WITH ALL THE ATTENTION PAID TO LASIK, it's possible to overlook the issues that might crop up with surface procedures such as PRK and epi-LASIK. In my practice, however, I do all my refractive procedures with surface ablation, so I'm well-acquainted with what can go awry. In this article, I'll provide a refresher on preventing and managing complications related to surface ablation.
Here are potential problems to watch for:
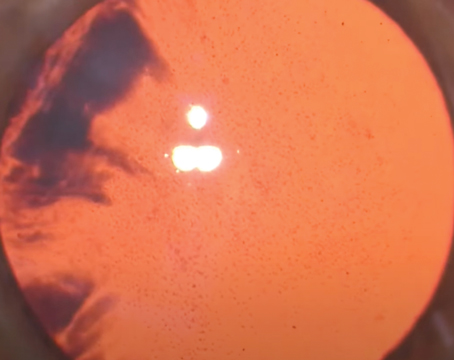
• Haze and regression. The risk of haze is related to ablation depth. So, to help head off any possible haze problems, I try to identify patients preop who may be at increased risk for haze, specifically those who are more nearsighted who will therefore need a deeper ablation.
In comparing custom treatment to standard on the Visx laser, there is typically not much of a difference in ablation depth for the same level of myopia, so selection of custom versus standard should typically not influence the risk of haze. If you use another platform, though, double-check the amount of tissue it removes for higher ablations.
The other risk factor I look for in patients is frequent exposure to high levels of ultraviolet radiation (e.g., boaters, outdoor athletes, etc.). These patients may have a higher risk of haze as as a result of the constant UV exposure.
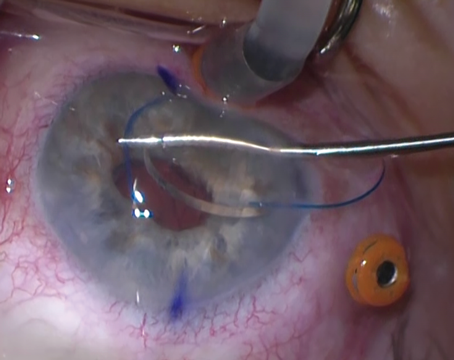
 |
| An incomplete flap is an unfortunate possibility with epi-LASIK. |
As a possible reason to perform LASEK or epi-LASIK, there is some evidence to suggest that the presence of an epithelial flap reduces the risk of haze.1,2,3 In light of these reports, I'm more likely to try to preserve an epithelial flap in a high myope vs. someone who's -2 D, in whom there's not as much of a risk for haze.
Also, one study suggested that oral vitamin C may be helpful in avoiding haze.4 I currently recommend at-risk patients take 1,000 mg per day, starting a week before their surgery. They then continue vitamin C several weeks postop.
As a final hedge against haze, surgeons have the option of using mitomycin C. When I use it, I use the regimen advocated by Chicago surgeons Randy Epstein and Parag Majmudar: 0.02% for 12 seconds following the ablation.
If a patient develops haze postop, I start Pred Forte every four to six hours, and question the patient to see if there is an underlying cause, such as sun exposure that can be remedied by the use of sunglasses. If you identify haze early, it will typically respond nicely to topical steroids. After four to eight weeks, the haze will decrease, along with a reduction in the myopic shift (regression) that often occurs concomitantly. The latter will often be the first sign that the haze is responding to treatment.
One of the risks with steroid use is elevation in intraocular pressure. If the pressure spikes, topical glaucoma medications are required, since you still need to continue the topical steroids to treat the haze. If the pressure remains high, you can switch to a steroid with a lower potency, such as Lotemax (Bausch & Lomb) or FML (Allergan), which would help reduce the IOP.
• Dry eye. One of the common reasons patients have refractive surgery is contact lens difficulties, and one of the common causes of these difficulties is dry eye. If dry eye isn't recognized prior to surface ablation, patients can have a delay in their epithelial healing. Patients identified with dry eyes preoperatively can be helped with treatments such as Restasis. Studies have shown that Restasis helps improve the visual results after LASIK. In one study, researchers showed that patients treated with Restasis were more likely than untreated ones to have a 20/20 result after LASIK. (Ursea R, et al. Invest Ophthalmol Vis Sci 2005;46:ARVO E-Abstract 4381)
Surface ablation patients with preop dry eye can also benefit from Restasis.
I start Restasis anywhere from a week to four weeks preop, usually as soon as I diagnose the patient with mild to moderate dry eye at the initial refractive-surgery screening visit. I have patients use it twice a day. I also use punctal plugs, which I'll place the day of surgery or soon thereafter in patients for whom Restasis wasn't enough. I prefer to start Restasis first, and after the inflammation has been reduced, raise the tear film with the plugs. The Parasol external plug and the Oasis internal plug have worked well for me.
To diagnose dry eye, I prefer to use Schirmer's tests with anesthesia, and will start Restasis if the test result is 5 mm or less. I'm also more likely to start Restasis if patients have significant symptoms, such as intolerance to contact lenses or blurred vision when using the computer.
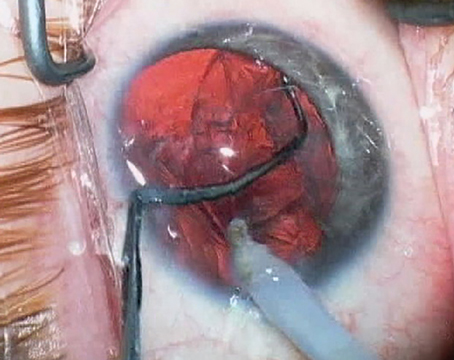
 |
| Using a blade, you can finish creating an epithelial flap in epi-LASIK. |
Anecdotally, I've also seen evidence of the benefits of this approach in consultation with physicians with surface-ablation patients who weren't pretreated ahead of time for their dry-eye symptoms. These patients had delayed epithelial healing and more discomfort after surgery than typical surface-ablation patients. When I examined them, I discovered that they had a history of dry-eye symptoms, leading me to believe that if they had been pretreated for their dry eye, either with Restasis or plugs, they may have had an easier postoperative course.
• Delayed epithelial healing. This increases the risk for haze and causes more discomfort postop.
To promote swift healing, I make sure I treat for any dry eye, and use a bandage contact lens that has a high oxygen-permeability factor.
If there's a delay in healing, I'll reduce the total amount of medicated drops to avoid preservative toxicity.
• Over- and undercorrections. When patients end up over- or under-corrected, I attempt to identify any epithelial irregularities, because they can make the patient appear to have a large refractive error.
If the surface is fine, I consider using Fayetteville, Ark., surgeon James McDonald's contact-lens assisted pharmacologically induced keratosteepening. This involves using a contact lens and Acular to adjust the shape of the epithelium to counteract an overcorrection. The patient instills the Acular and then stays in the contact lens 24 hours a day for four to six weeks. I've used this method in a handful of small overcorrections, and have had positive results.
You can also titrate the potency and/or the duration of the postop steroids to modulate healing. If a myope is healing aggressively, the refraction can regress. If this occurs, you can bump up the frequency of the steroid drop to try to reduce the healing process and produce a flatter corneal curvature. Alternatively, with an overcorrection, you can reduce or eliminate the steroids, which will allow the healing to continue. You can also use a more- or less-potent steroid, based on whether you're dealing with an under- or overcorrection, respectively.
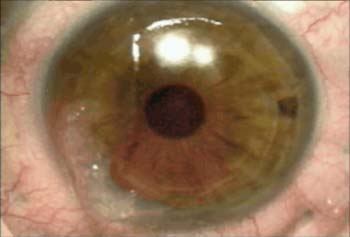
• Stromal incursion. This can occur when an epithelial separator makes a cut into stroma. If the cut occurs in the visual axis, you must carefully replace the flap and abort the case. If it's in the far periphery, you could potentially continue with the laser ablation and slide the flap back afterward.
For stromal incursion in the visual axis, the prognosis can be good. In one hyperope in which this complication occurred, his refraction slowly improved to a stable level (20/20 best corrected) over three months.
Dr. Trattler is in private practice, and lectures widely on refractive surgery issues. He would like to thank his colleague, Carlos Buznego, MD, for his contributions to this article.
1. Autrata R, Rehurek J. Laser-assisted subepithelial keratectomy for myopia: Two-year follow-up. J Cataract Refract Surg 2003;29:661-668.
2. Autrata R, Rehurek J. Laser-assisted subepithelial keratectomy and photorefractive keratectomy for the correction of hyperopia: Results of a 2-year follow-up. J Cataract Refract Surg 2003;29:2105-2114.
3. Shah S, Sebai Sarhan AR, Doyle SJ, et al. The epithelial flap for photorefractive keratectomy. Br J Ophthalmol 2001;85:393-396.
4. Stojanovic A , Ringvold A, Nitter T. Ascorbate prophylaxis for corneal haze after photorefractive keratectomy. J Refract Surg 2003;19:3:338-43.