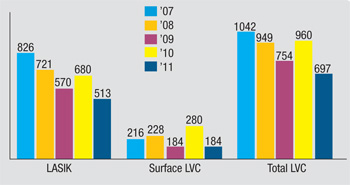
On last year’s survey of members of the American Society of Cataract and Refractive Surgery, signs of hope seemed to be emerging, as laser vision correction volumes showed their first increase since 2008. However, as the survey’s co-administrator Richard Duffey, MD, cautions, it takes a couple of years’ worth of data before you can call something a trend. Sure enough, volumes dropped again on this year’s survey, indicating that surgeons still may not be out of the woods.
This article reviews significant results from this year’s ASCRS survey, such as volumes and the procedures surgeons prefer for certain patients, with an eye toward emerging trends.
Surgical Volumes
Total LVC volume decreased from an anomalous 960,000 procedures in 2010 to 697,000 for this survey year, 2011. However, this is around the total of 754,000 from 2009. When compared to LVC’s heyday seven years ago, this year’s total is a decrease of 35 percent. PRK, as a percentage of this total, has steadily risen over the years, from 12 percent in 2005 to 26 percent in 2011.
“The bump in total LVC procedures on the 2010 survey is difficult to explain,” says Dr. Duffey. “When you look at the other survey we do—with the ISRS—LVC volumes were down a little bit last year and again this year, so there was no increase in last year’s ISRS survey. I talked with my survey partner, David Leaming, MD, and we crunched the numbers several times again, and they do indeed show that ASCRS members reported a growth last year. It might just be an anomaly, because occasionally some of the data can get questionable depending on the response rate. So with data, if you see something go up one year, check the next year. More important, though, is taking a look over the past five years and seeing that it’s down 35 percent. That’s probably a better indication of where things stand.
However, I have every reason to believe we’re all up a little bit as time has progressed this year. Both people and corporations that I speak to are all seeing a bit of a bump. Even though one quarter of statistics doesn’t tell all, this a nice positive indicator that we haven’t seen in a while.”
|
Preferred Procedures
Though many surgeons have moved away from LVC for high myopes, on the survey 36 percent of respondents say they’ll still use it for a -10 D patient. “I’m one of those,” avers Dr. Duffey. “I avoid phakic IOLs as much as I can because they involve intraocular procedures. I’d much prefer to stay extraocular, and I’ll still get excellent results if all other parameters are equal. I’ll even go up to -12 D with LVC.” He notes that the percentage of ASCRS surgeons who would prefer phakic IOLs for this type of patient presentation has steadily gone up over the years, and now sits at 46 percent on the survey.
Dr. Duffey says concerns over LVC in high myopes aren’t very significant as long as the patient is properly screened. “If all parameters are normal and the patient has a thick cornea and will have enough residual stromal bed postop, then I don’t think it would make that big of a difference,” he says. “How abnormal these corneas are also matters. We certainly have a subset of people who are high myopes and whose corneas are very normal, they just have an axial length issue, not a corneal curvature issue that’s resulted in their myopia. I think that’s more the norm. If a patient is a high myope because he has a 50-D cornea, however, then you’ve got a problem on your hands and we won’t be doing LVC on that patient.”
For the low hyperope (+3 D), LASIK is still the procedure preferred by ASCRS surgeons, at 57 percent. Twenty-two percent would do refractive lens exchange, 10 percent prefer PRK and 11 percent would just wait. For the high hyperope (+5 D), the numbers flip, and 57 percent prefer RLE, 33 percent like to wait, 7 percent would do LVC and 2 percent prefer a phakic lens. “There’s no doubt that 5 D of hyperopia is still too much for all of us,” says Dr. Duffey. “Just single-digit percentages of surgeons are willing to do LVC on this patient.”
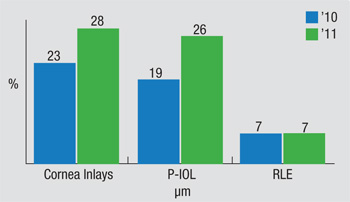
One interesting development Dr. Duffey notes is the continuing confidence some surgeons have in simultaneous bilateral intraocular surgery for phakic lens implantation. Last year 19 percent said they’d do it, now just over a quarter of surgeons say they would. “It’s interesting that 26 percent of doctors say they’ll perform simultaneous, bilateral surgery for these patients,” Dr. Duffey says. Though Dr. Duffey says he’s seen studies that say the odds of having a problem with these surgeries aren’t high, he thinks that if a problem ever occurs with them their acceptance will drop.
The survey also asks about surgeons and their family members who have had refractive surgery. “It’s interesting, if you add the numbers together, 25 percent of surgeons have had it, 28 percent say their spouses have had refractive surgery and 54 percent have at least one sibling who’s had it done. Also, 23 percent have a child who’s undergone refractive surgery,” says Dr. Duffey.
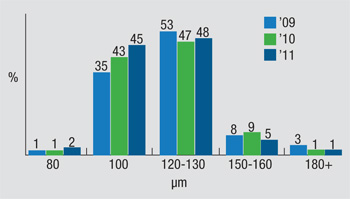
Flap Making
The trends in flap thickness appear to be shifting toward a preferred thickness of 100 µm, an option chosen by 45 percent of the survey’s respondents. “We’re moving toward 100 µm, but it’s not quite there yet, with 48 percent preferring flaps between 120 and 130 µm,” notes Dr. Duffey. “When you look at the growth of 100 µm, it’s grown pretty much every year. Even those who use microkeratomes now have better microkeratomes that make very nice thin flaps that are relatively planar in shape, as well.” Dr. Duffey doesn’t see the preferred thickness going much below 100 µm, though. “Sixty-five microns is the epithelium,” he says. “So the surgeon doesn’t want to end up with no stroma. But if your flap-making device is set for 80 µm, you don’t have a lot of leeway in there if the cut turns out to be off a little bit, so I think 100 is where the comfort zone is.
“In terms of residual stromal bed, we’re pushing toward 275 to 300 µm, amounts that, when put together, are preferred by 55 percent of the surgeons,” Dr. Duffey continues. “This is opposed to 40 percent who prefer a 250-µm thick bed, the old number we used to use for residual bed thickness.” REVIEW