Using these refinements, refractive surgeons readily can remove interface matter immediately following LASIK, remove debris and tear-film secretions in the intermediate postoperative period (one to several days), and address striae, flap slippage and epithelial ingrowth in the office at the slit lamp without having to return to the surgical suite.
 |
| In the intermediate postop period (one to several days), surgeons can address striae, flap slippage and other issues without returning to the surgical suite. |
Dr. Lessner developed the techniques over the past three years. "The first thing that I noticed was that people were having these little gaps around the [flap] edge," Dr. Lessner says. "I said, 'I wonder if you can seal this by brushing it with a wet Merocel?' And sure enough, it closes right up." Thus originated what Dr. Lessner calls the Merocel smoothing technique.
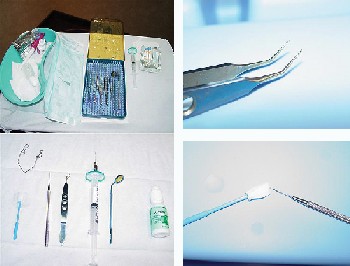
The Merocel is the most important instrument on your tray for these procedures, one that is used in almost all of Dr. Lessner's methods of treating post-LASIK minor complications. After saturating the Merocel with BSS, then pressing out some of the BSS, you can use the Merocel's tip to manipulate loose epithelium along the flap edges. The base of a saturated Merocel—either its side or its face—serves as an excellent smoothing device for striae or to close even the smallest gaps between the flap and bed edges.
Dr. Lessner developed further techniques through a series of discoveries. "I saw some fibers on the edge [in certain patients], and maybe they were under by half a millimeter," Dr. Lessner explains. "I took a little forceps and I pulled it out. There was another one, maybe a little farther in, and I reached a little farther under it, and I found I could pull it out and it didn't disrupt the flap. Then I discovered you could reach all the way into the visual axis, millimeters in, and not in any way disturb the flap. And if you needed to, you just smooth a little bit with the gap-smoothing technique."
The angle of the Kelman-McPherson Forceps is preferable over the non-angled jeweler's forceps for this purpose, Dr. Lessner says. The tool can be used to remove particles and fibers, even those located axially. Another useful tool is the Johnston LASIK applanator, which is an excellent instrument for massaging macrostriae while proptosing the globe using counterpressure with a Barraquer speculum.
Next, Dr. Lessner turned his attention to interface debris and tear-film secretions. "There are two patterns of debris in the interface," Dr. Lessner says. "They're either circumlinear around the edge of the flap, in about half a millimeter all the way around, where the secretions meander up through the nooks and crannies under the edge of the flap on that lumpy, bumpy bed, if you will. Or, if the flap kind of gets stuck to the lid a little bit and it pulls up, you'll see just a layer straight across of debris in a half-circle, crescent shape."
Dr. Lessner found that a 27-ga., air-injection cannula—or any cannula with an angle-to-tip length of 5 mm or greater—can be used to rinse away debris, scattered secretions and heme. This is followed by the Merocel smoothing technique. The cannula is also useful for refloating flaps that are not positioned or draping optimally. One pearl here is to keep only about 1.5 cc of BSS in the 3.0 cc syringe to make the plunger more accessible when used in a one-handed fashion.
|
|