Today, all ophthalmologists are familiar with OCT (optical coherence tomography) technology, commonly used to image the retina to aid in the diagnosis of retinal disease and glaucoma. Unfortunately, the popular OCT instrument has limited usefulness for some purposes. It scans with short-wavelength illumination, preventing it from penetrating easily through the optically opaque sclera, which makes it very difficult to image the angle at the root of the iris. Imaging the angle is crucial for monitoring the risk of angle-closure glaucoma—a worldwide health issue. Huge populations, particularly in
Anterior segment OCT is a new iteration of OCT technology that avoids this limitation. AS-OCT uses a longer wavelength of light that penetrates the sclera, while also allowing the safe use of higher levels of power. As a result, it can produce high-resolution images of the angle comparable to those obtained with ultrasound biomicroscopy.
At the moment, AS-OCT technology's primary applications are in refractive surgery—for example, looking at the cornea, examining incisions from LASIK and measuring anterior chamber biometry for placement of phakic IOLs. However, once the instrument becomes more widely available, it could also become a commonly used tool in angle-closure glaucoma diagnosis. The high-resolution images that can be captured, and the ease with which they can be captured, have the potential to change the way we look at patients when we suspect the angle may be at risk.
OCT vs. Gonioscopy
When considering the value of a new technology, it's important to compare its advantages to those of existing technologies already in use for the same purpose. Two methods that currently can be used to monitor the angle are gonioscopy and UBM.
The traditional method for determining whether someone has angle closure, or is at risk for getting it, is to perform gonioscopy. However, gonioscopy has several significant disadvantages: It's subjective, making it prone to inter-observer variability in the interpretation of the results; it's time-consuming; it requires a very skilled observer; and the illumination required to view the anterior segment can cause the pupil to constrict, making the angle appear less closed than it actually is under other conditions.
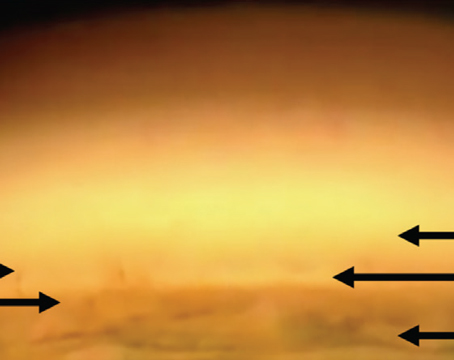
In contrast, OCT scanning is objective, takes less time and doesn't require a highly skilled technician to accomplish. Perhaps most significant for use in diagnosing glaucoma, AS-OCT can image the anterior segment anatomy in a dark room with an infrared light source that doesn't induce any pupillary constriction. This lets us get undisturbed images in the dark, which is the circumstance in which the angle is the narrowest. (Even using UBM requires a certain amount of room illumination in order to see what you're doing.)
OCT vs. UBM
UBM also has the capacity to produce high-quality images of anterior segment structures such as the angle, and it's been available for many years. In fact, UBM technology does have a few advantages over AS-OCT as a glaucoma tool, but OCT's advantages are more significant.
The main selling point for using UBM to monitor glaucoma is that it can readily image behind the iris. That means it can visualize the ciliary body, which can be useful if a patient has aqueous misdirection (sometimes referred to as malignant glaucoma) or plateau iris syndrome, in which the ciliary body is placed more anteriorly. When using OCT for this purpose you get a high degree of reflectance from the iris and shadowing behind the iris. This is a relatively minor advantage for UBM, however, because only a limited number of patients have these conditions.
Unquestionably, the greatest advantage OCT has in this situation is that it's a non-contact technique. While UBM requires using a gel or water bath to couple with the eye, to scan with OCT the patient just puts his chin in the slit lamp chinrest. To be imaged with UBM, a patient has to lie on his back; the cornea has to be anesthetized so the eye cup can be placed against the eye and filled with water or another solution. This process can be messy and uncomfortable for the patient, and it can take a long time. In addition, the operator has to be very skilled in order to get high-quality images. Moreover, the probe tip oscillates, which can be disconcerting for the patient.
In terms of accuracy, we've done some studies looking at the repeatability of measurements for both instruments; we've found that UBM and AS-OCT are comparable in terms of their inter-test repeatability. They seem to provide equally precise measurements. 
As you might expect, in a head-to-head comparison their numbers don't match exactly; there are systematic differences in measurement technique (such as the way light reflection data or sound echoes are converted into images) that lead to slightly different values. However, I don't believe these differences are clinically important. (At the same time, it's worth noting that UBM may actually alter the internal dimensions of the eye slightly because it does require the patient to lie on his back, and the eye cup pressing against the eye could also influence the results.)
In general it's unlikely that one measurement is more correct than the other, but the practical advantages of a non-contact technique give AS-OCT an edge as a clinical tool.
Identifying Patients at Risk
To be most useful as a diagnostic tool for glaucoma, it's important to find ways to use data to identify patients who may be in trouble or at risk. Two effective ways to accomplish this are 1) to accumulate normative data, making it possible to identify patients who fall outside the normal range; and 2) to follow patients over time and see which ones end up developing the problem. The latter approach makes it possible to identify baseline parameters indicative of greater risk.
Unfortunately, we don't yet have normative data from any population-based source for either AS-OCT or UBM, the two most objective sources of data on angle closure. AS-OCT is still too new to have such data, and although UBM has been available for many years, the cumbersome nature of the test discourages clinicians from trying to image a large number of people just to build a normative database. Also, because of the expense, limited applications and difficulty of use, UBM is often only available through multi-specialty practices and academic centers.
The second approach—following populations over time to determine baseline characteristics that accompany later disease progression—would allow us to provide prophylactic treatment in the form of a laser iridotomy for patients at high risk. Currently we are using this approach when we perform gonioscopy, but the judgment is subjective, and the method itself predisposes the angle to appear more open than it may be the rest of the time, for reasons described earlier. Given these factors, it's very likely that angle closure, as determined by gonioscopy, is being underdiagnosed.
In contrast, AS-OCT has the potential to provide this information in a much easier and more objective way, which could be tremendously beneficial. At this point, it seems like only a question of time before AS-OCT will accumulate both kinds of database, which could make it a powerful screening tool.
Is It Time to Switch?
Aside from looking for angle closure, AS-OCT technology could also potentially be useful for monitoring eyes with pigmentary glaucoma, in which there is posterior bowing of the iris; it could be used to quantify the change in anterior segment anatomy after a laser iridotomy; and it could help to identify patients with nonpupillary block angle closure, or plateau iris. Although the ciliary processes are placed anteriorly in plateau iris, and the ciliary body can only be imaged reliably by UBM, the iris contour is also unique in patients with this condition and performance of a laser iridotomy doesn't alter this anatomy. In contrast, the iris contour changes and the depth increases in patients with the more common pupillary block form of primary angle closure. Thus, determining whether or not the iris contour changes following laser iridotomy may prove to be useful in identifying those with plateau iris, even though OCT can't image posterior to the iris.
In addition, we're currently investigating using AS-OCT to image filtering blebs after trabeculectomy; we've been able to identify anatomic features within blebs that may indicate a risk of failure or a likelihood of success. This information could eventually help us to determine who would benefit from suture lysis or bleb revision, but our work in this area is still in the early stages.
Currently, two instruments designed for anterior segment OCT scanning are available in the
In the meantime, AS-OCT is useful even without the normative or long-term data. In our clinic we've found that a small percentage of patients who don't look narrow at the slit lamp reveal the iris in contact with the trabecular meshwork when scanned with AS-OCT in a darkened room. Compared to gonioscopy, AS-OCT is leading us to classify more patients as having a narrow or closed angle.
Over time, as the use of AS-OCT becomes more widespread and we learn how to use the data it generates, it should become an important tool in the day-to-day clinical management of glaucoma.
Dr. Smith is an assistant professor of ophthalmology at the Cleveland Clinic Lerner College of Medicine of