Gonioscopy-assisted transluminal trabeculotomy is a MIGS procedure that increases aqueous outflow by removing the trabecular meshwork and the inner wall of Schlemm’s canal. In moderate to advanced open-angle glaucoma, it has a reported success rate of 83.7 percent.1 One of the biggest benefits of GATT is that it’s a cost-effective option when using Prolene suture and other equipment that’s already in the OR.
Here, I’ll describe how to perform GATT using the suture technique and share pearls for success.
Patient Selection
Adults and children2 with open-angle glaucomas are ideal candidates for the GATT procedure, though GATT is safe and effective for both primary and secondary open-angle and angle-closure glaucomas as well.3 GATT can be employed in all stages of glaucoma since it treats the entire collector system. Studies have also shown that GATT is an option for patients who’ve already undergone filtering procedures such as trabeculectomy and tube shunt implantation, with reported success rates ranging from 60 to 70 percent.4 GATT is contraindicated in patients with unidentifiable angle structures, intraocular lens instability, those who can’t stop anticoagulant medication and those with corneal endothelial disease.
For surgeons who are new to GATT, selecting the right patients for the first few procedures will set you up for success. Those who have secondary open-angle glaucomas such as pseudoexfoliation, pigment dispersion or pigmentary glaucoma are good options. The reason for this is that when you’re first working in the angle, it can be difficult to visualize the structures, so having some of the pigment present as a landmark for identifying the trabecular meshwork is helpful. Using trypan blue to stain the trabecular meshwork can also aid visualization and identification of the angle layers.
Before attempting GATT, it’s a good idea to have some experience with other angle-based surgeries that might not involve cannulating the entire canal, such as iStent or Kahook dual blade goniotomy, in order to get familiar with working in the angle. Try performing intraoperative goniotomy on all your cataract patients to get used to using the gonioprism and obtaining an en face view of the angle.
 |
| Figure 1. In this combined GATT-phaco case performed by Ali Al-Beshri, MD, phaco is performed first, followed by GATT. A microcatheter is placed using an ab interno approach to unroof Schlemm’s canal for a full 360 degrees. Photo: All Images: Uday Devgan, MD (CataractCoach.com). |
Surgical Technique
I perform GATT using 5-0 Prolene most of the time because it’s cost effective. If using Prolene suture, it must first be prepared using low-temperature cautery to blunt the ends of the suture. The microcatheter technique is very similar, though these devices don’t require priming and have an illuminated, blinking tip to help the surgeon track its progress through the canal (Figure 1). The canaloplasty device iTrack is often used off-label for GATT.
Begin by making a clear corneal paracentesis directly across from the nasal meshwork. Fill the anterior chamber with viscoelastic such as Healon GV and rotate the eye on the gonioprism to visualize the angle. Direct visualization is one of the first steps in any angle-based surgery. So, if you don’t have a clear en face view—stop and try to get better visualization. Don’t press too hard on the gonio prism to avoid creating corneal striae.
I use a 25-gauge MVR blade to make a 1- to 2-mm goniotomy in the nasal quadrant. Before inserting the prepared suture, I inject a little more viscoelastic at the goniotomy site to further open up the area so that the suture has an easier point of entry.
At the goniotomy site, insert the suture at a 10- to 15-degree angle to ease entry into the lumen of Schlemm’s canal (Figure 2A). It’s important to confirm that you’re in the correct space before starting to cannulate, especially when using suture because even though it’s blue, it’s often more difficult to see than a microcatheter. You certainly don’t want to be in the ciliary body or create a cyclodialysis cleft for 360 degrees. Advance the suture slowly, about one clock hour at a time, in a counterclockwise direction for right eyes; clockwise for left eyes.
When the distal end of the suture returns to the initial goniotomy site (Figure 2B), grasp it together with the proximal end using microforceps and pull to unroof the trabecular meshwork (Figure 2C). As you tear through the trabecular meshwork, there will be some blood reflux. At the end of the case, leave some Healon in the eye to tamponade the bleeding (Figure 2D). The amount left will depend on the amount of blood reflux from the episcleral veins. If I see a lot of blood reflux, I’ll leave as much as half of the Healon in the eye, and the pressure may be closer to 20 or 30 mmHg at that time. If there’s minimal blood reflux, I leave less viscoelastic. The target pressures on the first day after surgery may range from 15 to 18 mmHg.
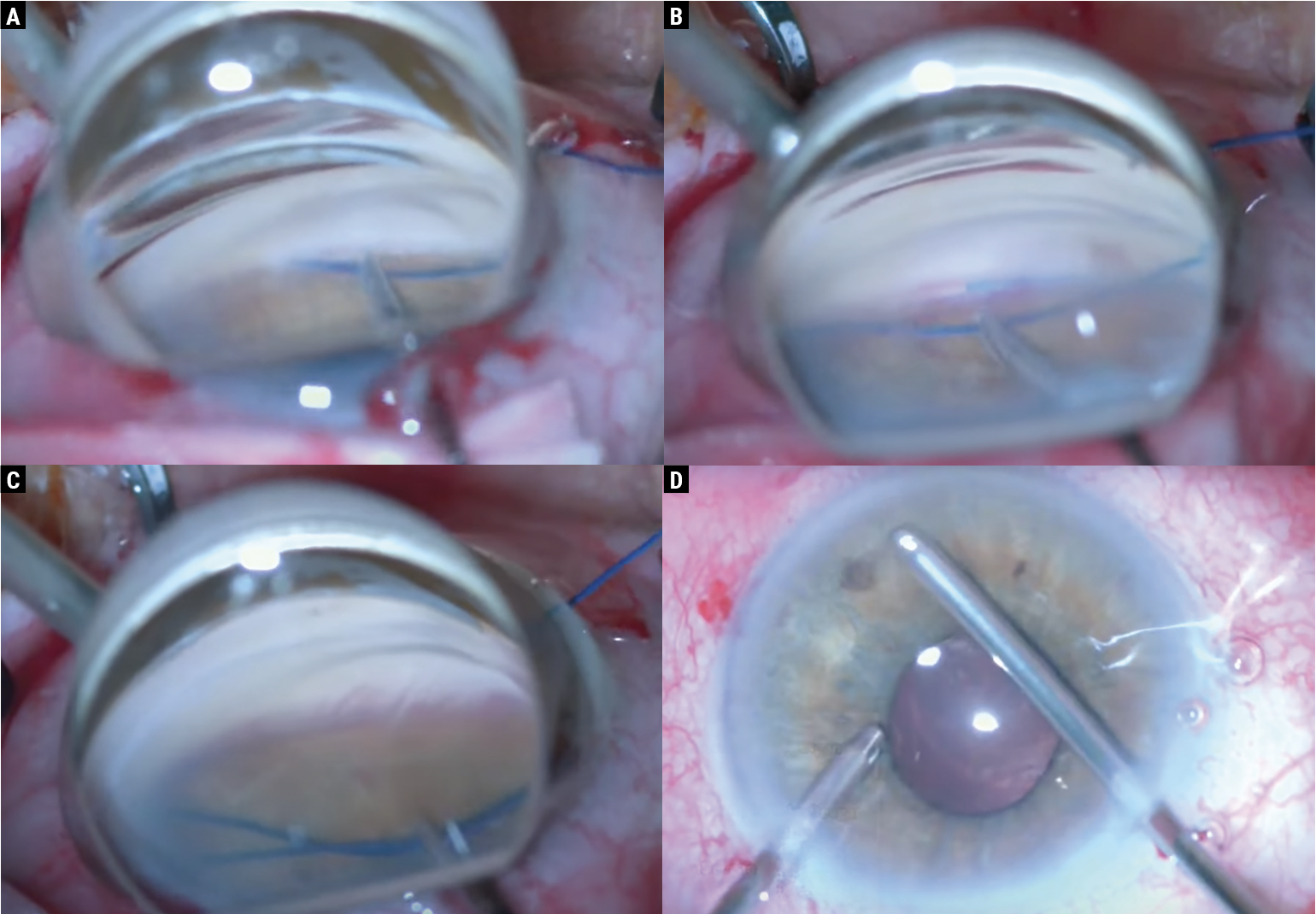 |
| Figure 2. (A) In this case, performed by Val Apostolov, MD, a patient with secondary uveitic glaucoma underwent GATT using the suture technique, followed by phacoemulsification. Combining phaco with GATT helps to provide additional pressure lowering, since crystalline lens removal opens the angle. Here, the blunted 5-0 polypropylene suture is inserted gently into the goniotomy incision at a slightly upward angle. (B) The suture is passed through Schlemm’s canal for a full 360 degrees, advancing slowly by about one clock hour at a time. (C) Using microforceps, both ends of the suture are grasped and pulled to unroof the trabecular meshwork. (D) Some viscoelastic is aspirated out of the anterior chamber. Leave a fill of 25 to 50 percent as a tamponade, depending on the amount of blood reflux present. Photo: Ahmad Aref, MD, MBA. |
Around the Globe
A 360-degree GATT is considered ideal since it treats the entire collector system; currently, we can’t easily identify the key areas where the collector channels are most robust. However, it’s not always possible to achieve a 360-degree GATT. If you meet considerable resistance, rather than attempting to shove the suture or microcatheter, cannulate what you can and tear through. A 200- to 270-degree GATT is often sufficient.
Hemi-GATT paired with cataract surgery has also been described in the literature. In one study, 180-degree cannulation of the inferior hemisphere was performed in 112 eyes of 112 patients with moderate to severe primary open-angle glaucoma, resulting in an IOP reduction of 37.9 percent (13.6 ±3.9 mmHg at 24 months) from a baseline of 21.9 ±5.8 mmHg.5
Postoperative Pressures
Pressure reduction after GATT is best evaluated about one week postoperatively. Take the initial IOP drop the day after the case with a grain of salt. On postop day one, patients may have good eye pressures because their glaucoma medications may not have washed out of their systems. It’s closer to the one-week mark where you can assess whether or not the procedure was successful. Certainly, for those times when the pressure is higher than expected, perform gonioscopy at the slit lamp to see the areas that have been cannulated and check whether there’s a clot or something else prohibiting the pressure from dropping more.
Intraocular pressure spikes are common after GATT and are most likely to occur within the first two weeks.6 Though they resolve with topical and systemic pressure-lowering treatments, pressure spikes are a risk factor for GATT failure. If IOP spikes occur due to postoperative topical steroid use, steroids should be discontinued in favor of an NSAID.
Dr. Zhang is a clinical associate professor of ophthalmology and visual sciences at the Kellogg Eye Center at the University of Michigan. She has no related financial disclosures.
1. Aktas Z, Ucgul AY, Bektas C, Karamert SS. Surgical outcomes of Prolene gonioscopy-assisted transluminal trabeculotomy in patients with moderate to advanced open-angle glaucoma. J Glaucoma 2019;28:10:884-888.
2. Shi Y, Wang H, Oatts JT, et al. A prospective study of intraocular pressure spike and failure after gonioscopy-assisted transluminal trabeculotomy in juvenile open-angle glaucoma: A prospective study of GATT in JOAG. Am J Ophthalmol 2022;236;79-88.
3. Aboalazayem F, Elhusseiny AM, El Sayed YM. Gonioscopy-assisted transluminal trabeculotomy: A review. Curr Eye Res 2023;48;4:329-338.
4. Grover DS, Godfrey DG, Smith O, et al. Outcomes of gonioscopy-assisted transluminal trabeculotomy (GATT) in eyues with prior incisional glaucoma surgery. J Glaucoma 2017;26:1:41-45.
5. Ruparelia S, Wilson D, Shoham-Hazon N. Hemi-GATT combined with phacoemulsification in patients with moderate-severe primary open-angle glaucoma: 2-year outcomes. Graefes Arch Clin Exp Ophthalmol 2023;261:11:3257-3262.
6. Naftali Ben Haim L, Yehezkeli V, Hollander EA, et al. Intraocular pressure spikes after gonioscopy-assisted transluminal trabeculotomy (GATT). Graefes Arch Clin Exp Ophthalmol 2024;262;3;927-935.




