One issue that often arises when managing a glaucoma patient with exfoliation syndrome is whether the patient should be tested for systemic conditions that might be related to the presence of exfoliation. We know that exfoliation material—an extracellular accumulation of macromolecules with a core of elastin fibers—can form inside the eye, obstructing the outflow system in the trabecular meshwork and leading to elevated IOP and optic nerve damage. In fact, exfoliation syndrome is the leading cause of secondary open-angle glaucoma around the world. However, we also know that in these patients the exfoliation material appears in tissues in other parts of the body. When an individual has exfoliation syndrome, very minute quantities of exfoliation material can be found in organ systems such as the skin, pulmonary tissue, heart and gallbladder. The question is, are those other deposits of clinical importance?
In fact, there’s a long list of possible clinical associations between exfoliation syndrome and other conditions that are discussed in the literature. Those possible associations include myocardial infarction, cerebrovascular disease, renal vascular disease, abdominal aortic aneurysm, elevated homocysteine levels, sensorineural hearing loss, and recently, inguinal hernia and pelvic organ prolapse. Some doctors also believe there may be an association between exfoliation syndrome and Alzheimer’s disease.
So: Does the presence of exfoliation syndrome warrant us recommending that our patients get a workup for other systemic conditions that might be associated with exfoliation syndrome?
Evidence of Systemic Impact
There’s no question that the presence of exfoliation can alter physical structures in the body. For example, my colleagues and I have conducted nailfold capillary microscopy in patients with different kinds of glaucoma. This is a useful part of the body to study because the capillary structure can be observed noninvasively. We put some cedar oil on the fourth and fifth digits of the nondominant hand, making the skin translucent; then, our microscope provides 300X magnification and allows noninvasive visualization of the nailfold capillaries. (See images.) These capillaries are elongated, hairpin-loop vessels resembling tiny skyscrapers; under the microscope you can see the blood coursing through them.
 |
| Healthy capillaries. |
One of the things we discovered was that in exfoliation syndrome, the nailfold capillary morphology is quite different from that seen in healthy patients. The vessels are markedly tortuous, for reasons we don’t completely understand, as we recently published.1 What’s interesting is that iris tissue also has these terminal hairpin-loop capillaries, which you can see if you study them under high magnification with fluorescence microscopy. Furthermore, the vessels in the iris are also affected by exfoliation syndrome; their walls become abnormal, encased with ex-foliation material. It’s possible that this encasement of the vessels also happened in the nailfold, contributing to the vessel tortuosity, although we don’t have the evidence to prove it. In any case, this alteration of the nailfold capillaries in the presence of exfoliation syndrome is another indication that the syndrome can have an impact outside the eye.
Other interesting findings have also turned up relating to different diseases. For example, my colleagues and I studied Alzheimer’s disease at Boston University; we performed nailfold capillary microscopy on those patients. It turned out that they also had significant nailfold capillary tortuosity compared to controls.2 This is intriguing, because in Alzheimer’s disease cerebral blood vessels are encased in amyloid plaques; in exfoliation syndrome iris vessels are encased in exfoliation material. Perhaps in both cases this is contributing to the tortuosity of the blood vessels.
However, as stated above, this leads to the question: Are these non-ophthalmic manifestations of clinical importance? Do these manifestations indicate, for example, that some percentage of exfoliation syndrome patients are going to get Alzheimer’s disease?
Examining the Data
Despite the long list of possible clinical associations with exfoliation syndrome discussed in the literature, the evidence supporting those associations is far from conclusive. For example:
 |
| The presence of exfoliation is known to alter physical structures outside of the eye. Here, microscopy reveals the impact of exfoliation on nailfold capillaries. |
• Alzheimer’s disease. Consider the similarities (or lack thereof) between exfoliation syndrome in the eye and Alzheimer’s disease:
— Amyloid is important in Alzheimer’s disease, but immunohistochemical studies don’t find amyloid in the blood vessels of exfoliation patients.3
— Certain peptides can be detected in the blood and cerebrospinal fluid of Alzheimer’s disease patients; they’re not found in the aqueous humor of exfoliation syndrome patients.4
— What we know about the genetics of the two diseases doesn’t jibe; for example, there’s a fairly robust association between common variants of LOXL1 and exfoliation syndrome, but these genetic variants are not associated with Alzheimer’s disease.5
— A population-based study done in China found no association between cognitive function and ex-foliation syndrome.6
So although Alzheimer’s disease and exfoliation syndrome share some common pathophysiologic motifs, they’re not pathogenetically linked—at least based upon the data we have so far.
• Cardiovascular disease. A recent meta-analysis of 16 studies looked at associations between various cardiovascular manifestations and exfoliation; all of the studies found a positive association.7 However, there are reasonable concerns about whether these results were con-founded by aging, so it’s possible that this is just a comingling of systemic disease with exfoliation syndrome—not a true association. To determine a connection more definitively, we
need prospective studies that can determine whether patients who are disease-free at baseline but end up getting cardiovascular disease are more likely to get exfoliation syndrome.
• Systolic blood pressure. One well-powered study conducted in India found that systolic blood pressure was indeed higher in patients with exfoliation syndrome, but it was not high enough to meet a definition of systemic hypertension.8
• Hearing loss. Although a number of studies have found some link between exfoliation syndrome and hearing loss, one recent study found no such association.9
 |
| Tortuous nailfold capillaries associated with exfoliation. |
• Homocysteine levels. Homo-cysteine levels are slightly higher in serum, aqueous humor and tears of exfoliation syndrome patients compared to healthy controls. How-ever, the largest study comparing homocysteine levels between patients with exfoliation syndrome and controls, done in India by Ashok Vardhan, DO, and colleagues, found no connection.8
This study, incidentally, was much larger than all of the other small studies relating to this put together. In fact, articles in the internal medicine literature are beginning to question whether the perceived association between homocysteine levels and cardiovascular disease is real.
• Pelvic organ prolapse. The Utah Population Database did find that exfoliation syndrome was more prevalent in women with pelvic organ prolapse, so it’s possible that such an association is valid.10
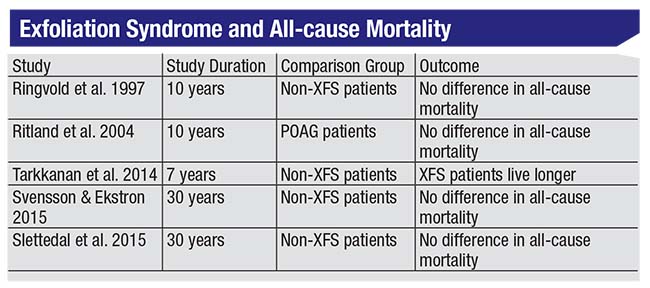
Perhaps most importantly, studies looking at the mortality of individuals with exfoliation syndrome don’t support the idea that they die earlier than healthy controls. (See table, above.) After all, if exfoliation syndrome is truly associated with conditions such as Alzheimer’s disease, cardiovascular disease or stroke, one would expect that it would also be associated with premature death. As it turns out, that’s not what the current literature shows. In fact, one of those studies actually concluded that exfoliation patients live longer than individuals without exfoliation.
Of course, the cited mortality studies have limitations. For example, all of them were done in Scandinavian countries, and they only evaluated exfoliation syndrome status at baseline; they didn’t update the status on an interim basis on follow-up. Nevertheless, if individuals who have exfoliation syndrome are more likely to die young, the evidence of that hasn’t shown up in the literature so far.
 |
No Reason for Concern—Yet
The bottom line is that although exfoliation materials are associated with elastic and collagen fibers throughout the body, no robust systemic association between exfoliation syndrome and other health issues has been confirmed by prospective studies. Yes, the literature has raised enough red flags to justify some concern, but a careful examination suggests that no real association has been demonstrated. It’s certainly possible that clear associations between exfoliation syndrome and systemic health issues may be found in the future; it’s just that more studies need to be done.
In the meantime, not every doctor managing exfoliative glaucoma worries about this—although I’ve heard doctors who have exfoliation syndrome themselves express concern about whether they should be checked for other health problems. For now, the evidence supporting such a connection is weak, and the most persuasive evidence that there isn’t any association between exfoliation syndrome and systemic disease may be that patients with exfoliation syndrome don’t appear to die prematurely.
So, when asked whether I believe that patients with exfoliation syndrome should have a systemic work-up of some kind, my answer is no—at least based on the evidence we have today. REVIEW
Dr. Pasquale is site chair of the Department of Ophthalmology at Mount Sinai Hospital in New York, and professor and system vice chair for translational ophthalmology research in the Department of Oph-thalmology at the Icahn School of Medicine at Mount Sinai. Dr. Pasquale is a consultant to Bausch + Lomb, Eyenovia and Verily; he has received NIH funding to study exfoliation syndrome.
1. Cousins CC, Kang JH, Bovee C, et al. Nailfold capillary morphology in exfoliation syndrome. Eye (Lond) 2017;31:5:698-707.
2. Cousins CC, Alosco ML, Cousins HC, et al. Nailfold capillary morphology in Alzheimer’s disease dementia. J Alzheimers Dis 2018;66:2:601-611.
3. Ritch R, Schlötzer-Schrehardt U. Exfoliation syndrome. Surv Ophthalmol 2001;45:4:265-315.
4. Janciauskiene S, Westin K, Grip O, Krakau T. Detection of Alzheimer peptides and chemokines in the aqueous humor. Eur J Ophthalmol 2011;21:1:104-11.
5. Abramsson A, Landgren S, Zetterberg M, et al. No association of LOXL1 gene polymorphisms with Alzheimer’s disease. Neuromolecular Med 2011;13:2:160-6.
6. Xu L, You QS, Wang YX, Jonas JB. Cognitive function and pseudoexfoliation syndrome. The Beijing Eye Study 2011. Br J Ophthalmol 2013;97:9:1215.
7. Aviv U, Ben Ner D, Sharif N, Gur Z, Achiron A. Pseudoexfoliation: An ocular finding with possible systemic implications. Isr Med Assoc J 2017;19:1:49-54.
8. Vardhan SA, ; Haripriya A, Ratukondla B; et al. Association of pseudoexfoliation with systemic vascular diseases in a South Indian population. JAMA Ophthalmol 2017;135:4:348-354.
9. Tryggvason G, Jonasson F, Cotch MF, et al. Hearing in older adults with exfoliation syndrome/exfoliation glaucoma or primary open-angle glaucoma. Acta Ophthalmol 2016;94:2:140-6.
10. Wirostko BM, Curtin K, Ritch R, et al. Risk for exfoliation syndrome in women with pelvic organ prolapse : A Utah Project on Exfoliation Syndrome (UPEXS) study. JAMA Ophthalmol 2016;134:11:1255-1262.



