect surgeons’ lens choices:
• Previous refractive surgery. “I
do a lot of refractive lens exchange and cataract surgery in patients who have had refractive surgery,” says Dr. Stahl. “For those patients I almost exclusively use the Crystalens AO.”
Dr. MacRae says he wouldn’t put a multifocal lens in most post-LASIK eyes. “It can work, but it often doesn’t,” he notes. “Unless the patient had a low LASIK correction that used a wide optical zone, you’ll be adding a multifocal implant to a multifocal cornea. That spells an unpredictable outcome.”
Whether the previous LASIK was myopic or hyperopic may also make a difference. “The change in asphericity caused by myopic LASIK means that most of these patients would benefit from an aspherical multifocal IOL,” notes Dr. Buznego. “The one specific situation where I would avoid aspheric IOLs is in patients who’ve had hyperopic LASIK. With these patients, I’d use a standard, spherical multifocal IOL such as the older version of the ReSTOR IO, the SN60D3.”
When choosing a presbyopic lens for a former RK patient, surgeons also warn against choosing a multifocal. “We don’t want to reduce contrast sensitivity in patients who’ve already lost some,” says Dr. Wallace. “Plus, these patients already have a multifocal cornea.” Dr. Buznego agrees, but notes that the multifocality of an RK cornea may actually complement the effect of a Crystalens, resulting in improved near vision.
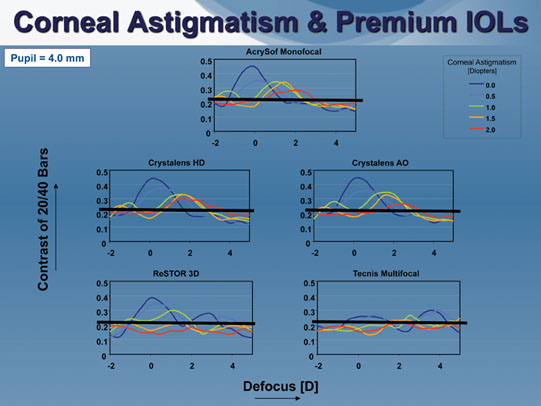 |
| Optical bench testing shows that multifocals are more susceptible to image quality loss with higher levels of corneal astigmatism. Corneal astigmatism reduces image contrast moderately with the monofocal AcrySof and the Crystalens HD and AO, but image quality still remains above the 20/40 contrast threshold. With the ReSTOR +3.0 and the Tecnis mulitfocal, image contrast drops below the 20/40 threshold with more than 1 D of astigmatism. (Testing conducted at the Flaum Eye Institute, University of Rochester.) |
• Severe dry eye. “I’m going to treat that preoperatively,” notes Dr. Stahl. “If we get improvement but I’m worried that long-term we’re still going to have issues with this, I’d probably shy away from using a multifocal lens. Dry eye will decrease contrast, and we don’t want to worsen that with a lens that will do the same.”
• Glaucoma. “We’re shy about using multifocal lenses in patients who have had significant optic nerve damage from glaucoma,” says Dr. Wallace. “If it’s moderate glaucoma—in the 0.5 cup/disc ratio range—we’ll consider it, especially if the patient is motivated. But beyond that, we’re not likely to recommend a multifocal lens. I think a Crystalens would be okay be-cause there’s not as much contrast sensitivity loss.”
• Small or large pupils. Dr. MacRae notes that pupil size is an important consideration. “People with a really large pupil won’t get much benefit from a ReSTOR-type lens,” he points out. “The ReSTOR is apodized, so it tends to perform better as the pupil comes down. Patients who have large pupils even under relatively bright light conditions will probably do better either with a Tecnis multifocal or a Crystalens AO.
“The advantage of the Crystalens HD drops off when the pupil is large because you get a lot of light through the mid-periphery of the lens, rather than just through the central bump,” he continues. “Of course, by switching to the AO you lose the advantage of the 1-D bispheric that the HD has. To compensate, I might give the patient a little more monovision; maybe 0.25 D.
On the other hand, if the individual has a small pupil, a Crystalens HD or ReSTOR +3.0 is more helpful.”
Dr. Stahl points out that patients with smaller pupils will automatically have increased depth of focus, even with a monofocal lens. “So if the patient is concerned about reading, even the Crystalens AO will probably work well,” he says. “Small-aperture optics create a larger range of vision.”
| What Goes in the Second Eye? |
|
Carlos Buznego, MD, in practice at the Center for Excellence in Eye Care in Miami and a volunteer assistant professor of ophthalmology at the Bascom Palmer Eye Institute, believes that the technique of “mixing and matching” presbyopic lenses is no longer a popular approach. “I think that had a lot to do with the prior generation of multifocal IOLs,” he says. “Given the improvements in multifocal and accommodative lenses, I believe most surgeons are sticking with a single type of lens.” Nevertheless, there are circumstances in which surgeons may still be motivated to implant a different type of lens in the second eye.
“Sometimes a patient who receives a multifocal in the first eye has difficulty deciding whether he likes the result enough to want it in the second eye,” says Jason E. Stahl, MD, assistant clinical professor of ophthalmology at the University of Kansas. “Perhaps his near point of focus is not where he anticipated, or he may be struggling a little bit with his intermediate or computer vision. Usually, if I put the same lens in both eyes, patients adapt over time; the range of vision increases and they do just fine. But if a patient needs more time to decide, he gets it, and if he’s still not sure about using multifocal technology in both eyes, we’ll offer the Crystalens as an option. We know the Crystalens is better at intermediate. In my experience, that has always satisfied patients in this situation.” Dr. Stahl adds that leaving at least two weeks between the implants is advantageous. “We learn a lot about how the patient is responding from the first surgery,” he says. “That helps me choose the lens power and decide how I’ll approach the fellow eye.” A different lens might also be appropriate if a patient has had a keratorefractive procedure in one eye but not the other. “We may feel that a multifocal lens is best for the virgin cornea but put a Crystalens in the fellow eye,” notes Dr. Stahl. Dr. Stahl adds that his preferred initial choices for a patient were different in the past. “When the options were the Crystalens 5.0 and the ReSTOR +4.0, putting one in each eye was my primary surgical procedure if I was going with presbyopic lenses,” he says. “It was rare that I’d use a multifocal lens in both eyes. But after the ReSTOR +3.0 was introduced, intermediate vision improved and there was less of a need to do the combination surgery. I still do it on occasion, but it’s not very common in my practice today.” |
“Occasionally we see a patient with a cataract in only one eye, or a patient who only needs to enhance near or distance vision in one eye,” says Dr. Stahl. “In that case we may feel it would be appropriate to operate only on the one eye for the time being.
“There’s been discussion about whether a patient can do well with a multifocal lens in only one eye,” he continues. “I’ve done that in many cases, and I’ve never had an issue with the patient not adapting to it. I’ve also put multifocal lenses in patients who have a monofocal lens in the other eye; they do just fine. It’s better than not having one in either eye.”
Dr. Wallace notes that not implanting a presbyopic lens in this situation means the patient will have to wear reading glasses for the rest of his life. “We’ve been surprisingly successful just treating one eye with a multifocal lens in patients who are motivated to have multifocal vision,” he says. “They’re capable of neuroadapting to the difference in vision between the two eyes—especially if the other eye is close to plano. Sometimes we’ll have to fit them with a contact lens, but generally, they learn to tolerate the difference because they’re so interested in multifocal vision.”
Dr. Wallace admits that such a patient may be less satisfied with a multifocal if the unoperated eye still has some accommodation. “But when they consider the alternative—only having distance vision—they tend to go along with the idea,” he says. He adds that he would consider a Crystalens for such a patient, depending on how important excellent near vision is to the individual.
Dr. Wallace notes that some surgeons in Europe are also experimenting with the idea of putting a multifocal lens in one eye of a plano presbyope—assuming the patient is very motivated to achieve multifocal vision. “The reports indicate that these patients don’t notice much trouble with halos at night, and their near vision and depth perception are quite good,” he says. “This involves less money and less risk than operating on both eyes. And if it doesn’t work out, you can always do surgery on the other eye.”
Dr. Buznego says that he’s had good success implanting a multifocal lens when the other eye has a monofocal lens. “These patients know the wonders of pseudophakia, but most of them wish they could see better up close,” he notes. “I’ve had a pretty high conversion rate in this group of patients, and a high level of satisfaction.”
In some situations, a Crystalens may be a better option. “If a younger patient has no cataract in the fellow eye, especially if he still has some accommodation, the benefit of good near vision gained from a multifocal IOL may be lost on him,” says Dr. Buznego. “Also, the loss in contrast sensitivity is more likely to be symptomatic with a relatively normal fellow eye. I tend to opt for a pseudoaccommodating IOL like the Crystalens with this kind of patient.”
Still Evolving
“I suspect that with all of the improvements in these technologies, we’ll be changing our minds a lot about patient selection, and about what patient expectation levels can be reached, as time goes by,” says Dr. Wallace. “It’s a matter of paying attention to the changes that are taking place, deciding how to react to them, and determining how best to serve our patients.”
Dr. Wallace is a consultant for Bausch+Lomb, AMO, LensAR and Allergan. Dr. Stahl is a consultant for Alcon, AMO, and Bausch+Lomb. Dr. Buznego is a consultant for Alcon, Allergan and Bausch + Lomb. Dr. MacRae is a consultant for Bausch+Lomb.



