The introduction of minimally invasive glaucoma surgery has ushered in a variety of implantable and surgical devices characterized by an ab interno approach. As an alternative that’s finding its niche in between topical drops and trabeculectomies and tube shunts, the MIGS space is also finding its way into the treatment algorithm of an increasing number of surgeons. Some of these surgeons seek to further maximize the benefits of MIGS by combining different devices and procedures. A look at this twist on a fairly new treatment modality follows, along with insights from surgeons who’ve done it.
Multiple Mechanisms
Steven R. Sarkisian Jr., MD, founder and CEO of Oklahoma Eye Surgeons and clinical professor of Ophthalmology at the University of Oklahoma in Oklahoma City, says that combining MIGS makes sense because attempting to manage IOP by one mechanism can be shortsighted. “We can’t really cling to the standard of, ‘Glaucoma is an outflow problem, so the only appropriate surgery is an outflow-adjusting procedure.’ That’s really not plausible if you look at how we take care of glaucoma medically,” he says. “So we’re seeing more and more people looking at the inflow side of the equation and treating that more aggressively. It’s interesting to see this shift. We now have multiple ways of modulating aqueous. You could increase outflow in three ways, either through the suprachoroidal space, the canal or the subconjunctival space. Moreover, aqueous flow can be altered by decreasing production. MIGS combinations can be complementary if they’re done in just the right way.
“To illustrate how this works, let’s look at how cardiologists treat blood pressure,” he continues. “It used to be that to treat high blood pressure, doctors would start someone on one medication, such as an oral beta-blocker. They’d max that oral beta-blocker out to the highest dose, and if that wasn’t adequate to treat the blood pressure, they’d keep them on that very high dose of beta-blocker and then also start them on a water pill like hydrochlorothiazide, for example. Whatever they started with, the goal was to max out one drug, then add another and then max out that one and add another one. Now, however, we’re seeing a lot more cardiologists initiating treatment with several drugs at the same time, all at the lowest possible doses—and taking advantage of the complementary mechanisms of action. They may not always be able to tell you which medication is being the most effective in lowering blood pressure—the beta-blocker, the calcium channel blocker or the ACE inhibitor—but nonetheless, they’re starting people on this low-dose cocktail to help them achieve more control with fewer side effects.”
Endoscopic cyclophotocoagulation is a treatment aimed at modulating inflow by targeting the cilary body epithelium; Dr. Sarkisian notes that it’s a popular implant-free component of combined MIGS procedures. “ECP has been used in combination with every MIGS surgery out there—whether it’s the Hydrus (Ivantis; Irvine, California); the Trab360 (Sight Sciences; Menlo Park, California); GATT (iTrack; Ellex, Mawson Lakes, South Australia, Australia); the ABiC (Ellex); the Kahook Dual Blade (New World Medical; Rancho Cucamonga, California); the Trabectome (NeoMedix; Tustin, California); and formerly, the CyPass (Alcon; Fort Worth, Texas),” he says.
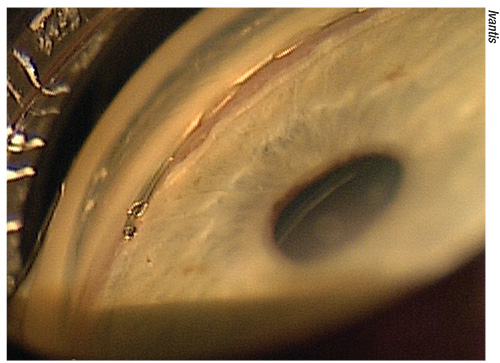 |
| Oklahoma City surgeon Steven Sarkisian will combine the Hydrus (above) with another MIGS procedure. |
Eric D. Donnenfeld, MD, founding partner at Ophthalmic Consultants of Long Island, also thinks stacking MIGS is a viable way to customize glaucoma treatment. “The management of glaucoma is based on first, the severity of the glaucoma; and second, the intraocular pressure. So for patients with mild disease, without significant visual-field loss and using one medication, you certainly want to do the simplest procedure possible—and that would be a single-MIGS procedure or two of the same type of MIGS. For patients who have more advanced glaucoma, who are on multiple medications and need more pressure control, I think combining MIGS is a very reasonable thing to do,” he says. “I don’t do it a lot, but I have certainly done it, and it’s been very successful. I’ve put in the iStent Supra and the regular iStent (Glaukos; San Clemente, California) in the same eye, combining a suprachoroidal and trabecular meshwork bypass device in the same patients,” he says. “I think there’s a role for using them both together.”
Dr. Donnenfeld says that he combined the iStent with the iStent Supra when taking part in clinical research in Yerevan, Armenia (ClinicalTrials.gov Identifier: NCT01456390). “We’ve followed the patients now for about five years, and they’re still doing well,” he says, adding that he hasn’t combined the devices in the United States.
His experience with multiple stents, including combining implants that target different areas, has prompted Dr. Donnenfeld to develop a straightforward treatment nomogram intended to maximize the benefit of MIGS. “I think the more stents you put in, the better the pressure control, so I follow a very simple rule of thumb: If your patient takes one medication, it’s reasonable to use one MIGS procedure; if they have two or more medications, then it’s reasonable to either use two of the same type of MIGS—or preferably, in the future, two different types of MIGS, such as a suprachoroidal device and a trabecular meshwork bypass,” he says. “Optimally, you’d get the patients off their medications completely,” he continues. “But it isn’t reasonable to think you’ll achieve that with every patient, so the goal is to get the pressure as low as you can in a safe manner. For a lot of patients, we can and do get them off the medications completely, but certainly not everyone.”
An Abundance of Caution
Safety and rapid recovery are two of the calling cards of MIGS procedures, but does doing two types of procedure in one surgery create more risk than the benefits can justify? “I think MIGS procedures are extremely safe,” says Dr. Donnenfeld. He adds that some devices carry more risk than others, though. “I think the suprachoroidal MIGS do play a role, but there is some increased risk with those procedures, so you need to weigh the risk against the reward you’ll have of lowering the pressure,” he cautions. “There are a lot of different combinations you can use. I think some more research still needs to be done on what the best combinations are, but I do believe that different pathways used together might be best. That’s why I think that a suprachoroidal and a trabecular meshwork bypass combination would be a very reasonable approach to take.”
Before considering combining MIGS, Dr. Donnenfeld says he would make sure his patient understood the potential risks and benefits, just as he would prior to any other procedure. “I would have a conversation with patients who have glaucoma about what’s in their best interest, and the best way of approaching it,” he says. He adds that as a refractive, cornea and cataract specialist, he doesn’t hesitate to direct patients he considers too advanced in their disease to a glaucoma specialist. “The real decision that needs to be made by a lot of patients is whether they will need to go to a more advanced procedure that has greater efficacy, but also has greater risk; or whether they’ll try a MIGS procedure first. I think that most patients—and many doctors—would agree that the most atruamatic, safest procedure should always be done first. If the patient does well, then there’s no need to go on to a more advanced procedure such as a trabeculectomy or a tube shunt. I am very much in favor or using MIGS to the full extent of their efficacy, even in patients who are borderline, before going to a more advanced treatment if necessary,” he says.
Dr. Sarkisian concurs that combining MIGS represents an opportunity to treat more severe cases of elevated IOP earlier without defaulting to trabeculectomy. “It will soon be the case that if the only glaucoma surgery you’re doing is trabeculectomy, you aren’t going to be a very busy glaucoma surgeon,” he says.
“The MIGS space allows you to expand to a more severe level of glaucoma cases,” he continues. “The iStent is approved for mild to moderate glaucoma. Just because the FDA has indicated it for mild to moderate disease, that doesn’t mean you’re limited to using it only for those cases: It means that’s how the study was done, which limits the company’s ability to market the device. Is it possible that in the name of saving money, insurance companies will decide not to pay for things unless they’re perfectly on-label? Yes—and that’s wrong.”
Dr. Sarkisian says that Alcon’s August 2018 withdrawal of the CyPass Micro-Stent, a suprachoroidal stent designed to enhance uveoscleral outflow, has affected his combined MIGS practice. Five-year data from the COMPASS XT study showing an increased rate of endothelial cell loss in patients who’d undergone a CyPass procedure plus cataract surgery, versus those who’d had cataract surgery alone, prompted the withdrawal. The increased ECL appeared to be correlated with shallower implantation of the stent.
“We need to advocate strongly that the CyPass be brought back to market,” he says. “The directions for use should be modified so that doctors know how to implant it correctly, or perhaps Alcon should tweak the design. That would probably take a very long time, though. It’s important not to view the CyPass as an opportunity to badmouth MIGS in general.
“No longer having it does change my mix,” he acknowledges. “I’m looking forward to the iStent Supra’s release.” The iStent Supra is currently CE-marked but doesn’t have FDA approval. The iStent inject, which allows surgeons to implant two trabecular microbypass stents from a single injector, won FDA approval in late 2018. Like Dr. Donnenfeld, Dr. Sarkisian has used the suprachoroidal stent abroad. “I was part of the Glaukos MIGS study group in Armenia where we combined first and second-generation iStents with the third-generation iStent (Supra) in the same eye. They’ve demonstrated that combining first-generation iStents and the Supra, the third-generation device, with prostaglandins has achieved really low intraocular pressures, and that’s a big deal,” he says.
The Visco360 (Sight Sciences), an ab interno microcatheterization system for transluminal viscodilation of Schlemm’s canal, together with a trabecular microbypass implant, is a current staple of his combination-MIGS armamentarium. “Right now, with regard to mixing MIGS, combining Visco360 with iStent or Hydrus is probably my number-one combination,” he says. It was closely followed by the Omni (Sight Sciences) with the CyPass, but that’s now impossible. Before that, it was combining the iStent with ECP.” He’d also combine ECP with the Trab360, a manual trabeculotomy cutter, for a procedure he still considers “an excellent option.” He reports that Medicare has been bundling ECP plus iStent and ECP plus Trab360. “It’s infuriating because there is separate overhead associated with each of those two procedures that doesn’t overlap,” he says.
“The biggest problem is that you don’t get paid for them yet,” says Dr. Donnenfeld of combined MIGS procedures. “There are financial disincentives here, but in Europe it’s very commonly done.”
Looking Ahead
Dr. Sarkisian looks forward to a time when surgeon experience and joint decision-making between doctor and patient will hold more sway in the choice to combine MIGS. “The question of two implants in the same eye is a complicated one that gives a lot of people anxiety, for a variety of reasons,” he says. “I think that if people weren’t worried about what insurance companies and Medicare were going to do, if it was just between the doctor and the patient, we’d see a lot more combining of multiple MIGS at the same time. I have had patients pay cash for multiple stents, and
other surgeons have as well, particularly in patients that have earlier stages of glaucoma where stents are a standalone procedure. You don’t have to do cataract surgery to put in an iStent or a Hydrus, for example. That’s just how they’re FDA approved. They’re actually very effective by themselves. I think that once we get standalone indications for a lot of these devices, some of these issues will go away.”
Dr. Sarkisian is skeptical that anyone will design large randomized controlled trials to compare the efficacy of different MIGS combinations, however. “I don’t believe there are going to be large clinical trials comparing combinations of this or that MIGS device versus not combining them. No one’s going to fund those studies,” he says. “But I do foresee future standalone indications for the iStent. It’s public knowledge that the next phase for the iStent is going to be the iStent Infinite, which is three iStents at one time using the Inject model as a standalone indication. I also believe there will by standalone indications for the CyPass if it’s brought back, and the iStent Supra. I think standalone indications will be the watershed moments for these stents, and we’ll see more general adoption, because we won’t be constrained by the billing and reimbursement issues.”
He remains confident in the future of MIGs in general, including combined procedures. “After all, we’re treating a blinding illness: The alternatives to MIGS are often not acceptable,” says Dr. Sarkisian. “What are we supposed to do—just put patients back on four medications? There are patients who would’ve gotten phaco-trabculectomy or phaco-ExPress in the past, and would’ve been at risk for wipeout syndrome and hypotony and endophthalmitis, but now they’re not facing those risks. So MIGS could allow us to really revolutionize the treatment of glaucoma. Does it always work? Of course not, but neither does trabeculectomy. I’m sleeping a lot better at night knowing that I can personalize the care I give and not cause the blinding complications we can see with traditional glaucoma surgery.”
Dr. Donnenfeld predicts that MIGS—alone or in combination procedures—will one day have an added feature to boost their efficacy. “In the future, there will be MIGS devices that will also be medication-delivery systems. That will once again give us another option for prolonged pressure control, via a device that will not only lower the pressure surgically, but will also provide medication intracamerally to treat the glaucoma. That’s not here today, but it’s coming,” he says.
“We need to keep pushing forward and keep fighting for better treatments,” Dr. Sarkisian concludes. “In the end, we’re here to help our patients with the best technology we can use. That’s how we fulfill our oath. It’s an exciting time to be able to do that.” REVIEW
Dr. Donnenfeld is a consultant for Glaukos, Ivantis and Alcon. Dr. Sarkisian is a consultant/advisor to Alcon (He’s received lecture fees and grant support.); Sight Sciences (He owns equity in the company and has received grant support.), and Glaukos (He has received grant support.) He is also a consultant-advisor to Allergan, Beaver-Visitec International, Katena, New World Medical, Santen and Omeros.



