When faced with the problem of deciding between laser iridotomy and cataract surgery for angle-closure patients, a surgeon once quipped, “Do you want to treat the problem or cure it?” Indeed, due to cataract surgery’s excellent efficacy in these patients, some surgeons advocate it as a first-line treatment for angle-closure glaucoma. Other surgeons, however, believe that cataract surgery should be reserved for patients whose intraocular pressure cannot be controlled by laser iridotomy and medications. In this article, experts weigh the pros and cons of both options.
“These two treatments are not interchangeable. It’s easier to do an iridotomy, which takes a couple of minutes, versus a cataract operation, which is kind of a big deal,” says Reay Brown, MD, from Atlanta Ophthalmology Associates. “If a patient has angle-closure
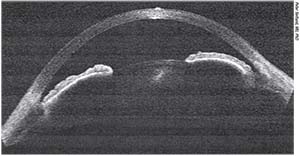 |
| Narrow angle in a nanophthalmic eye. Cataract surgery in narrow-angle patients creates an almost normal open-angle depth. |
glaucoma and elevated pressure, cataract surgery is more effective than an iridotomy for lowering the pressure. However, when you perform a cataract procedure, the patient is exposed to significant risks, such as infection, bleeding and retinal detachment. In contrast, iridotomies have very little risk. So, if a patient has a narrow angle and normal pressures, I wouldn’t even consider cataract surgery. But, if a patient has elevated pressure that can’t be controlled with medical therapy, an iridotomy is unlikely to help them, while cataract surgery might help them a lot.”
Dr. Brown bases his treatment choice on the severity of the patient’s situation. “It’s weighing risk and benefit,” he says. “If a patient has a pressure of 22 mmHg without IOP-lowering medication, and angle closure, I would perform an iridotomy and possibly add a topical medication unless he or she has decreased vision from a cataract. You must match the risk you’re going to expose the patient to with the severity of the glaucoma. Patients who have optic nerve damage and significantly elevated pressures in the high 20s and even 30s on maximal medical therapy should undergo a trabeculectomy or cataract surgery. Cataract surgery is much safer than trabeculectomy, and in many cases can provide long-lasting pressure lowering.”
Dr. Brown explains that the most important difference between cataract surgery and iridotomy is that cataract surgery deepens the anterior chamber and opens the angle to almost a normal open-angle depth, whereas an iridotomy does not deepen the angle or the anterior chamber significantly. “In cataract surgery, you are creating more space, which sort of converts a patient from angle closure to open angle,” he explains. “In other words, the mechanism of angle closure is at least partially counteracted by cataract surgery. An iridotomy will probably prevent an acute attack of angle closure, but there is still the risk of continuing pressure elevation and chronic angle closure. We may be able to completely eliminate these issues with cataract surgery.”
Dr. Brown notes that the data are overwhelmingly in favor of cataract surgery. “However, it’s important to emphasize that this is true in patients with a serious problem. It’s not for patients in whom the angle is just a little narrow,” he says.
Sanjay Asrani, MD, professor of ophthalmology at Duke University, and medical director of the Duke Eye Center of Cary, North Carolina, agrees that treatment depends on whether the patient has acute or chronic narrow-angle glaucoma. “Let’s start with acute narrow-angle glaucoma,” he says. “In these patients, there is no choice but to proceed with the laser iridotomy as a temporary procedure to normalize the IOP levels and then proceed with cataract surgery at a later time. The surgeon is basically just performing a laser iridotomy so that the pressure comes down and the inflammation is controlled quickly, so that elective cataract surgery can be performed in the near future. ‘Near future’ should be emphasized.”
In comparison, patients who have a narrow angle, raised pressure and a normal optic nerve are considered to be pre-glaucoma. “In such cases, if the lens is clear, the treatment would be laser iridotomy and controlling the pressure with eye drops and managing the glaucoma medically,” Dr. Asrani explains. “I do not proceed with cataract surgery in these cases because I may be able to control the pressure medically after a laser iridotomy, and the patient’s lens is clear, so he or she doesn’t require cataract extraction.”
In patients with a narrow angle, optic nerve cupping, and a lens that’s clear or doesn’t have a visually significant cataract, Dr. Asrani will try performing an iridotomy and controlling the pressure with eye drops. “If I find that the target pressure is not achieved with the use of maximum tolerated medical therapy and/or the glaucoma is worsening with the maximum tolerated medical therapy, I will proceed with cataract surgery,” he adds.
Dr. Asrani recommends proceeding with cataract surgery in patients in whom the angle is narrow, the pressure is high, the optic nerve is cupped and the cataract is visually significant, meaning that the patient is already having symptoms of a cataract. “This should help the problem. However, I do not tell patients that cataract surgery is the solution to their problems, only because in many cases the pressure stays high after cataract extraction,” he says. “The reason is that the trabecular meshwork has already been damaged and compromised. Removing the cataract reduces the pressure somewhat, but doesn’t bring the pressure down as far as you would expect. Some doctors advocate removing the cataract when the pressure starts rising and the angle is narrow, to prevent damaging the trabecular meshwork. The concern is that cataract surgery is not without complications. So, you take a person who is 20/20 with high pressure and perform cataract surgery. This is a risk I typically don’t take, unless, once again, I have not been able to control the pressure, the glaucoma is getting worse, or the cataract is visually significant.”
The EAGLE Study
Surgeons agree that cataract surgery should be considered in patients with a visually significant cataract, but the EAGLE (Effectiveness of early lens extraction with intraocular lens implantation for the treatment of primary angle-closure glaucoma) Study found clear-lens extraction is also efficacious and cost-effective.
In the EAGLE Study, between January 2009 and December 2011 researchers enrolled patients from 30 hospitals in five countries.1 Patients were randomized to undergo clear-lens extraction or laser peripheral iridotomy and topical medical treatment. Patients were eligible to participate in the study if they were 50 years of age or older, didn’t have cataracts, and had newly diagnosed primary angle closure with an intraocular pressure of 30 mmHg or greater, or primary angle-closure glaucoma.
The study included 419 participants: 155 had primary angle closure and 263 had primary angle-closure glaucoma. Of these 419 patients, 208 underwent clear-lens extraction and 211 were assigned to standard care. Eighty-four percent of patients (351) had complete data on health status, and 87 percent (366) had complete data on intraocular pressure.
The mean health status score (0.87), assessed with the European Quality of Life-5 Dimensions questionnaire, was 0.052 higher (95% CI 0.015–0.088, p=0.005) and mean intraocular pressure (16.6 mmHg) was 1.18 mmHg lower after clear-lens extraction than after iridotomy and medical treatment.
The incremental cost-effectiveness ratio was $19,721.92 for initial lens extraction versus standard care. One patient who underwent clear-lens extraction and three who received iridotomy and medical treatment experienced irreversible loss of vision. No patients had serious adverse events.
This study found that clear-lens extraction was more effective and more cost-effective than laser peripheral iridotomy and should be considered as an option for first-line treatment.
David Friedman, MD, PhD, Alfred Sommer Professor of Ophthalmology at Johns Hopkins University’s Wilmer Eye Institute and director of Wilmer’s Dana Center for Preventive Ophthalmology, believes that, based on the results of the EAGLE Study, “it’s perfectly reasonable to recommend early cataract extraction for patients who have angle-closure glaucoma or angle closure and elevated IOP. It’s really a shared decision-making process with the patient.”
Dr. Friedman goes on to explain that recommendations and treatment choices depend on defining the population. “For people who have very high eye pressure—which was defined in the EAGLE study as 30 mmHg or higher—and angle closure, or who have angle-closure glaucoma and somewhat elevated pressure, I think the doctor should offer early lens extraction, because those people were shown to have
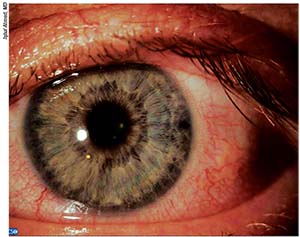 |
| Placing a laser peripheral iridotomy temporally rather than superiorly appears to reduce postop dysphotopsias and cause less pain during surgery. |
better outcomes with early lens extraction,” he says. “They are typically older and are going to need cataract surgery in the next decade in the majority of cases. By operating earlier, the surgeon is just moving the process forward for the patient, removing the need for medications in many cases, and reducing the risk of further surgery to control IOP. The EAGLE Study showed that, if the lens was removed, there were far fewer additional surgeries needed, fewer medications and better control of pressure. Additionally, patients reported slightly better quality of life. I believe that if you look at the road the patient will be going down in the future, he or she will need cataract surgery, so it makes sense to take the lens out early. However, if someone is just an angle-closure suspect and his or her IOP is normal, I would never take the lens out. I would always consider iridotomy. Lens extraction is not indicated in those cases.”
Insurance Reimbursement
Dr. Asrani notes that he is “a pro-iridotomy guy.” He says that, in the EAGLE Study, the investigators included patients with high pressures and no glaucoma damage. “This means that the pressures had not been high for very long,” he explains. “In these patients, when you remove the cataract, the pressure will come down because the trabecular meshwork has not been damaged for a long time.
“The issue is that the investigators took out cataracts when they were not visually significant,” he adds. Here, in our insurance scenario, it is not easy to get approval for clear-lens extraction just for the sake of lowering pressure, especially if you haven’t tried maximal medical therapy and/or laser iridotomy, or proven that the glaucoma is getting worse despite all your efforts. Then, the insurance carriers might cover cataract surgery for glaucoma, but, otherwise, it’s not an easy task to get approval for clear-lens extraction for narrow angles.”
Dr. Asrani encourages surgeons to strongly consider performing simultaneous glaucoma surgery and cataract surgery if the patient has significant cupping or if glaucoma has damaged the optic nerve. “This is especially true if there is cupping that involves the superior neuroretinal rim,” he says.
According to Dr. Asrani, cataract surgery should be reserved for those whose pressure isn’t controlled with maximum tolerated medical therapy, or for those whose glaucoma is getting worse. “If their glaucoma is getting worse or their pressure is not coming under control under their maximum tolerated medical therapy, then, even if the cataract is not visually significant, I will go ahead and get insurance approval and proceed with cataract surgery,” he says.
Dr. Friedman agrees that there are some issues with reimbursement. “The volumes have been relatively small, so I’m not sure how exactly to code for these things,” he avers. “I think this is going to have to come up in coding discussions, but I’m not sure where that process is on the national level.”
In younger patients, Dr. Friedman still recommends offering cataract surgery as an option. “In the EAGLE Study, the minimum age was 50 to avoid inducing presbyopia,” he recalls. “This study also excluded certain people, such as those with extremely shallow anterior chambers, because these people are at increased risk of complications during cataract surgery. Cataract surgery should be used to treat angle-closure glaucoma in patients in whom lens extraction is likely to be very straightforward with very few complications. And in the EAGLE Study, there was a 1-percent posterior capsule rupture rate, despite the fact that lens extraction was performed by many surgeons over a very large number of hospitals. That’s the basis on which I’m making my decision. The patient is part of the discussion and should be offered cataract surgery.” REVIEW
1. Azuara-Blanco A, Burr J, Ramsay C, et al, for the EAGLE study group. Effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma: A randomized controlled trial. Lancet 2016;388:1389-1397.
Suggested Reading
1. Brown RH, Zhong L, Lynch, MG. Lens-based glaucoma surgery: Using cataract surgery to reduce intraocular pressure. J Cataract Refract Surg 2014;40:1255-1262.



