|
This article looks at the management of late hypotony in complicated blebs using a conjunctival pedicle flap technique.
Background
Trabeculectomies can fail due to fibrosis of the conjunctiva and Tenon's capsule. Since the early 1990s the apparent enhanced surgical success associated with the use of intraoperative adjuvant mitomycin-C has led to a rapid gain in its popularity.
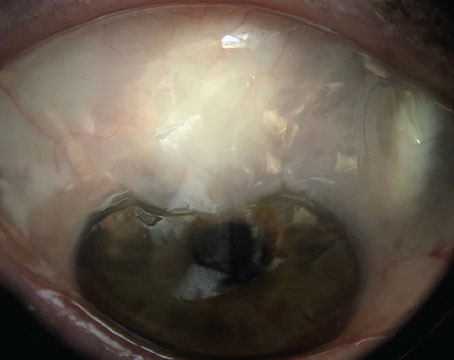
Mitomycin-C is much more potent than 5-fluorouracil, promotes fibroblast apoptosis, inhibits vascular proliferation, may cause atrophy of the ciliary body, and is toxic to the corneal endothelium. The potency of MMC has resulted in a virtual epidemic of extremely thin filtering blebs. In many cases it has become difficult to determine whether the patient has a slight bleb leak or simply rapid transudation of fluid. Intraocular pressures in the single digits are much more common since trabeculectomy with MMC became popular.
|
I participated in a recent retrospective review of primary trabeculectomy with MMC which included 123 eyes with a minimum five-year follow-up. Mean IOP was approximately 9 mmHg. Excluding those with bleb leaks, 42 percent of eyes had an IOP at least six months postoperative of less than 6 mmHg at a mean of 26 months after surgery.
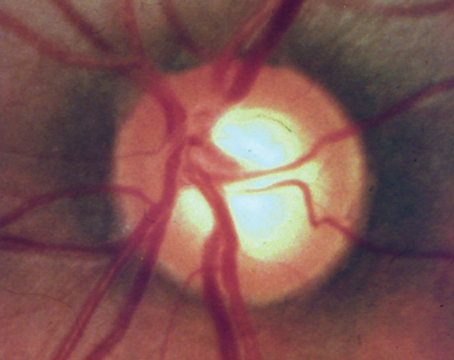
In addition, 9 percent of patients had hypotony maculopathy, consistent with other reports in the literature. Interestingly, new cases of hypotony continued to develop as long as five years after the initial surgery. The study found no correlation between MMC concentration or exposure time and the development of hypotony.
The single greatest predictor for the development of late hypotony was a low IOP at one month post operative (p<0.05). The study found no correlation between MMC concentration or exposure time and the development of hypotony. Blood injection was attempted in some patients, but the majority required surgical intervention to reverse the hypotony.
The success of autologous blood injection in reversing hypotony and the associated visual dysfunction appears to be less than 50 percent at two years. As a result, resuturing of the scleral flap or scleral reinforcement with a patch graft is usually necessary to manage this problem. Depending on the integrity of the bleb, conjunctivoplasty is often integral in late hypotony and bleb leak intervention.
When evaluating hypotony preoperatively, anatomical and functional status should direct the surgical approach. I advocate the following guidelines:
• When there is hypotony only in the presence of a bleb leak, conjunctival grafting is indicated.
• For hypotony with robust conjunctiva and no history of bleb leak or infection, consider scleral reinforcement that preserves the original bleb.
• For hypotony and a thin ischemic or intermittently leaking bleb, or history of bleb infection, use scleral reinforcement plus conjunctivoplasty.
Scleral Reinforcement
Surgical treatment for hypotony is indicated in patients with decreasing visual acuity, macular or choroidal folds, or variable refractive error that is not well-tolerated. Though older patients may tolerate hypotony well with stable visual function, a temporarily above-average intraocular pressure appears to be important in reversing visual loss from hypotony maculopathy, particularly in younger patients.
Therefore, when performing scleral re-suturing or patch grafting, placing one set of sutures to approximate the final "target" intraocular pressure and a second set of "tight" sutures to produce a temporary, substantial increase in pressure allows for delayed suture lysis of tight sutures once symptoms of hypotony have resolved.
The greatest concern in patients in whom scleral reinforcement is performed is a return to uncontrolled glaucoma. A retrospective analysis was performed at our center to evaluate postoperative results after scleral reinforcement for late hypotony in 22 eyes (Scleral reinforcement surgery for late hypotony after trabeculectomy with MMC. Bindlish, Condon, et al. Poster, American Academy of Ophthalmology 2000, Dallas).
Patients had initially undergone MMC trabeculectomy, and mean follow-up was two years. All patients had symptomatic visual dysfunction, 82 percent were primary trabeculectomy patients, 72 percent had maculopathy prior to surgery, 41 percent had concurrent bleb leaks, and 55 percent had received autologous blood injections. One year after surgery, mean intraocular pressure was 12 mmHg, 77 percent had a mean increase in visual acuity of almost four lines, 73 percent were using no glaucoma medications at the last follow up, and 9 percent required additional surgery for uncontrolled glaucoma.
Conjunctivoplasty
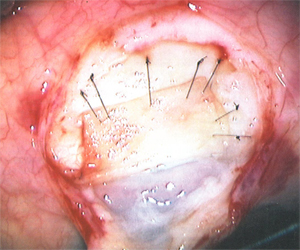
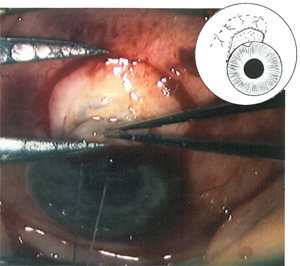
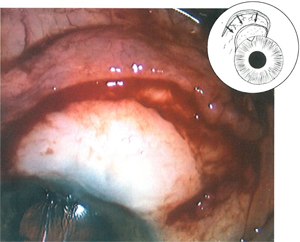
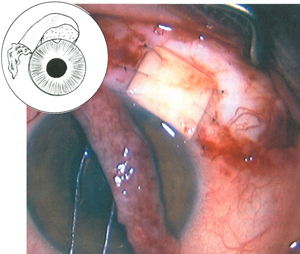
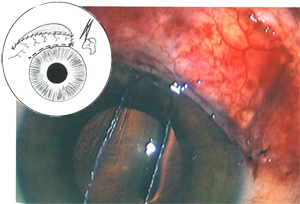
Effective approaches described to resurface a leaking bleb or a scleral graft include either a free autograft or simple conjunctival advancement with or without a relaxing incision. The technique of rotating a conjunctival pedicle flap appears to have some potential advantages including the ability to manage large blebs, maintain a blood supply and minimize ptosis. In cases where a bleb leak dictates only a conjunctivoplasty, removing the existing bleb epithelium—while preserving rather than excising the underlying bleb architecture—may allow better long-term control of intraocular pressure.
With the pervasive use of mitomycin C, surgical intervention for hypotony and bleb leak is becoming increasingly common. Fortunately, operative results are encouraging, but filtration failure remains the major concern with intervention. REVIEW
Dr. Condon is an associate professor of ophthalmology at Drexel University College of Medicine, Allegheny General Hospital, Pittsburgh.
1. O'Connor DJ, Tressler CS, et al. A surgical method to repair leaking filtering blebs. Ophthalmic Surg 1992;23:336.
2. Budenz DL, Chen PP, et al. Conjunctival advancement for late-onset filtering bleb leaks: indications and outcomes. Arch Ophthalmol 1999;117:1014.
3. Morris DA, Ramocki JM, et al. Use of autologous Tenon"s capsule and scleral patch grafts for repair of excessively draining fistulas with leaking filtering blebs. J Glaucoma 1998;7:417.
4. Harris LD, Yang G, et al. Autologous conjunctival resurfacing of leaking filtering blebs. Ophthalmology 2000;107:1675
5. Wadhwani RA, Bellows AR, et al. Surgical repair of leaking filtering blebs. Ophthalmology 2000;107:1681.
6. Bindlish R, Condon GP, et al. Efficacy and safety of mitomycin-C in primary trabeculectomy: five-year follow-up. Ophthalmology 2002;109:1336.
7. Burnstein AL, WuDunn D, et al. Conjunctival advancement versus nonincisional treatment for late-onset glaucoma filtering bleb leaks. Ophthalmology 2002;109:71.