ALTHOUGH NOT CONSIDERED A FIRST-line treatment for glaucoma, filtering surgery such as trabeculectomy is a common approach to lowering intraocular pressure when medications have failed to achieve a satisfactory result. However, once a bleb is created, late complications such as infections, bleb leaks or bleb failure can occur. These late problems may become more likely when antimetabolites such as mitomycin-C or 5-Fluorouracil are used during surgery.
Antimetabolites serve a positive purpose at the time of surgery: They inhibit fibroblasts—the cells that cause scarring. This reduces the likelihood that the bleb will completely heal and prevent the very filtration that the surgery was intended to provide. Unfortunately, mitomycin and 5-Fluorouracil are nondiscriminating poisons that also inhibit nearly all cells in the area, including immunological cells and epithelial cells. That means that the bleb has less resistance to infection and less ability to heal if a leak occurs. So using these agents is a double-edged sword: They improve the initial surgery success rate, but they increase the likelihood of problems later on.
I've encountered five late complications that can occur after filtering surgery: infection; leaks; bleb growth onto the cornea; interference with eyelid function; and bleb failure. Here, I'd like to share what I've learned about managing these complications when they occur, and offer some suggestions for titrating antimetabolites to minimize them.
A bleb infection is a potentially devastating complication. Following filtering surgery, three types of infection can occur. The first is an infection in the immediate postoperative period, which can happen with any eye surgery. This kind of endophthalmitis is rare—perhaps one out of every 500 or 1,000 surgeries.1
What's unique to glaucoma filtering surgery is the possibility of late endophthalmitis, which can occur at any time within five or 10 years of the surgery. The incidence of late infection in some studies is as high as 7 percent over a 10-year period—a pretty large number.
There are two levels of late infection. The first, blebitis, is localized at the bleb and is milder. Blebitis is heralded by pain, mildly reduced vision and red eye, which may be accompanied by a discharge. Left untreated, this infection can spread inside the eye, becoming full-blown endophthalmitis. Obviously, you want to recognize and treat the infection at the blebitis stage, when intensive topical antibiotics are usually sufficient to resolve the problem. If the infection spreads inside the eye, it requires much more intensive treatment: intraocular and intravenous antibiotics, and possibly vitrectomy and hospitalization. Once this has occurred you'll only have a 25-percent chance of rescuing the eye.
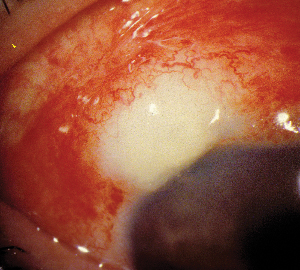 |
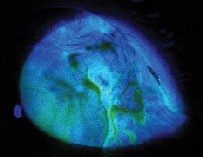
| A late case of blebitis (infection of the bleb); note the opalescent bleb and conjunctival hyperemia. In this case, there is no discharge. |
For this reason, I recommend giving these patients a flyer that tells them what signs to look for, and why they need to treat the appearance of symptoms like an emergency ... not to the point of panicking, of course, but to the point of being concerned enough to seek out ophthalmological care without delay. (As a result of taking this kind of precaution, not one of my patients who has developed blebitis in the last eight years has gone on to develop endophthalmitis.)
In terms of treatment, a third- or fourth-generation fluoroquinolone is probably the antibiotic of choice. Of course, if the problem is conjunctivitis, the cause could be viral rather than bacteriological, but if the patient has a filtering bleb it makes sense to err on the side of caution.
Bleb Leaks
Bleb leaks are another problem related to the use of antimetabolites. Factors such as dry eye can cause the eyelid to stick to the conjunctiva that covers the bleb and tear a tiny hole in it. When this happens, pressure usually drops significantly, ending up anywhere from 3 to 7 mmHg; that's one cue that the bleb may be leaking.
Bleb leaks can be serious for two reasons. First, a leak means the eye has increased susceptibility to infection. (Of course, if a leaky bleb is already infected, you have to treat the infection first.) Second, when IOP is extremely low for an extended period, fluid can form behind the retina, causing the choroid to move forward (choroidal detachment) and reduce vision. Some patients can actually bleed into that space, which can be devastating. Also, if the pressure is too low for too long, some patients may develop hypotony maculopathy.
If the bleb leak is small, I usually have the patient wear a bandage contact lens with topical gentamycin for a few weeks. If that doesn't work, I'll revise the site surgically by excising the necrotic tissue, undermining the remaining conjunctiva and pulling the more normal conjunctiva over the site. Of course, I could simply go directly to this alternative, but I find that patients are more receptive to surgical revision if I've given them a short trial of conservative therapy first.
Additional problems that can occur in the years following surgery include:
• Bleb enlargement. Occasionally, a bleb will enlarge and grow down onto the cornea, becoming a cosmetic or functional problem.This can occur any time in the first 10 or 15 years after surgery. If this occurs, I usually do nothing unless it starts to bother the patient, either cosmetically or in terms of irritation and discomfort. Then I excise the corneal portion of the bleb; often it's possible to do this and still preserve the filtration function of the bleb.
 |
 |
Fortunately, this is not a very common complication, but it can be very annoying for the patient.
• Interference with eyelid function. The eyelid is responsible for spreading tears evenly over the cornea. If a bleb becomes large enough and is close to the edge of the cornea, it may prevent the eyelid from pushing tears into the area of the cornea right below the bleb, creating corneal dellen. This can be irritating or even painful. Usually this problem can be managed by using artificial tears and lubricating drops. However, if the problem becomes severe, you may have to excise the bleb.
• Bleb failure. The body may heal the bleb over time, which is why the success rate of this surgery tends to drop after three to five years. You'll be able to tell this has happened because the patient's IOP will start to creep back up; an eye with a pressure of 12 mmHg after surgery may gradually rise to 14, then 17, then 20 mmHg. Or, you may be able to see that the bleb is scarring down.
When this happens, you can switch to topical pressure-lowering medications, try needling the bleb, or perform further surgery. Needling the bleb—using a needle underneath the bleb to try to break up the new scar tissue that has formed—is a simple in-office procedure that's often effective. If it is effective, pressure will drop immediately, and the bleb will enlarge. If it doesn't work the first time, I usually try a second time (although I won't try a third time).
If needling fails, depending on the patient's risk factors for failure of filtration, I may perform another trabeculectomy or insert a tube shunt to provide drainage.
Using Antimetabolites
Many of these late complications are enhanced by the use of intra-operative or immediately postoperative antifibrotics such as mitomycin-C or 5-Fluorouracil. They are a mixed blessing; if you don't use them at all, you'll have fewer complications, but the bleb is less likely to remain viable over the long run.
Because these drugs have the potential for promoting some complications, it's important to titrate their use depending on the likelihood of long-term success. We apply it using a cornea light shield made of methylcellulose, which doesn't fragment and absorbs a specific amount of the drug. (The standard cellulose sponges often used in surgery have a tendency to fall apart, and hold different amounts of the drug, depending on the manufacturer.) We position the sponge underneath the conjunctiva, over the sclera, for whatever time we've decided is appropriate. In the case of mitomycin, our standard maximum dose is 0.5 mg/ml, held in place for five minutes.
I use antimetabolites in the majority of my filtering surgeries, but I choose a dose appropriate to the patient's status. Unfortunately, this isn't always an easy decision to make. I'm likely to use the full dose described above if a patient is at high risk for bleb failure right from the start. This group would include younger patients, African Americans and patients with secondary glaucoma. If the patient has a lower risk of failure, as might be true for a much older patient, I use a lower dose and leave it in place for a shorter time. So, for example, if the patient is a 35-year-old African American with advanced glaucoma, I'd use the full 0.5 mg/ml for five minutes. If the patient is an 82-year-old Caucasian woman with moderate glaucoma who doesn't need her pressure lowered much, I might use 0.2 mg/ml for two minutes.
If you titrate your dosage you're less likely to get late side effects, but you probably won't be free of them. I just saw a 50-year-old Hispanic patient yesterday who underwent a trabeculectomy two years ago. Prior to this visit his IOP was fine, but now it had dropped from 14 to 3 mmHg. Sure enough, his bleb was leaking, although there was no sign of infection. I gave him a bandage contact lens, but I also scheduled him for surgery. I told him that if he comes back and the bleb has healed, we'll pop open a bottle of champagne and cancel the surgery.
Into the Future
As the science of glaucoma treatment progresses, alternatives to the use of antimetabolites will probably appear, and these kinds of late complications will become a thing of the past. Even the need for a surgical option may eventually disappear. But for now, we have to do our best to ensure that the options we offer our patients are effective, and that we—and the patient—are prepared to deal with complications, even if they occur many years later.
Dr. Stamper is a professor of clinical ophthalmology and director of the Glaucoma Service of the Department of Ophthalmology, University of California-San Francisco. He is the senior author of Becker-Shaffer's Diagnosis and Therapy of the Glaucomas, 7th edition, and has published more than 40 articles on glaucoma diagnosis, pharmacology and surgical treatment. He is a past president of the American Glaucoma Society.
1. Eifrig CW, Flynn HW Jr, Scott IU, Newton J. Acute-onset postoperative endophthalmitis: Review of incidence and visual outcomes (1995-2001). Ophthalmic Surg Lasers 2003;34:1:80.




