Cataract surgeons on our National Panel appear to be adopting a wait-and-see attitude regarding new technology such as the femtosecond laser for cataract surgery, and haven’t yet taken to bimanual cataract surgery or mixing and matching presbyopic intraocular lenses. Instead, they’re sticking with what’s been working for them in their practices, such as toric IOLs, incisions around 2.7 mm wide and manual capsulorhexes.
Those are just some of this month’s results from our survey on cataract surgery technique. This month, 35 surgeons, or 7 percent of our 500-surgeon sample, replied with their views on cataract surgery.
General Techniques
Clear corneal wounds and the use of topical anesthesia are still the mainstays of our panelists’ cataract surgery technique.
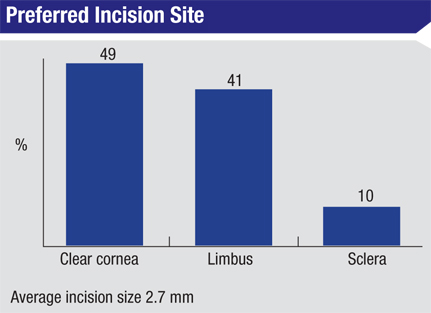
Forty-four percent of the respondents use clear corneal incisions, 32 percent prefer limbal wounds, 21 percent like scleral incisions and 3 percent do a combination of limbal/corneal wounds. The average incision width is 2.7 mm. “The clear corneal incision seals well and induces minimal to no astigmatism,” says Westerly, R.I., surgeon David Rivera. A surgeon from Texas, however, prefers limbal incisions. “The limbal incision heals well and no scar is seen.”
Richard Erdey, MD, of Columbus, Ohio, however, is in the scleral incision camp. “I like that the scleral incision has an excellent seal and is no-stitch,” he says. “It has better wound healing compared to clear cornea.” An Illinois surgeon agrees, saying that scleral incisions are “fast-healing.”
|
However, not all the surgeons are content with the type of incisions they currently use, and a quarter of them are considering switching to a different wound location. Two-thirds of surgeons who are contemplating switching say they’d probably switch to a limbal incision, 23 percent say clear corneal could be the way to go and 10 percent are thinking of moving to scleral wounds. “Limbal wounds heal better,” says a Massachusetts surgeon considering moving away from clear corneal incisions.
One thing most panelists agree on is that bimanual phacoemulsification isn’t the procedure for them. Eighty-four percent don’t use the technique. “There’s no benefit to it,” says Luther Fry, MD, of Garden City, Kan. A surgeon from Indiana concurs, saying, “Bimanual phacoemulsification is not practical, especially with my preferred intraocular lenses requiring larger than 2.2-mm incisions.” Some surgeons don’t necessarily dislike the technique, but there are factors preventing them from trying it. “I don’t have the equipment,” says Rhode Island’s Dr. Rivera. A New York surgeon leaves the door open for possibly adopting the technique in the future, but for now, says, “I’m not comfortable enough with bimanual phaco to do it yet.”
|
As a possible alternative to bimanual phaco, 28 percent of the surgeons say they use a coaxial micro-incision surgical technique, which doesn’t separate the infusion and aspiration as bimanual does, yet can be performed through a small, potentially 1.8-mm, incision. “Alcon’s C-MICS, using a 2.2- to 2.4-mm incision, works for my preferred intraocular lens,” says a surgeon from Illinois. A surgeon from Tennessee says he uses a variety of C-MICS to operate through a 1.8-mm incision, though it doesn’t adhere to the classical definition. “I kind of use C-MICS: If I can suck the lens into the anterior chamber, I will do a one-handed phaco without the second hand dividing,” he explains. A Florida surgeon says he prefers to use C-MICS because it’s “easy.”
Most surgeons, though, are waiting to see more from C-MICS before they’ll jump on the bandwagon. “At this point, I don’t feel that it offers any additional benefit,” says a surgeon from Vermont.
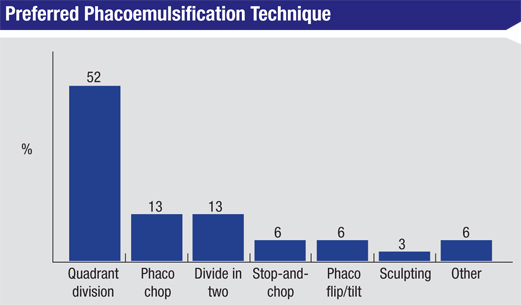
When it comes to breaking up the nucleus, quadrant division is preferred by 52 percent of panelists, followed by phaco chop (13 percent), divide in two (13 percent), phaco flip/tilt (6 percent), stop-and-chop (6 percent) and sculpting (3 percent). Six percent use a combination of these techniques. “Phaco chop is easy to do and efficient,” says a surgeon from Vermont. Dr. Rivera also uses a phaco-chop technique, describing it as “fast—it minimizes lens manipulation.”
A proponent of phaco flip/tilt likes it because, he says, “It protects the posterior capsule.” A surgeon from Tennessee describes his technique as a “Modified Brown technique.” Says he, “I use a Mercedes tri-cut, then, if the lens comes out, I use a Brown technique. If it doesn’t come out, I use a divide-and-conquer. This approach has been safe and effective.” Ohio’s Dr. Erdey uses a different technique from the rest. “It’s a phaco backcrack/tilt/chop,” he says. “It is a very efficient nuclear disassembly that uses very little phacoemulsification energy, like a phaco assist.” A surgeon from Indiana, however, says that a “combination of pre-chop and stop-and-chop” is the most efficient technique in his hands.
|
Surgeons also shared their personal tips and techniques that they feel make a difference in their cataract outcomes. “Plan your surgery well,” advises a surgeon from Indiana. “That way you can concentrate on the task at hand once you’re in there. Also remember: Safety first,” he says. New Jersey’s Dr. Greco says, “Take extra time to do a good capsulorhexis.” Marc Safran, MD, of Liverpool, N.Y., has a tip for surgeons about to break up the cataract: “Before placing the chopper at the equator, I like to give it more room by slightly depressing the nucleus with the phaco tip.” Before closing the case, a surgeon from Florida says he likes to “irrigate through the paracentesis to identify any residual nuclear fragments.”
Other worthwhile tips include:
|
- “Listen to the patient. For instance, if a multifocal IOL isn’t working, fix it,” says a surgeon from Tennessee.
- Use epi-Shugarcaine for the Flomaxed iris.
- Tilt the patient’s head a little toward the operated side.
- Avoid aggressive aspiration flow rates.
Managing Astigmatism
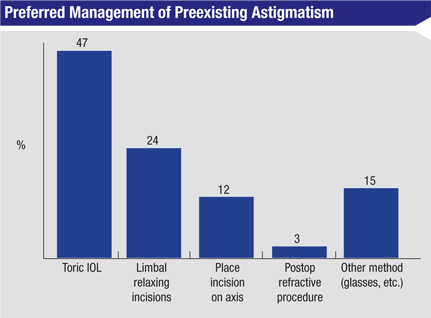
Toric IOLs, chosen by 42 percent of the panelists, are still a popular option with respondents who have to deal with a cataract patient’s astigmatism. Twenty-four percent of the surgeons prefer limbal relaxing incisions, 15 percent use another method such as prescribing spectacles postop or combining LRIs with toric lenses, 12 percent place the entry incision on the axis of astigmatism and 3 percent will use a postop refractive procedure.
“A toric IOL has better accuracy and stability than a limbal relaxing incision,” says Dr. Fry. Dr. Rivera also prefers to use a lens. “The toric IOL is the most precise for me,” he says. “Also, I don’t have access to a laser.” A surgeon from Vermont says, “The toric IOL gives excellent results.” An Indiana surgeon, however, prefers LRIs. “They’re cheaper than lenses, quick, and enjoy good patient acceptance.”
Dr. Erdey says he’ll use a toric lens if the patient’s astigmatism is against-the-rule, but scleral recession if it’s with-the-rule. “Modification of the scleral tunnel with scleral recession is very effective,” he says.
|
Anesthesia Options
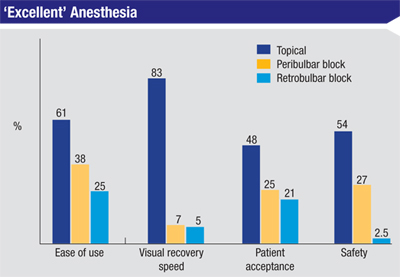
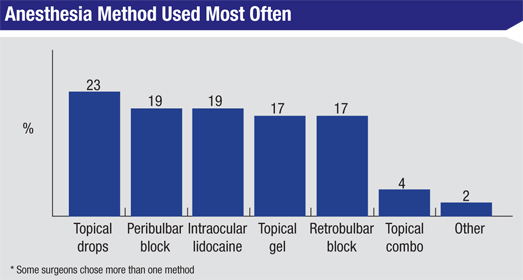
Forty-two percent of the surgeons use some type of topical anesthesia in their cataract surgery cases; 22 percent use topical drops, 15 percent use a gel and 5 percent use some variety of topical combination. Twenty-two percent of the respondents say they use intraocular lidocaine, 18 percent each use peribulbar blocks or retrobulbar blocks.
“Topical anesthesia is the method that works the best for me,” says a surgeon from Virginia. Ronald May, MD, of Deerfield, Ill., however, prefers to use a retrobulbar block. “The retrobulbar block offers patient and surgeon comfort,” he says. A California surgeon says that retrobulbar blocks “have the best patient acceptance” in his practice. “Topical anesthesia is stressful for the patient and the surgeon,” he adds.
Though cataract surgeons today may feel pressure from all sides to be more and more efficient with their procedures, a surgeon from Nebraska reminds that haste can sometimes make waste. “Don’t rush,” he says. “Slow down to speed up.” REVIEW