A multivariate analysis from the European Glaucoma Prevention Study cites baseline age, vertical cup-to-disc ratio, vertical C/D ratio asymmetry, and pattern standard deviation as good predictors of the onset of open-angle glaucoma, and central corneal thickness as a powerful predictor of the development of OAG. These results agree with the findings of the Ocular Hypertension Treatment Study and support the need for a thorough evaluation of patients with ocular hypertension, the authors say.
The randomized, double-masked, controlled clinical trial included 1,077 patients >30 years old, at 18 European centers. Inclusion criteria: intraocular pressure, 22 to 29 mmHg; two normal and reliable visual fields (on the basis of mean deviation and corrected PSD); and a normal optic disc.
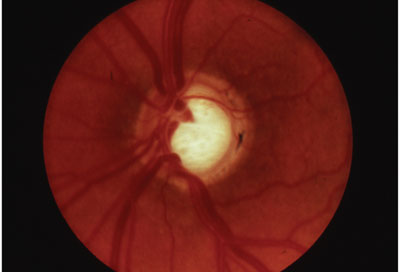
Intervention involved treatment with dorzolamide or a placebo (the vehicle of dorzolamide) in one or both eyes. Main outcome measures were VF and/or optic disc changes. Baseline demographic and clinical data were collected before randomization, except for corneal thickness measurements, which were determined during follow-up.
(Ophthalmology. 2007;114:3-9.)
European Glaucoma Prevention Study (EGPS) Group; Miglior S, Pfeiffer N, Torri V, Zeyen T, Cunha-Vaz J, Adamsons I.
Synchrony Shows Promise in Pilot
The Synchrony dual-optic intraocular lens shows promise as an option to provide accommodative function in pseudophakic patients, say investigators, following a prospective, noncomparative case series with retrospective control.
The series included 21 patients (26 eyes) scheduled for small-incision cataract extraction by phacoemulsification with implantation of the Synchrony dual-optic accommodating IOL (Visiogen) (accommodating IOL group) and 10 patients who had small-incision, phacoemulsification with implantation of a monofocal, single-optic IOL at least six months previously (control group). Patients were examined one, three, six and 12 months after surgery. Defocus curves in the accommodating IOL group were compared with those in the control group. The main outcome measures were postoperative distance uncorrected and best corrected visual acuity; near uncorrected, distance corrected, and near corrected visual acuity; and accommodative range based on defocus curves.
Twenty-four eyes were available at the six-month follow-up visit. All eyes had best corrected distance visual acuity of 20/40 or better, and 19 eyes (79 percent) had an uncorrected distance visual acuity of 20/40 or better. Uncorrected near visual acuity was 20/40 or better in all eyes. With distance correction, 23 eyes (96 percent) had an acuity of 20/40 or better at near. Defocus curve analysis suggested a mean accommodative range of 3.22 D ±0.88 (SD) (range 1 to 5 D) in the accommodating IOL group and 1.65 ±0.58 D in the control group (range 1 to 2.5 D) (p<.05).
(J Cataract Refract Surg 33:47-52.)
Ivan L. Ossma, MD, MPH, Andrea Galvis, MD, Luis G. Vargas, MD, Michelle J. Trager, MD, M. Reza Vagefi, MD, Stephen D. McLeod, MD




