AS LONG AS LASIK REMAINS POPULAR, SURGEONS will be searching for the best way to create the flap. Today, some surgeons believe that femtosecond lasers will eventually replace mechanical microkeratomes as the gold standard for flap-making.
With that in mind, we asked a number of top surgeons to share their thoughts about the future of laser flaps and microkeratomes. They spoke about the current merits and disadvantages of both methods, and how future changes in the instruments themselves and the nature of refractive surgery may affect their popularity.
We found that many surgeons who have purchased a femtosecond laser have become enthusiastic proponents of the technology—but others are a long way from being sold on it.
One advantage that most surgeons are willing to concede to the laser is reproducibility. Terrence P. O'Brien, MD, director of the Ocular Microbiology Laboratory at Johns Hopkins Wilmer Eye Institute, says that he and his colleagues are gradually developing a preference for the use of the laser because of its accuracy. "The laser allows us to set the flap depth more precisely than automated keratomes," he notes. "You can create the shape and diameter that you want and avoid some of the blade complications that can occur with automated microkeratomes."
"Laser flaps have a tighter standard deviation," agrees Eric Donnenfeld, MD, co-chairman of cornea and external disease at Manhattan Eye Ear and Throat Hospital and associate professor of ophthalmology at New York University Medical Center. "However," he adds, "people often quote early studies that compared the IntraLase to the older keratomes. Newer keratomes, like the Amadeus II and the Zyoptix XT, have much tighter standard deviations."
Perry Binder, MD, co-medical director for IntraLase, Inc., says, "Microkeratome flap thickness is influenced by preop corneal thickness, and corneal steepness affects hinge dimensions, flap thickness and flap diameter. In addition, you have to change microkeratome blades between eyes to get the same flap thicknesses when doing both eyes of one patient.
|
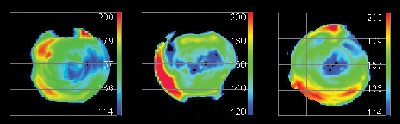
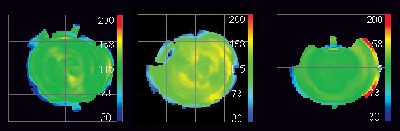
Flap Thickness: Mechanical versus Laser |
|
|
|
|
| Thickness of LASIK flaps, scanned by the Artemis 2 (Ultralink LLC). Flaps were created using a Hansatome 160-Z head (top); Intralase set at 110 µm (bottom). |
The femtosecond laser is widely perceived as being safer than a mechanical microkeratome, particularly in terms of intraoperative complications. However, not everyone believes the difference is significant. "With a microkeratome you can get more devastating complications like buttonholes or incomplete flaps," notes Dr. Donnenfeld, "but if you let the flap heal and do photorefractive keratectomy the patient almost always ends up with 20/20 vision.
"On the other hand," he says, "the literature suggests that complications seen with IntraLase are more subtle, but more common—more diffuse lamellar keratitis, epithelial ingrowth and transient light sensitivity. Your severe complication rate is probably lower with the laser, but your overall complication rate is higher."
Vance Thompson, MD, who practices at Vance Thompson Vision, Sioux Valley Clinic in Sioux Falls, S.D., and is assistant professor of ophthalmology at the University of South Dakota School of Medicine, notes that laser complications decrease with experience. "When you first get your laser, if the settings are too high, you can see more inflammation at the edge," he says. "However, I don't think I've seen more inflammation with laser flaps than with blade flaps. What I have seen more of is transient light sensitivity at one to two months postop. I don't know the cause, but with a week of q.i.d. steroids, the vast majority of eyes are back to normal.
Dr. Thompson says the best thing about the complications associated with laser flaps is that they're not vision-threatening, unlike a button-hole or partial flap caused by a blade, which can lead to loss of best-corrected vision. He adds that one of the things he's enjoyed about laser flaps is a decrease in the incidence of dry eye. "I think it's because the laser flap is not meniscus-shaped, so it cuts through fewer corneal nerves in the peripheral cornea compared to a blade flap that's thinner centrally but can be quite thick at the edge."
Y. Ralph Chu, MD, medical director of Chu Vision Institute in Edina, Minn., and adjunct assistant professor of ophthalmology at the University of Minnesota, says he thinks it's really a question of choosing which set of complications you prefer to deal with. "Mechanical microkeratomes have advanced to a level where it's difficult to say that you get more safety with the laser. Dr. Robert Maloney just did a study looking at 16,756 of his own microkeratome cases; he had one complication per 1,676 eyes. So for him to reduce complications by switching to the IntraLase sets a pretty high bar."
| Deja Vu All Over Again |
| Several surgeons recalled other technologies overtaking pre-existing ones. Y. Ralph Chu, MD, says he's reminded of the debate over the IOLMaster and immersion A-scan. "When a new technology costs so much more, you want to make sure it adds enough value," he says. "An IOLMaster costs a lot more than an immersion A-scan machine, and there are still times when you need to use your A-scan, which has proven to be just as accurate. For many practices, adding this laser technology probably won't be cost effective." Perry Binder, MD, MS, say he "totally understands" the laser skeptics' point of view. "But consider this," he says. "When $500,000 excimer lasers came out, they replaced radial keratotomy, which uses about $3,000 worth of equipment. Why did that happen? Because the lasers produced better outcomes, had greater patient acceptance, and were more predictable." "This situation is being a lot like extracap versus phacoemulsification," notes Vance Thompson, MD. "People didn't think phaco would replace extracap, but it did. However, sometimes we still need to do an extracap. So even if laser flaps do become the gold standard, we'll still need to know how to make a blade flap. That's one reason I try to stay good at both." |
Dr. Binder notes that the peripheral DLK that is sometimes seen with the laser decreases as experience increases and energy settings are refined. He also notes that less than 1 percent of patients complain of light sensitivity six or eight weeks after surgery, and it doesn't affect their visual acuity. "If I had to trade off buttonholes, decentered, flaps, or flaps that are too thin or thick," he concludes, "I'd much rather have these problems than those."
Comparing Outcomes
At the April 2005 ASCRS meeting in Washington, D.C., Steve Schallhorn, MD and Dan Durrie, MD, presented data from recent studies suggesting that laser flaps produce better UCVA and contrast sensitivity—especially at the outset. (Dr. Schallhorn's study was prospective and masked; Dr. Durrie's study was randomized, prospective, masked and contralateral.) Dr. Schallhorn notes that contrast sensitivity was better under both photopic and mesopic conditions; Dr. Durrie found that the IntraLase's results were better in terms of visual acuity, Schirmer's test, tear film, corneal staining and contrast sensitivity at all time points.
| Uncorrected Visual Acuity (Cumulative ETDRS)—12-Month Cohort |
|
Postop 1 Day *p=0.09 Postop 3 months *p=0.0001 Postop 6 months *p=0.02 Postop 12 months *p<0.5 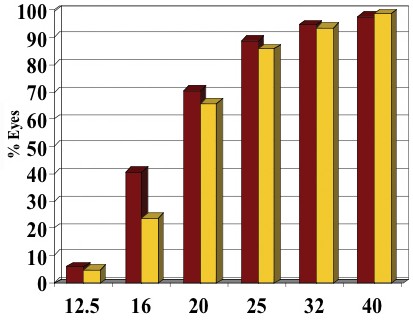 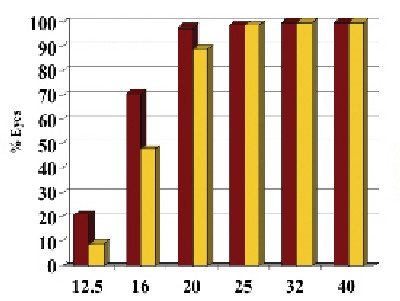 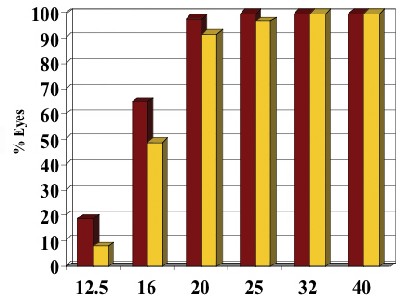 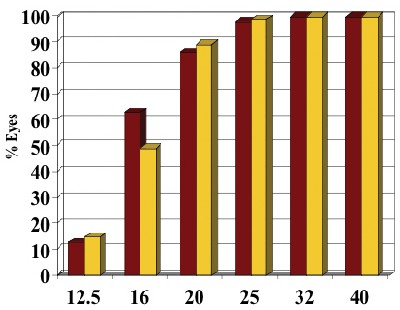 Dan Durrie, MD |
| In this prospective, randomized, contralateral study, visual results with an IntraLase flap were initially superior; however Hansatome flap patients caught up by 12-month follow-up. (Note the shifting p-values.) This was also true for contrast sensitivity. |
Nevertheless, skeptics have pointed to earlier data, such as a study reported in 2004 by J. Trevor Woodhams, MD, FAAO, a LASIK pioneer and clinical associate professor of ophthalmology at Emory University in Atlanta, that found better postop acuity with microkeratome flaps. However, Dr. Woodhams has since had much better results with the laser. "During the first year that I used the IntraLase," he says, "we experienced an unacceptable amount of postoperative photophobia and DLK despite using the lowest possible energy settings. However, subsequent work with the company, including using a newer model with faster application time, has almost completely eliminated this problem. We currently use the IntraLase in a majority of our LASIK cases, with excellent results."
Practical Concerns
One set of factors that will affect the ultimate popularity of laser flaps is the day-to-day use of the laser in a clinical setting. These issues include:
• Cost. "Using the laser costs me around $230 extra per case," says Dr. Thompson. "However, more than 90 percent of my patients, who come from all income levels, choose to have surgery despite the extra cost."
Dr. Chu isn't convinced. "I've heard of surgeons who raised their price only to drop it again. And some practices will find it difficult to pass along that cost. I'm already at $2,200 per eye, and talking a patient into a $2,700 eye surgery is a different ballgame," he says.
Dr. Binder says that he was nervous when he and his partner decided to invest in the laser technology. "However," he says, "our profitability has gone up, our complication rates have gone down and our patient satisfaction is up."
• Speed of the procedure. Dr. Binder admits that the longer time required to make the flap using the laser is a valid concern. "With the current 15-kHz IntraLase it takes me 57 seconds to create a 9-mm diameter flap, and the patient comes in and out of the room to have bilateral laser flaps created. That takes about four or five minutes, plus I wait about 10 minutes for the gas bubbles to disappear. Instead of doing four patients an hour, I can do two or three an hour," he says.
Dr. Thompson says working with the forthcoming upgrade to the IntraLase (with a pulse repetition rate of 15 kHz instead of 30 kHz) has improved things. "The current laser takes about a minute per eye. But with the 30-kHz we're getting down to the 40-second range, and we feel like it goes faster than when we use a blade. However," he adds, "if you have to make the laser flap in a different room than the room where you do the correction, that will slow you down and affect your flow a bit."
• Portability. A mechanical microkeratome is far easier to transport from one office to another than a laser. However, Dr. Binder notes that lifting a laser flap for the first time several months after it was actually created is just as easy as lifting any enhancement flap. "Patients can have the flap created at a central office and have the rest of the LASIK procedure done later at another office," he says.
• Marketing. When the femtosecond laser first attracted interest, many surgeons used it as a marketing tool. Today, many surgeons are skeptical of its value in this arena.
"I'm one of the medical monitors for TLC The Laser Center," notes Dr. Donnenfeld. "TLC looked at procedural volume at 73 of our centers; the 68 centers that only offer microkeratome flaps showed more growth than the five centers where the company offers laser flaps. That suggests that offering the IntraLase is not a guarantee that you'll attract more patients. In fact, I do hundreds of LASIK procedures every month, and only one or two patients a year ask for a laser flap."
Dr. Donnenfeld also notes that marketing advantages tend to wear off rapidly. "In my experience, marketing only has a two-year lifespan," he says.
Dr. Chu agrees. "As soon as another technology comes along, you've lost your edge," he says. "I believe patients choose based on their relationship with the surgeon, perhaps on price, but very rarely on technology alone."
Future Factors
Several issues relating to the changing nature of refractive surgery could have a big impact on whether laser flaps become the gold standard. One of the those is whether LASIK holds on to its current dominance of the refractive surgery market.
"Our practice is one of the clinical investigators for epi-LASIK, using the Amadeus microkeratome," says Dr. Chu. "It's much better than PRK. The patients heal much faster. I love it, and I think it will be 25 to 30 percent of my practice within six months to a year."
Dr. Donnenfeld agrees. "It wouldn't surprise me if I end up doing 20 to 25 percent of my cases with surface ablation very soon," he says. "The IntraLase won't be helped by this. But a keratome that can do epi-LASIK will allow you to do both procedures."
On the other hand, a shift that may work in the favor of the lasers' popularity is new surgeon preference. "If you offer a microkeratome and a laser flap maker to a new surgeon, they're going to put the blade in the closet," says Dr. Thompson. "I've already had people refer patients to me because they needed a blade flap, and the surgeon wasn't experienced with blade flaps!"
Dr. Chu isn't convinced that this will reduce microkeratome usage. "If I was starting out now," he notes, "using the laser to make flaps might be attractive, but I probably couldn't afford to buy an IntraLase."
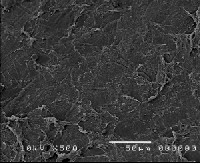
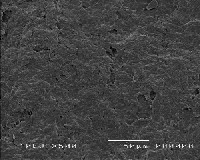
| Which Bed Is Smoother? | ||||||
|
When comparing flaps made by mechanical microkeratomes to flaps made by the femtosecond laser, one concern that has engendered serious debate is the smoothness of the resulting bed.
However, a masked study conducted by Daniel B. Tran, MD, and Perry Binder, MD, MS, compared SEMs of the beds created by a Hansatome and the IntraLase at a depth of about 110 µm, with different results: Three doctors found no difference between them. Software used to judge surface roughness quantitatively also found no difference. (See examples, above.) However, the laser bed was rated superior if the Hansatome blade was making its second cut.
Drs. Tran and Binder also compared the corneal beds left by deeper cuts (between 180 and 190 µm) and found all beds to be rougher, with the IntraLase bed more so than the Hansatome. However, they believe this is clinically irrelevant, since few surgeons would choose to cut this deep. Vance Thompson, MD, notes that the new 30-kHz laser produces smoother beds than the 15-kHz model, and is less dependent on surgeon technique. |
The Impact of Evolution
Another major factor in the future popularity of laser flaps will be improvements in technology. Next-generation mechanical microkeratomes, such as the new Zyoptix XP keratome from Bausch & Lomb, are offering tighter standard deviations in flap thickness and more options for hinge position, as well as greater ease of use. At the same time, the next generation IntraLase, which the company hopes to have on the market this summer, features a 30 kHz laser (compared to a 15 kHz laser in the current model).
Dan B. Tran, MD, who practices at Coastal Vision Laser Eye Centers in Newport Beach, Calif., has been working with the new version for several months. "Doubling the kilohertz has cut treatment time in half," he notes. "It also allows us to decrease the energy per laser spot and the separation between laser spots for better quality dissection and a flap that lifts more easily. This should mean less chance for postop inflammation and faster visual recovery."
Trudy Larkins, global director of professional relations at IntraLase, says that the company is optimizing the laser system for other uses, including anterior lamellar keratoplasty, deep lamellar keratoplasty, penetrating keratoplasty, and posterior keratoplasty. "In terms of ophthalmic applications," she says, "the IntraLase is still in its infancy."
So: Are Laser Flaps Inevitable?
Overall, our surgeons generally see a bright future for the femtosecond laser—with some qualifications. "I think laser flaps are inevitable," says Dr. Donnenfeld. "As technology improves, the laser will eventually do a better job of making a flap than a keratome will. However, for one technology to replace another, you need to show a very significant superiority, and I don't think we see that today."
Dr. Thompson gives a qualified yes. "For virgin, uncut corneas, the laser flap is the best way to go," he says. "With studies showing better visual results and fewer enhancements, I think we're moving towards an era of all laser flaps."
Dr. O'Brien is a little more cautious. "Eventually the biological and scientific advantages may overcome the economic disincentive," he says. "On the other hand, we don't fully know what effect the laser energy is having on corneal tissue. Nevertheless, I think lasers will gradually gain prominence because of their safety profile and their ability to more precisely control the dimensions of the flap."
Dr. Binder sees the eventual dominance of laser flaps as inevitable. "Mechanical microkeratomes work well," he says. "But if you look at all the parameters, the femtosecond laser far outdoes a mechanical microkeratome.
"If you're curious about laser flaps," he adds, "watch a procedure, look at the patients. You'll be convinced."
Suggested Reading
Binder, P. Flap dimensions created with the IntraLase FS laser. J Cataract Refract Surg 2004;30:26–32
Kezirian GM, Stonecipher KG. Comparison of the IntraLase femtosecond laser and mechanical keratomes for laser in situ keratomileusis. J Cataract Refract Surg 2004; 30:804–811.
Tran DB, Sarayba MA, Bor Z, Garufis C, Duh YJ, Soltes CR, Juhasz T, Kurtz RM. Femtosecond laser versus mechanical keratome flaps in wavefront-guided laser in situ keratomileusis. J Cataract Refract Surg 2005;31:97-105.
Durrie DS, Kezirian GM. Femtosecond laser versus mechanical keratome flaps in wavefront-guided laser in situ keratomileusis. J Cataract Refract Surg 2005;31:120-126.