A disease like blepharitis is a classic example. There are several types of blepharitis and multiple causes, and your armamentarium can be rendered ineffective if you don’t accurately identify the precise nature of the problem. Only by understanding the disease can a physician effectively diagnosis and treat it. Thus, deciphering and identifying the unique signs and symptoms of blepharitis pave the way for effective treatment.
The Blepharitis Basics
Blepharitis is an inflammatory condition associated with redness, itchiness and flaking and crusting of the eyelids, found in both children and adults. Classifications of the disease range from chronic to acute, and anterior vs. posterior. Anterior blepharitis is typically the result of Demodex mite infestations, or bacteria found on the eyelid. Seborrheic blepharitis is one type of anterior disease in which patients often find flaking in their eyebrows or lashes. The more typical type of blepharitis is posterior, known as meibomian gland disease or dysfunction.
As well as causing general discomfort and inflammation for patients, blepharitis can also affect the outcomes of cataract and refractive surgery, so it’s important for physicians to remain vigilant for this often-overlooked condition.
Symptoms
In a study looking at the symptoms and causes of dry-eye disease, researchers noted that up to 20 percent of adults over the age of 45 reported some discomfort from blepharitis and meibomian gland dysfunction.1 From there, the reported cases of blepharitis increase to the point where it’s present in 68 percent of patients over the age of 60.2 Because of the prevalence of the disease, physicians need to be on the lookout for symptoms that indicate either acute or chronic blepharitis.
Some of the most common symptoms and signs of blepharitis are:
-lid-margin inflammation or redness;
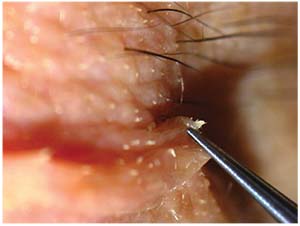
-collarettes around the base of each eyelash;
-the thickening and cloudiness of the clear oil of the meibomian glands;
-lash loss;
-complaints of itching or a tickling sensation around or on the eyelids;
-and the presence of Demodex mites.
Telltale Causes
Demodex mites. A Demodex mite infestation can incite blepharitis. In a 2010 study on the role of Demodex mites in blepharitis, researchers found that the incidence of Demodex infestations increases with age, affecting 84 percent of the population at age 60 and 100 percent of those older than 70 years.3
The two species of Demodex found to cause blepharitis are Demodex folliculorum (anterior blepharitis, with issues associated with the eyelashes) and Demodex brevis (posterior blepharitis, with issues related to the meibomian gland and keratoconjunctivitis).
Staphylococcal infection. “This type of anterior blepharitis is a r
 |
| A case of blepharitis displaying eyelid inflamation and collarettes around the base of the lashes. |
Seborrheic. “Patients with seborrheic blepharitis usually complain of eyelash flaking, along with the redness and irritation you typically see with other types of blepharitis,” Dr. Wolle says. Due to these symptoms, it’s often mistaken for other common skin conditions such as eczema, so it may be overlooked.
Rosacea. Due to the nature of rosacea, this skin condition also affects the eyes of patients, paving the way for blepharitis to take root, so the two often present hand-in-hand.
Meibomian gland dysfunction. Because the meibomian glands don’t secrete enough oil into the tears, they evaporate too quickly, which can result in dry eye. “This one is tricky, because blepharitis can either be the cause or the result of meibomian gland dysfunction,” says Dr. Wolle. “MGD is usually identified by tear-duct obstruction and changes in glandular secretion, which will lead to the irritation you usually see with blepharitis.”
Diagnostic Issues
Because so many patients present with some sort of untreated blepharitis, identifying and diagnosing the disease can be a tricky issue. Robert Noecker, MD, an ophthalmologist based in Fairfield, Conn., discusses the challenges of identifying blepharitis before it gets into its acute stages. “It’s a double-edged sword. In some ways, diagnosis is relatively straightforward, but on the other hand, blepharitis flies under the radar a lot because it usually comes in the context of other things,” he says. “Other types of dry-eye issues or ocular surface diseases and such can sometimes come packaged with blepharitis. Patients taking glaucoma medication probably all have some degree of blepharitis. So if a doctor isn’t careful, and looking for Demodex mites or crusting on the lids and lashes, the symptoms of blepharitis might be dismissed as those of dry eye or some other issue.”
Dr. Wolle highlights the important role that the patient’s age plays in her diagnosis and personalized treatment. “Usually it’s present in elderly women, but you can find it in the whole gamut,” she says. “However, because our older patients are usually suffering from some other eye disorder (typically dry eye and/or glaucoma), and are on medications for said disorder, we have to be careful about administering another medications that may interact with what they’re already prescribed.”
Dr. Noecker also discusses the importance of demographics and how they can affect the severity of the disease. “Immune problems like cirrhosis also exhibit symptoms and cases of blepharitis. Blepharitis tracks into the portions of the population that typically have eye concerns (dry-eye patients, glaucoma), so once you get into the later stages of your life, you’re more likely to have it,” he says. “But it can happen to anyone. Allergy season can contribute to flare-ups. Treatment just comes down to the chronicity of it.”
Dr. Noecker continues, providing some advice for a quick and accurate diagnosis. “It’s like everything else. The more you look for it, the more you’ll find it. In an exam, sometimes you have the tendency to just go for the cornea, and not look at the lids or the meibomian glands. This contributes to the ocular surface dysfunction,” he says. “Following patients’ questionnaires is important, too. You have to look at what they write and pay close attention to both signs and symptoms. Just performing a quick external examination before they pop their head into the slit lamp makes a big difference, too. The due diligence can get away from you sometimes.
“It’s just saying, ‘Okay, I’m going to take
 |
| In this case, a patient presented with both rosacea and Demodex mites. |
Dr. Wolle also provides some advice for identifying blepharitis. “The eye exam really starts with looking at the lids, and that’s where we sometimes don’t focus. Or maybe it’s not as extreme as one expects. Maybe there are just a few collarettes hanging on the base of the lids, so they are overlooked,” she says. “Those types of blepharitis are more extreme because of the mites. Sometimes you don’t see the crusting or the mucus on the lashes, so one should really focus on the lashes as well as the lid margin. Paying close attention to the lashes and lids will allow you to catch most of the cases.”
Treatment Options
Because of the different types of the disease, the treatments (or, rather, management) vary. Underlying causes and conditions should be addressed first (dry eye, etc.) so that recurring bouts of blepharitis are minimized. Once underlying causes are taken care of, symptoms can be tackled, experts say.
Dr. Wolle highlights the different approaches to treating this problematic disease. “For the chronic treatment of blepharitis, the main therapy is going to be warm compresses for at least five minutes, followed by lid massages or scrubs twice a day to get rid of recurring bouts,” she says. “If it’s more than a mild bout, the patient can apply some topical antibiotic ointment to the eyelids during or after the warm compresses to help manage it.” While these lid scrubs and compresses aren’t cures for the condition, they can provide relief, while eliminating lid-margin debris and bacteria.
“Now for acute blepharitis, you have a few options,” she says. “Typically, you can administer an antibiotic either orally or topically. You may also consider using a weak steroid if it’s a really bad bout. You’ll quiet it down, but you wouldn’t want to use a steroid for more than a few weeks because it could damage the eye.” She adds that one must also be careful in administering these steroids since their long-term use could be problematic in their interaction with other medications, leading to other complications outside of blepharitis. As of today, the most common treatment is a combination of corticosteroid therapy with antibiotics to alleviate the symptoms of blepharitis. The persistence of blepharitis requires several repeat visits to effectively treat the disease, as treatment/management will likely be ongoing.
“When Demodex mites are identified as being present, the treatment is straightforward. However, because of the nature of the mites, they can multiply at a rapid pace, so they must all be removed,” Dr. Wolle says. “The best way to go about this is through lid scrubs and tea tree oil, which cleans the dandruff from the lash root and irritates the mites enough for them to move out of the skin. Like anything else, maintaining proper hygiene is essential.”
Getting Ahead of the Curve
In order to manage and prevent bouts of blepharitis, patient education is essential. Dr. Wolle discusses how to best prevent the development of blepharitis before you step into the exam room. “Let your patients know what to look for. Tell them to be good about their eyelid hygiene. Even if they don’t have an issue with blepharitis, they should be washing their eyelids in general to prevent any issues of colonization,” she says. “For women especially, they should be careful about their makeup. They tend to reuse their makeup or don’t change it for a period of time, and from that you can get organisms that can end up causing blepharitis. Suggest that they try to be as hygienic as they would be with their teeth and their faces.” Dr. Wolle does, however, note, “Some of it isn’t that preventable. There are genetic issues that people have which are hard to get around, but that’s a whole different category.”
With proper hygiene and lid scrubs, most patients with blepharitis can have their symptoms alleviated. Proper physician diligence can help patients get ahead of a chronic flare-up and avoid the nuisance of a corticosteroid and antibiotic regimen. However, it must be noted that even if the symptoms are gone, there is always the possibility of a recurring problem, so diligence with eyelid care is essential to avoideng and overcoming persistent bouts of blepharitis. REVIEW
Drs. Wolle and Noecker have no financial interest in any product discussed in the article.
1. Brewitt H, Sistani F. Dye eye disease: The scale of the problem. Surv Opthalmol 2001;45:199-202.
2. Macsai M. The role of omega-3 dietary supplementation in bleparitis and meibomian gland dysfunction. Trans Am Ophthalmol Soc 2008;106:336-356.
3. Liu J, Sheha H, Tseng S. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol 2010;10:5:505-510.



